Have you ever wondered if there’s a more direct way to tackle elevated eye pressure (IOP) by targeting the natural drainage pathways, rather than just slowing fluid production? Rhopressa provides exactly that opportunity. This once-daily eye drop is specifically formulated to increase aqueous humor outflow, which helps reduce the load on your optic nerve. Instead of taking a broad approach or relying solely on older classes of pressure-lowering medications, Rhopressa zeroes in on the trabecular meshwork—one of the eye’s main outflow routes. By encouraging better fluid drainage, it aims to stabilize or reduce IOP levels in patients who are managing glaucoma or ocular hypertension.
One exciting aspect of Rhopressa is how it harnesses Rho kinase inhibition to soften tissues within the drainage structures. Traditional medications often focus on slowing aqueous fluid production or diverting fluid through less conventional pathways. In contrast, Rhopressa primarily makes it easier for the fluid to exit exactly where it’s meant to. This emphasis on outflow sets the stage for a distinctive treatment option that could blend well with other drops—or in some instances, even serve on its own. Below, you’ll get an up-close view of how Rhopressa works, how doctors integrate it into therapy, the supporting research behind its development, and what to expect in terms of safety and pricing.
How Rhopressa Brings a Modern Approach to Eye Pressure Management
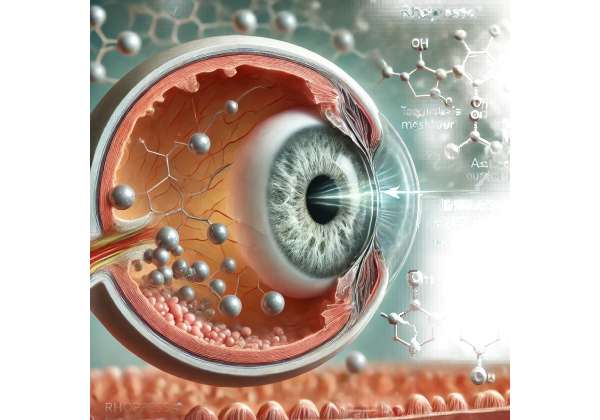
Rhopressa’s place in the glaucoma treatment landscape represents a breakthrough in targeted pharmacology, especially in how it interacts with the eye’s natural drainage mechanisms. While earlier glaucoma medications leaned heavily on reducing fluid production from the ciliary body or improving drainage through alternate channels, Rhopressa’s uniqueness arises from directly relaxing the trabecular meshwork (TM).
Shifting the Paradigm to Outflow Enhancement
Intraocular pressure fluctuates based on how much aqueous humor the eye produces versus how effectively it drains. When drainage lags behind production, pressure spikes, placing strain on the optic nerve. Prostaglandin analogs typically open the uveoscleral pathway, and beta-blockers reduce fluid generation in the ciliary body. Rhopressa, however, takes a fresh route:
- Trabecular Focus: By targeting the TM, the medication addresses the primary path through which around 80% of fluid exits. This is a more physiologic approach, leveraging the main drainage route rather than a workaround.
- Rho Kinase Inhibition: The active molecule in Rhopressa blocks Rho kinase, an enzyme that can stiffen cells within the TM. When Rho kinase activity is diminished, tissues relax and create less resistance to fluid flow.
In many ways, this parallels the concept of vasodilators in blood pressure management: by reducing stiffness or narrowing, you allow fluid to pass with fewer constraints. This fosters a potential synergy with older treatments, since each agent addresses a different aspect of fluid dynamics in the eye.
Why Rho Kinase Matters in Glaucoma
Rho kinase (ROCK) plays pivotal roles across various body systems, influencing how cells contract and maintain shape. Inside the eye, ROCK’s presence in the trabecular meshwork has two important consequences:
- Altered Cytoskeleton: ROCK boosts actin stress fibers, making cells contract. If these cells remain tense, they tighten the TM, hindering outflow and possibly escalating eye pressure.
- Possible Effects on Blood Flow: Some studies suggest that Rho kinase might also have indirect effects on ocular perfusion, though the clinical significance is still being explored. Reduced ROCK activity might improve local blood circulation or help protect ocular tissues from stress.
When the TM is overly stiff, the fluid meets more friction and drains less efficiently. That leads to a net pressure increase. Rhopressa downshifts this tension, paving the way for more fluid to exit. The concept might sound basic, but it’s a key leap forward because it zeroes in on a fundamental mechanical process long recognized in glaucoma but rarely targeted in earlier drug classes.
Advantages Over Traditional First-Line Therapies
Beta-blockers (e.g., timolol) and prostaglandin analogs (e.g., latanoprost) have historically been first-line treatments. They can deliver robust IOP reduction but also have limitations:
- Systemic Impact: Beta-blockers may lower blood pressure or aggravate certain respiratory conditions.
- Tachyphylaxis: Over time, some individuals see diminishing returns from repeated beta-blocker use.
- Pigment Changes: Prostaglandins can darken the iris and eyelid skin, or cause eyelashes to grow in unintended ways.
Rhopressa sidesteps many of these issues by focusing on the TM. While it can cause mild eye redness and some other localized effects, it does not typically carry systemic cardiovascular or respiratory implications. In practice, doctors often weigh these considerations when deciding on an initial or add-on medication. For patients with mild to moderate glaucoma—particularly those who haven’t responded fully to older drops—Rhopressa can be a logical next step.
Addressing Disease Progression
A significant aspect of open-angle glaucoma is the slow, insidious rise in eye pressure and progressive optic nerve damage. If the TM degenerates or stiffens over time, fluid outflow diminishes, gradually intensifying mechanical stress on nerve fibers. By inhibiting Rho kinase:
- Improved Drainage: Over an extended period, consistent TM relaxation could help keep IOP in a safer range, potentially slowing optic nerve damage.
- Enhancing TM Health: Some researchers hypothesize that healthier outflow channels might reduce the risk of further structural damage.
- Broader Protective Mechanisms: Preliminary data suggests that Rho kinase inhibitors might have protective roles for retinal ganglion cells in certain laboratory settings, though this is still an area of active inquiry.
While any promise of direct neuroprotection remains tentative, the key advantage is that daily use of Rhopressa can help ensure stable pressure, a cornerstone in preserving sight. When doctors talk about long-term management, it isn’t just about achieving an immediate drop in IOP—it’s about maintaining that reduction day after day to safeguard the optic nerve from slow attrition.
Combining with Existing Regimens
Glaucoma regimens can become complex, especially as the disease progresses. Patients might be on multiple medications or rotating through different classes. Rho kinase inhibition can neatly fit into that puzzle:
- Add-On Therapy: If someone’s IOP remains above target, introducing Rhopressa alongside a prostaglandin or beta-blocker can yield an additional reduction. Studies show that synergy often occurs because the mechanisms complement one another.
- Single-Agent Option: For mild cases, or for those intolerant to other drops, Rhopressa alone could suffice. The once-daily dosing fosters compliance, a crucial factor for success.
Either route depends on personalized assessments. Some individuals might do well with a single agent, while others require multiple lines of defense. The consistent thread is that Rhopressa taps an underused method—optimizing outflow at the TM—to offer a new dimension in treatment.
Remaining Challenges and Outlook
Though widely embraced by many eye care professionals, Rho kinase inhibitors aren’t an absolute fix-all. A subset of patients might experience side effects like ocular surface irritation or may require multiple medications to hit their IOP targets. That said, the therapy’s novel approach inspires optimism that we can refine how we address ocular hypertension. Ongoing research into advanced formulations or combination drops could reduce daily burden or lessen side effects. Meanwhile, the distinct mechanism continues to open fresh avenues for investigation into how best to preserve the optic nerve over a lifetime.
For now, Rhopressa provides a modern twist on a longstanding objective: keep IOP as low as safely possible, using therapies that respect the eye’s normal fluid dynamics. This focus on physiologically relevant outflow could be the blueprint for future therapies that similarly hone in on specific, local processes. With Rhopressa, many doctors and patients feel there’s finally an outflow-centric option robust enough to stand shoulder to shoulder with established classes of glaucoma medications.
Practical Steps for Using Rhopressa Each Day
Navigating a new eye drop often comes with questions about how it fits into your daily routine and other medications. Although Rhopressa is typically straightforward—once-daily dosing is a key convenience—there are recommended strategies and cautions worth understanding to maximize comfort and results.
Typical Dosing Schedule
Rhopressa is prescribed as a one-drop-per-day regimen in the affected eye(s). Many clinicians suggest bedtime instillation for two main reasons:
- Nighttime Tolerance: If mild redness or irritation occurs, a patient may not notice it as much while sleeping.
- Consistent Routine: It’s usually easier to remember a nightly schedule, reducing the likelihood of missed doses.
If an individual occasionally forgets a dose, the next step is to administer it as soon as they recall, then revert to the standard evening schedule. Double-dosing to “catch up” is not advisable, as it can raise the risk of local side effects.
Correct Technique for Eye Drop Application
Getting that single drop onto the eye surface might sound easy, but technique matters:
- Hand Hygiene: Start by washing your hands thoroughly. This step helps avoid contaminating the bottle tip or your eye.
- Head Tilting: Tilt your head back slightly and look upward, or lie down if that’s more comfortable.
- Form a Pocket: Use one finger to pull down the lower eyelid, creating a small pocket where the drop can rest.
- Release the Drop: Carefully squeeze one drop of Rhopressa into the pocket.
- Close Gently: After the drop lands, shut the eye for up to 2 minutes without blinking too vigorously. This helps the medication stay in contact with the eye surface.
- Avoid Contact: Try not to let the bottle tip touch your eyelashes or eyelid, which can lead to contamination.
Because the dose is small, it’s easy for some of the liquid to slip out if a person blinks heavily. Eye care providers often advise people to gently blot away any excess with a clean tissue—without applying pressure to the eye. By practicing a calm, measured application technique, the medication can disperse across the cornea effectively.
What to Expect Initially
After the first few doses, some individuals might notice mild stinging or blurring. Such sensations typically fade within moments. Slight redness (hyperemia) can also appear, especially in the early weeks of use. This effect often diminishes as the eye adapts. If discomfort persists or feels significant, it’s wise to inform the prescribing doctor, who may suggest using lubricating drops or adjusting the routine.
Handling Other Medications
It’s common for patients to juggle multiple eye medications, whether it’s for glaucoma or other conditions. When combining Rhopressa with additional drops:
- Time Spacing: Wait at least 5-10 minutes between different eye products to prevent dilution or washout of the first medication.
- Order: Some doctors recommend administering watery solutions before more viscous or gel-based drops. This helps each drop make full contact.
- Tracking: Keeping a chart or alarm can help manage multiple medications, ensuring none are skipped or overlapped improperly.
Doctors sometimes adjust the schedule so that one drop is used in the morning and Rhopressa in the evening, which can simplify adherence. Over time, as IOP stabilizes, the specialist might decide if a second medication can be discontinued—though this depends on how well each agent is controlling pressure.
Refill Logistics and Storage
Rhopressa is commonly dispensed in small bottles. Storing them at room temperature in a clean, dry place is typically suitable, but always confirm the package insert for specific guidelines. If the supply runs low, the person should request a refill promptly to maintain continuous therapy. Even short lapses can let IOP creep back up. Many health insurance plans allow early refills, ensuring you always have medication on hand.
Monitoring and Follow-Up
No matter how effective a medication is, ongoing follow-up remains crucial in glaucoma management. During regular check-ups, doctors measure IOP to confirm whether Rhopressa is achieving the target pressure. They may also:
- Examine the Optic Nerve: Using tools like optic nerve photos, scanning laser ophthalmoscopy, or optical coherence tomography (OCT) to watch for subtle changes.
- Assess Visual Fields: Checking peripheral vision can spot any progression that might not be evident solely by IOP readings.
- Tweak the Treatment Plan: If the pressure hasn’t decreased enough, the regimen might be expanded or adjusted. Alternatively, if the patient experiences side effects, a different approach could be explored.
Adapting to Lifestyle
Although eye drops don’t typically disrupt daily routines significantly, certain factors can help maintain ocular comfort. For instance, staying hydrated, avoiding smoky or overly dry environments, and using humidifiers can keep the eye surface from feeling irritated. Some individuals also choose to limit caffeine or smoking, as these may impact vascular function and, indirectly, eye pressure.
With consistent, proper use, many find that Rhopressa effectively fits into their daily life. The therapy’s reliance on an outflow mechanism can deliver a sense of empowerment: rather than just reducing fluid generation, it actively fosters a more open, healthy drainage path within the eye. This synergy between an easy dosing schedule and direct mechanical relief is at the heart of Rhopressa’s appeal for many doctors and patients looking for straightforward solutions.
Recent Findings and Investigations on Rhopressa
From large-scale clinical trials to real-world observational studies, the development of Rhopressa (netarsudil ophthalmic solution) has come with a considerable amount of research scrutiny. Unlike older agents that were introduced decades ago, Rho kinase inhibitors underwent rigorous testing to prove their effectiveness and safety before reaching pharmacies. Below is a closer look at some of the key data shaping medical opinions on this therapy.
Foundational Trials Establishing Efficacy
Initial trials—often referred to as Rocket 1, Rocket 2, and Rocket 3—laid the groundwork for regulatory approvals in multiple countries. These studies enrolled participants with open-angle glaucoma or ocular hypertension, comparing once-daily Rhopressa to established treatments like timolol, a beta-blocker commonly used as a reference standard.
- IOP Reductions: In these pivotal trials, Rhopressa proved non-inferior to timolol in participants whose baseline IOP wasn’t exceedingly high (often around the low to mid-20s mmHg). Patients saw average drops of 3-5 mmHg from baseline over the initial 3 months.
- Durability: Across longer extensions (up to 12 months), the results remained consistent, indicating that Rhopressa’s effect didn’t wane with time.
- Side Effect Profiles: Mild to moderate conjunctival hyperemia was the most commonly reported adverse event, echoing earlier preclinical work. This redness improved or stabilized in many patients who continued the medication over time.
These findings garnered enough confidence for authorities like the FDA to give Rhopressa the green light as a daily therapy for elevated IOP. They also established a viable place for Rho kinase inhibition among other first-line or second-line treatments.
Comparative Insights with Prostaglandin Analogs
While the initial tests pitted Rhopressa mostly against timolol, follow-up studies and smaller observational reports examined how it matches up to prostaglandins (e.g., latanoprost, bimatoprost). Prostaglandins have been a mainstay for many years, so any new therapy must hold its own in such comparisons:
- Efficacy Range: Prostaglandins remain some of the most potent IOP-lowering agents, often hitting reductions of 6-8 mmHg or more. Rhopressa’s typical effect is slightly less on average, especially if the baseline pressure is very high.
- Mechanistic Benefits: In eyes with moderately elevated IOP or in patients who do not respond well to prostaglandins, Rho kinase inhibitors can offer a unique complementary effect.
- Adverse Event Differences: Whereas prostaglandins may cause lash growth or iris color changes, Rhopressa’s main side effects revolve around the ocular surface, such as mild stinging or redness.
The net conclusion from these analyses: while a prostaglandin might still be tried first in many cases, Rhopressa can either replace or augment it, depending on patient-specific responses and tolerance.
Synergistic Effects in Combination
One of the more promising areas of research has been exploring how well Rhopressa performs when added to someone’s existing medication regimen. Because it relaxes the trabecular meshwork, it addresses a different mechanism than, say, alpha agonists or carbonic anhydrase inhibitors, which reduce fluid production. Preliminary data suggests that:
- Add-On Gains: In patients already using a prostaglandin analog but still showing unsatisfactory IOP control, layering Rhopressa resulted in an additional drop of 2-4 mmHg in many participants.
- Reduced Need for Third Agent: Some individuals who might otherwise require a third or fourth medication found that switching to or including Rhopressa maintained target pressures with fewer total drops.
Clinicians highlight the convenience factor—if a patient can accomplish better control with one daily Rhopressa dose plus another agent, rather than juggling multiple new drops, adherence typically improves. This synergy could potentially shape treatment guidelines in the future, making Rho kinase inhibition a top consideration in combination strategies.
Observational Data in Everyday Practice
Beyond the confines of strictly controlled trials, real-world usage reports are beginning to trickle in. These typically involve local clinic audits, retrospective reviews, or physician questionnaires that capture how Rhopressa works in routine settings:
- Sustained Pressure Lowering: The majority of patients who adhere to the once-daily regimen maintain stable IOP at follow-up appointments, with average reductions aligning closely with the original trial data.
- Hyperemia Management: Some practices note that around 10-15% of users report persistent redness or discomfort enough to consider changing medications. However, a significant proportion adapt within the first 6-8 weeks.
- Favorable for Early Intervention: Doctors mention prescribing Rhopressa earlier in the disease course, particularly for younger patients who prefer a once-daily schedule and want to avoid potential systemic side effects from other classes.
In general, these real-world insights confirm the medication’s role as a valuable alternative or companion to older drug classes. They also highlight the importance of patient education about potential, but often transient, redness or mild irritation.
Investigations Into Neuroprotection
Rho kinase’s involvement in cell survival, neuronal growth, and blood flow regulation has spurred a wave of basic science studies to see if inhibitors like netarsudil (the key ingredient in Rhopressa) might shield the optic nerve from damage. Early lab experiments on animal models hinted at potential neuroprotective effects under certain stress conditions. However, translating these findings to humans remains complex. Ongoing clinical trials or prospective observational studies would be required to prove any direct nerve-sparing effect in glaucoma patients.
That said, even a mild improvement in perfusion around the optic nerve could be beneficial, if verified. For the moment, clinicians remain cautious, focusing on the established outflow advantages as the main reason to prescribe Rhopressa. If future data confirm significant neuroprotective properties, it could reshape how doctors prioritize Rho kinase inhibitors in the broader treatment algorithm.
Future Directions and Unanswered Questions
As more patients adopt Rhopressa, additional studies are looking to:
- Identify Ideal Candidates: Which subgroups of glaucoma or ocular hypertension patients do best on Rho kinase inhibition?
- Refine Dosing: Though once-daily is the standard, might some patients benefit from a different schedule or a combination drop that merges netarsudil with a prostaglandin or other agents?
- Assess Long-Term Safety: While the year-long data is reassuring, decades-long follow-ups will reveal if any rare complications arise or if ocular surface tolerance shifts.
Some pharmaceutical research also explores extended-release formats, such as sustained implants or micro-dosing contact lenses, to deliver netarsudil in a more controlled manner. These approaches could further reduce the daily burden on individuals who struggle with drops or have dexterity challenges.
Altogether, the scientific landscape around Rhopressa is dynamic, balancing well-documented trial evidence with real-world experiences. For doctors who want a direct outflow method or for patients seeking an alternative to older medications, these findings underscore Rho kinase inhibition as a legitimate, forward-thinking option in the ongoing fight against vision loss from glaucoma.
Measuring Efficacy and Addressing Potential Side Effects
Rhopressa has garnered praise for its ability to reduce intraocular pressure by targeting the trabecular meshwork. Clinical data consistently show pressure drops comparable to certain established medications, especially in patients with moderate baseline IOP. Many achieve and maintain target pressures with once-daily application, which simplifies compliance.
Still, no eye drop is entirely free of side effects. With Rhopressa, one of the most commonly noted issues is mild to moderate redness (hyperemia). This side effect can appear more frequently in the first few weeks, often lessening with continued use. Other possible complaints include slight stinging, blurred vision immediately after application, or dryness around the eyes. Serious complications remain rare, but anyone experiencing a marked or persistent discomfort should consult their ophthalmologist. Meanwhile, systemic side effects appear minimal, given the localized nature of the treatment and relatively low absorption beyond the eye.
When evaluating results, doctors generally look for consistent IOP readings in the target range without progressive damage to the optic nerve. If necessary, adjusting the regimen—whether by adding a second medication, changing the time of administration, or exploring alternative solutions—can help refine therapy. In real-world practice, Rhopressa is viewed as having a favorable overall safety profile, making it a compelling addition to current glaucoma interventions.
Costs and Availability of Rhopressa Therapy
The price of Rhopressa may vary based on factors like location, insurance coverage, and pharmacy pricing. A monthly supply often ranges from \$100 to \$150 in the United States. Certain insurance plans or patient assistance programs can offset these costs, so individuals should check with their provider or ask their pharmacist about any applicable discounts.
This article is provided for educational reasons and should not be taken as a substitute for direct medical guidance from a qualified professional. If you believe Rhopressa could help you or a loved one, reach out to an eye care specialist to discuss personalized options. If you found this information valuable, feel free to share it on Facebook, X, or wherever you connect with others seeking effective ways to safeguard their eyesight.