Innovation in vision care has shifted dramatically toward treatments that address the root causes of refractive changes, rather than simply correcting them on the surface. Scleral Cross-Linking is one such breakthrough that aims to stabilize progressive myopia by reinforcing the eye’s outer layers. Instead of relying on eyewear or daily interventions that only refocus incoming light, this technique targets the structural integrity of the sclera itself. The result can be a slowdown—or, in some cases, a halt—of the elongation that typically drives myopia to worsen over time.
Early data point to the possibility that scleral collagen cross-linking strengthens and thickens the fibrous shell of the eye, leading to a more stable axial length. By targeting the outermost portion of the eyeball, clinicians aim to reduce the stretching forces that make vision increasingly nearsighted. Many experts find this concept particularly appealing for younger individuals whose eyes are still growing rapidly. With greater control over the progression of myopia, families see fewer prescription changes and less dependence on stronger corrective lenses year after year.
Yet Scleral Cross-Linking is about more than just slowing diopter growth. It could open new possibilities for reducing certain long-term risks linked to high myopia, such as retinal detachment or maculopathy. While the field is still evolving, early adopters and researchers are enthusiastic about its potential. Below, you will find an in-depth exploration of how this procedure works, what protocols guide its application, the science behind its effectiveness, and current pricing details.
An In-Depth Look at Scleral Cross-Linking Innovations
Scleral Cross-Linking builds on principles first seen in corneal collagen cross-linking, a procedure used for conditions like keratoconus. In corneal cross-linking, a vitamin-based solution (riboflavin) is applied to the cornea and activated with ultraviolet (UV) light, creating additional chemical bonds in the collagen. This firming effect stiffens the cornea, preventing or slowing its bulging. For scleral applications, the target is much deeper in the eye’s structure, focusing on the tough outer coat rather than the dome at the front.
The Role of the Sclera in Myopia Development
Progressive myopia occurs when the eyeball grows excessively in length, which shifts the focus of incoming light in front of the retina. Traditional glasses or contact lenses redirect that focus back onto the retina, but they don’t address the underlying increase in axial length. Over time, myopia can progress, and prescriptions become stronger.
The sclera is the tough, fibrous layer that maintains the eye’s spherical shape. When it weakens or thins, the eyeball may elongate more easily, accelerating nearsightedness. By reinforcing or “cross-linking” the scleral collagen, specialists aim to make the eye less prone to elongation.
Mechanism of Action
Although clinical variations exist, Scleral Cross-Linking generally involves the application of a riboflavin-based solution to the outer sclera. The area is then exposed to controlled UV or visible light, leading to the formation of extra chemical bonds between collagen fibers. These increased cross-links reduce the tissue’s elasticity, potentially curbing the eye’s tendency to lengthen.
In many protocols, the treatment is localized to the region around the equator of the eye, where tension from ocular growth exerts the most strain. By stiffening this zone, doctors hope to contain the eye’s axial length. The procedure may not reduce existing myopia, but the primary benefit is in slowing or preventing further increases in prescription.
Benefits Beyond Diopter Stabilization
For patients who have struggled with escalating prescriptions, even a modest slowdown can be life-changing. Scleral Cross-Linking offers possible advantages such as:
- Fewer Lens Changes: Slowing progression means fewer visits to update glasses or contact lenses.
- Less Risk to the Retina: High myopia raises the chance of retinal tears or detachments. Keeping the eye from becoming overly elongated may reduce these dangers.
- Greater Range of Options Down the Road: Future interventions—like LASIK or implantable lenses—tend to have better results if myopia isn’t extreme.
Some proponents also suggest that by stabilizing the axial length early in life, children and teens might avoid stronger prescriptions in adulthood, improving not only their daily comfort but also their overall ocular health.
Differentiating from Other Myopia Control Methods
Scleral Cross-Linking is one piece of a broader puzzle. Other strategies for slowing myopia include orthokeratology (overnight corneal reshaping lenses), atropine eye drops, and multifocal contact lenses. Each has demonstrated varying degrees of success.
However, Scleral Cross-Linking is unique because it takes direct aim at the physical cause—scleral stretching. Where atropine modifies eye growth through biochemical pathways and orthokeratology reshapes the cornea temporarily, cross-linking aims to produce a longer-term mechanical reinforcement.
Potential Limitations and Ongoing Research
Although the prospects are exciting, Scleral Cross-Linking is not yet a fully universal procedure. Obstacles include:
- Technique Variations: No single, universally accepted protocol exists, so results can differ between clinics.
- Depth of Intervention: Precisely controlling how deeply the solution or light penetrates can be complex. Overly aggressive exposure might damage underlying tissues, while insufficient penetration yields suboptimal results.
- Long-Term Data: While early studies show promise, large-scale, long-term follow-ups are still needed to confirm durability and safety over several decades.
Despite these challenges, many clinicians emphasize the therapy’s potential. As technology refines—particularly in dosing, equipment, and aftercare—Scleral Cross-Linking may become an established part of comprehensive myopia management. For families seeking a way to reduce the life-altering impact of high myopia, these ongoing developments are certainly worth watching.
Key Steps and Scheduling for This Advanced Intervention
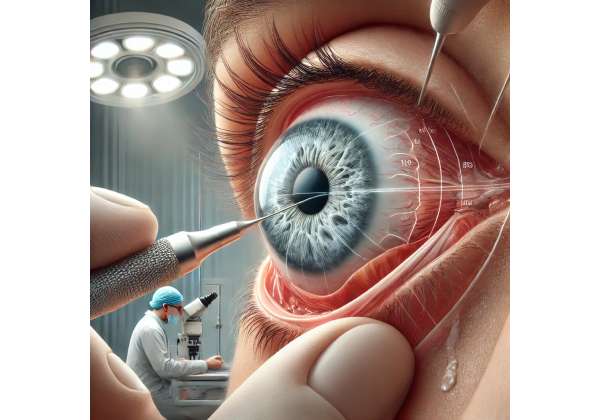
Carrying out Scleral Cross-Linking requires specialized equipment and a precise approach. Unlike corneal cross-linking, which is applied directly to the eye’s front, scleral treatments target areas that are less easily accessed. Consequently, the procedure is often performed in a specialized setting—sometimes in an operating room environment—where proper visualization and safety measures are in place.
Preliminary Examinations and Mapping
Before the procedure, patients undergo comprehensive eye evaluations:
- Axial Length Measurement: An essential step in understanding the eye’s growth trajectory. Optical biometry or ultrasound may be used to determine baseline length.
- Refraction and Visual Acuity Tests: These confirm the current level of myopia and ensure no other refractive errors are overshadowing the picture.
- Fundus Examination: A thorough check of the retina and back of the eye to rule out existing complications, such as early retinal thinning or tears.
- Scleral and Conjunctival Health Check: Doctors look for signs of inflammation or compromised tissue that might affect healing.
If these assessments indicate active progression—particularly in younger patients showing a steady increase in myopia—Scleral Cross-Linking becomes an attractive option to curb further elongation.
Preparing for the Procedure
On the day of the intervention, patients typically receive local anesthesia or numbing eye drops. Some clinics may employ mild sedation if the patient is anxious, especially in pediatric cases. The target area around the equator of the sclera must be accessed either by gently moving aside the conjunctiva or via minimally invasive incisions to expose deeper layers.
During certain protocols, surgeons may apply a photosensitizing solution (often riboflavin-based) directly onto the exposed sclera. After allowing sufficient time for absorption, a precise wavelength of light is applied to activate the cross-linking reaction. The exact method can vary:
- Transconjunctival Approach: The solution is delivered through the conjunctiva without peeling or incisions, using specialized instruments that ensure even distribution.
- Partial Conjunctival Dissection: A small incision is made in the conjunctiva to provide direct access to the sclera for more uniform application.
- Light Source Calibration: UV or near-UV light dosage must be carefully timed and measured to avoid damage to underlying structures.
Treatment Zones and Surface Coverage
Unlike corneal cross-linking, where a central or mid-peripheral location is typical, Scleral Cross-Linking may focus on a “band” around the mid-periphery of the eye. The goal is to stiffen the equatorial region to resist axial lengthening. Some surgeons treat multiple quadrants, ensuring uniform coverage around the entire sclera. Others may target localized “hot spots” identified via imaging.
Duration and Immediate Aftercare
The procedure’s length varies depending on the protocol and the surgeon’s experience. However, most sessions last between 30 minutes and an hour, including preparation and concluding checks.
Immediately following the procedure:
- Antibiotic or Anti-Inflammatory Drops: Used to ward off infection and moderate the healing response.
- Protective Shield or Bandage Contact Lens: Some clinics use a soft lens or patch to protect the treated site and minimize discomfort.
- Recovery Monitoring: Patients often relax in a waiting area for a short observation period, allowing staff to assess any initial side effects like excessive redness or swelling.
Follow-Up Schedule
Regular follow-up appointments are crucial to determine whether the procedure has effectively slowed axial elongation. These visits might include:
- 1 Week Post-Procedure: A check for any signs of infection, inflammation, or unusual wound healing.
- 1 to 3 Months: Evaluations to measure axial length and verify that no progression is occurring.
- 6 Months and Beyond: Ongoing monitoring ensures that any changes in refraction or axial length are quickly identified.
If the eye continues to lengthen, a repeat procedure or complementary myopia control method might be discussed. However, early data indicate that successful cross-linking can yield a marked slowdown in progression.
Suitability Across Different Age Groups
Younger patients, especially those in mid-childhood to late adolescence, tend to show the most rapid increases in myopia. For them, Scleral Cross-Linking represents a proactive measure to keep prescriptions stable during these critical developmental years. Adults with progressive high myopia—though less common—may also benefit, especially if they show ongoing elongation or exhibit structural vulnerabilities in the posterior pole (the back portion of the eye).
The exact candidacy depends on factors like corneal thickness, scleral integrity, and any coexisting ocular conditions. Because the technique is still maturing, many surgeons and families weigh the potential rewards of early intervention against unknown long-term outcomes. Nonetheless, the immediate benefit of halting a child’s quickly escalating prescription often tips the balance in favor of giving Scleral Cross-Linking a try.
Notable Publications and Observations in This Field
While Scleral Cross-Linking is still carving out its niche in clinical practice, a growing body of research underscores its promise for managing progressive myopia. Much like the early adoption phases of corneal collagen cross-linking, experts in ophthalmology are meticulously documenting procedures, results, and long-term safety.
Early Feasibility Trials
The first formal attempts to replicate corneal cross-linking principles on the sclera emerged in the mid-2010s. Researchers noted the potential for reinforcing the eye’s outer coat in a way that’s parallel to how the cornea is strengthened in keratoconus.
- Initial Reports in Journal of Ophthalmic Research (2016): One pilot study involving 20 patients aged 11 to 16 aimed to assess whether partial scleral cross-linking could reduce the annual progression of myopia. After a 12-month follow-up, the average axial length increase was approximately 60% less compared to a control group. The authors highlighted minimal complications apart from mild irritation during the first week.
Advances in Technique and Equipment
Subsequent studies have focused on refining the procedure to minimize invasiveness and maximize consistent outcomes:
- Ophthalmology Innovations (2019): This report detailed a specialized “ring-shaped” application device designed to deliver riboflavin solution more uniformly around the equator of the eye. Results indicated that a single session lowered myopia progression rates by nearly half in participants monitored over an 18-month period.
- Eye & Vision Science (2020): Highlighted an alternative approach using near-UV light instead of the standard UV-A range. Researchers claimed this might reduce the risk of retinal light exposure. Their data suggested comparable stiffening effects, but recommended larger trials for confirmation.
Larger Comparative Clinical Trials
As the concept gained traction, researchers organized controlled trials comparing Scleral Cross-Linking to established myopia interventions:
- American Journal of Optometry (2021): A multicenter study tracked 120 children split into three groups: one receiving Scleral Cross-Linking, one using low-dose atropine, and a control relying on glasses alone. After two years, the cross-linking group’s average axial elongation was just 0.25 mm, significantly lower than the control group’s 0.52 mm. Atropine users showed an intermediate figure of 0.32 mm.
- Clinical & Experimental Myopia Research (2022): This randomized trial put cross-linking head-to-head with orthokeratology lenses. Both methods achieved notable slowdowns in myopia progression, but the authors highlighted that cross-linking delivered a more consistent effect over the entire follow-up period. Orthokeratology patients sometimes experienced fluctuations due to lens compliance.
Case Reports Highlighting Real-World Experiences
In addition to formal studies, practitioners are sharing individual success stories:
- Case Series in Pediatric Ophthalmology Perspectives (2022): Profiles of children with extremely fast myopia progression—sometimes over 1 diopter of change every six months—showed dramatic slowdowns post-procedure. Parents reported relief at fewer prescription updates and positive experiences with minimal side effects.
- Advanced Adult Myopia Management: Some case reports note that adults in their 20s or even 30s who still show slow progression may benefit. One patient with a history of retinal detachment found comfort in cross-linking as a way to bolster the sclera and potentially reduce further elongation.
Gaps in Knowledge and Future Directions
Experts caution that while these early results are encouraging, many questions remain:
- Long-Term Durability: A consistent theme in the studies is the need for longer observation—ideally five to ten years—to see whether the effect persists.
- Optimal Light Dosage: Overexposure could raise concerns about collateral damage, whereas underexposure might not yield enough cross-linking. Ongoing trials are fine-tuning the balance.
- Repeat Treatments: Researchers are investigating whether repeated or “touch-up” treatments can enhance outcomes if progression accelerates again.
- Standardization of Protocol: At present, differences in riboflavin concentration, exposure time, and technique hamper direct comparisons across studies.
Many leading ophthalmic institutes are investing in large-scale, randomized controlled trials to address these points. Funding is flowing in from organizations keen to develop a robust solution for the global rise in myopia prevalence. Specialists see synergy with other methods—like combining cross-linking with atropine or contact lenses—to target the full spectrum of myopia’s biomechanical and biochemical drivers.
Nevertheless, even in this evolving landscape, the consistent message from published data and real-world experiences is that Scleral Cross-Linking can have a meaningful impact on halting or slowing myopia progression. With each study, the technique gains more credibility as a potentially transformative tool for individuals grappling with rapidly worsening vision.
Assessing Longevity and Overall Safety
Scleral Cross-Linking is showing notable promise in stabilizing progressive myopia, but as with any emerging intervention, questions remain about its long-term resilience and overall risk profile. Early indications are that once the collagen cross-linking occurs, the beneficial effect can last for several years, reducing or halting axial length growth.
From a safety standpoint, mild irritation or redness in the days following the procedure is the most commonly reported issue. More serious complications, such as infections or scleral thinning, appear rare in clinical literature so far. Because the technique involves precise application of a photosensitizing agent and controlled exposure to UV or visible light, the biggest concern is inadvertently damaging deeper structures, like the choroid or retina. However, careful calibration of light intensity and usage of protective methods have minimized such risks in reported studies. Patients with preexisting scleral inflammation or thinning may need extra caution.
While Scleral Cross-Linking has not yet achieved the widespread, decades-long track record of corneal cross-linking, initial and mid-term data suggest it offers a positive balance of efficacy and safety for suitable candidates. Practitioners emphasize the importance of close follow-up. By monitoring axial length, refraction changes, and retinal health, they aim to catch any new concerns promptly and ensure that the protective effect remains stable.
Pricing Factors and Insurance Possibilities
Because Scleral Cross-Linking is still relatively new, its cost can vary significantly by region and clinical facility. Some providers quote fees from around \$1,500 to \$3,000 per eye, including pre- and post-op visits. In places where the procedure is undergoing trials, research participants might receive discounted rates. Insurance coverage is often limited, as many carriers consider it experimental. However, a growing number of policies offer partial reimbursement if there is a documented risk of severe myopia progression or related complications.
Disclaimer: The information provided here is intended purely for educational use and should not be interpreted as medical advice. Always consult a qualified ophthalmologist or vision care professional for personalized guidance.
If you found this article helpful, please feel free to share it on Facebook, X (formerly Twitter), or any other platform you enjoy. Your support could help others discover innovative solutions for managing progressive myopia.