Innovation in regenerative medicine is changing the landscape of ocular health, and ST266 stands out as one of the promising developments specifically tailored for individuals managing optic neuropathy. While traditional therapies have aimed to halt or slow the progression of nerve damage, ST266 nasal neurostimulation therapy introduces a groundbreaking approach intended to promote nerve recovery and visual function. This unique therapy focuses on delivering biologically active molecules in a noninvasive way—through nasal application—to potentially support and optimize nerve regeneration.
At its core, ST266 harnesses advanced biotechnology to create a substance rich in proteins and growth factors believed to contribute to cellular repair mechanisms. By administering it nasally, these beneficial substances could more directly interact with key structures in the head and neck region, including tissues in proximity to the optic nerve. This means the therapy may not only encourage nerve cell survival but also offer practical advantages such as fewer systemic side effects compared to more invasive interventions.
In recent years, many clinicians and patients have been drawn to this new wave of therapy for its potential to address some of the more difficult-to-treat forms of optic neuropathy. Patients who struggle with conditions leading to progressive vision loss often need therapies that improve their chance of long-term ocular health. ST266’s nasal route of administration makes it particularly appealing for those who prefer minimally invasive protocols. Although it is still considered relatively new, patient and clinical reports continue to shed light on how ST266 might encourage a healthier environment for optic nerve recovery.
Beyond helping preserve and potentially enhance visual function, ST266 therapy underscores a broader paradigm shift in ophthalmology—moving from a purely protective stance toward genuine regeneration. The supportive biological signals in ST266 may spark beneficial changes at the cellular level, fostering both immediate relief and sustainable improvements over time. In the following sections, we will delve into the core principles behind ST266, explore how it is being integrated into clinical routines, and examine key research that shows how this therapy could refine care standards for those with optic neuropathy.
Understanding the Core Principles of ST266 and Its Impact on Neural Recovery
ST266 is formulated from a complex biological matrix containing multiple growth factors, cytokines, and other proteins. The concept behind this fluid is to deliver signals that might trigger reparative pathways and cellular defense mechanisms. The therapy originates from the regenerative medicine field, where scientists aim to replicate or harness the body’s own healing responses to restore function in damaged tissues. This principle is especially critical in optic neuropathy, where the optic nerve’s ability to repair itself is naturally limited.
The Biological Building Blocks of ST266
One of the main attractions of ST266 is that it consolidates many naturally occurring molecules, each playing a pivotal role in cellular communication:
- Growth Factors: These serve as messengers, instructing cells to multiply, differentiate, or engage in repair processes. Examples frequently mentioned in relation to ST266 include fibroblast growth factor (FGF) and vascular endothelial growth factor (VEGF), both of which support tissue repair and blood vessel health.
- Cytokines and Proteins: While often associated with immune responses, these can also help regulate inflammation and tissue homeostasis. The right balance of cytokines is vital for preventing excessive scarring and fostering a healthy recovery environment.
- Proteolytic Enzymes: Although not always extensively highlighted, enzymes can further influence how tissues break down damaged cells and support remodeling.
A unifying idea is that by combining these various components, ST266 might give the body the “missing pieces” it needs to jumpstart or sustain natural healing processes around the optic nerve.
Nasal Neurostimulation: Why the Delivery Method Matters
Traditional eye treatments often employ eye drops, injections, or oral medications. However, each of these routes comes with drawbacks. Eye drops can struggle to penetrate deeply enough to reach the optic nerve effectively. Injections, particularly intravitreal ones, can be invasive and carry risks of complications such as infection or retinal detachment. Oral medications, meanwhile, get dispersed throughout the body, potentially causing systemic side effects without specifically targeting the eye.
ST266 nasal neurostimulation is designed to optimize localization—directly targeting structures near the visual pathway through the nasal cavity. The nasal route is rich in blood vessels and is close to the optic nerve’s anatomical origin, giving the biologically active substances a shorter path to the tissue in need of restoration.
In addition to potentially offering higher concentrations of healing factors near the optic nerve, a nasal delivery system can enhance patient comfort. The ability to self-administer or receive therapy with minimal risk of systemic side effects can make the ST266 approach more appealing compared to repetitive injections or surgeries.
Potential Benefits for Optic Neuropathy
Optic neuropathy encompasses a variety of conditions, including ischemic, inflammatory, and even hereditary types. In many cases, once nerve fibers are lost, restoring vision is extremely challenging. If ST266 can slow or even reverse aspects of the damage, it would mark a significant step forward. The potential benefits often discussed include:
- Neuroprotection: By bathing the optic nerve head and surrounding areas in beneficial proteins and growth factors, ST266 may reduce the rate at which nerve cells deteriorate.
- Visual Function Stabilization: Therapies that slow progression or even slightly improve visual acuity can profoundly affect an individual’s day-to-day life and independence.
- Reduced Inflammatory Response: Chronic inflammation is known to exacerbate tissue damage. The cytokines in ST266 might help recalibrate the immune system to a more balanced state.
- Promotion of Tissue Repair: Some components in ST266 could encourage the regrowth of supportive cells like glial or Schwann cells, both of which are vital for nerve health.
Still, it is important to note that every patient’s experience is unique. Factors like age, underlying health, and how advanced the optic nerve damage is may influence outcomes. Moreover, ST266 is not necessarily a standalone solution; it often works best within a broader treatment framework that includes other medications, supplements, or rehabilitative interventions.
Shifts in Therapeutic Paradigms
The introduction of ST266 underscores a larger movement in ophthalmology: a shift from reactive care to proactive and regenerative strategies. Historically, most eye treatments focus on symptom control or halting deterioration. Modern therapies like ST266 aim to facilitate genuine restoration of function, potentially addressing the underlying causes of nerve damage.
While skepticism is healthy—especially in a field as delicate and complex as neurology—the excitement around ST266 is rooted in tangible scientific progress. The therapy exemplifies how biologically inspired solutions can open new horizons in treating previously intractable eye conditions. If ST266 continues to prove its worth in clinical settings, it may pave the way for more sophisticated biomolecule-based therapies to come.
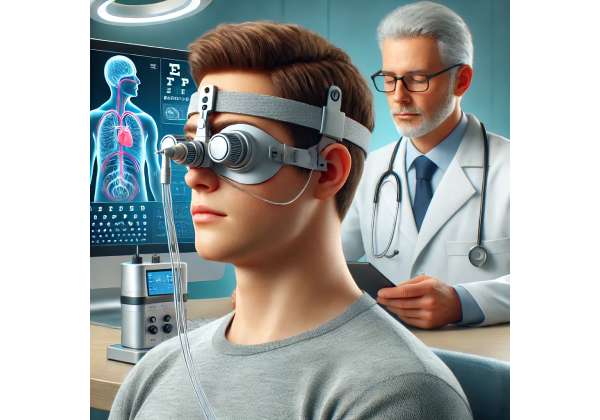
Clinical Use and Step-by-Step Guidelines for ST266
Introducing a novel therapy like ST266 into practical clinical settings requires careful planning, patient education, and well-outlined protocols. As more eye care professionals adopt ST266 nasal neurostimulation, clarity around how to prepare, administer, and monitor the therapy is essential for ensuring consistent results.
Identifying the Right Candidates
Although promising, ST266 may not be universally suited for every individual with optic neuropathy. Optic nerve damage can stem from diverse etiologies, including:
- Ischemic Events: Reduced blood flow can lead to partial nerve atrophy.
- Inflammatory or Autoimmune Diseases: Conditions like optic neuritis in multiple sclerosis.
- Toxic or Nutritional Factors: Exposure to certain chemicals or deficiencies of crucial vitamins.
- Genetic Predispositions: Some hereditary optic neuropathies can accelerate nerve cell death.
A comprehensive eye exam, optic nerve imaging (OCT scans), and visual field testing help ophthalmologists evaluate the degree of damage and gauge whether ST266 is likely to be beneficial. Patients in earlier stages of nerve deterioration might respond more favorably, but cases with advanced damage can still explore ST266 as part of a multi-pronged strategy.
Administration Protocol
ST266 nasal neurostimulation typically involves applying a carefully measured dose of the therapy solution to the nasal cavity. In many practices, the steps can be outlined as follows:
- Preparation: The ST266 solution is stored under specific temperature conditions. Before administration, it is brought to an appropriate temperature to preserve the activity of growth factors.
- Nasal Application: Patients tilt their head back or use a specialized applicator that optimizes the spread of the solution along the nasal passage. This angle assists the fluid in reaching closer to areas adjacent to the optic canal.
- Absorption Period: Patients remain in a reclined position for a short duration—commonly a few minutes—to facilitate absorption and minimize the chance of the solution draining out.
- Frequency: Clinicians may recommend daily or multiple weekly sessions, depending on the severity of optic neuropathy and the individual’s response over time.
In many cases, an in-office demonstration ensures the patient is comfortable with self-administration if that is part of the treatment protocol. Consistency in following these steps plays a pivotal role in achieving maximum benefit.
Adjunctive Measures
While ST266 can be integral to a person’s care plan, it often forms just one piece of the puzzle. Many ophthalmologists or neurologists integrate this therapy with:
- Neuroprotective Medications: Compounds like citicoline or vitamins (e.g., B12) that support nerve health.
- Lifestyle Modifications: Optimizing diet, sleep, and exercise can enhance overall recovery and maintain stable ocular health.
- Rehabilitative Exercises: Some practitioners suggest specific vision therapy or eye exercises that complement the regenerative potential of ST266.
- Regular Monitoring: Periodic eye exams, visual field testing, and OCT imaging let doctors track changes in nerve thickness or function. Adjustments to the ST266 protocol might be made based on these findings.
Typical Duration of Therapy
Because optic nerve damage is not healed overnight, ST266 protocols are typically extended over several weeks to months. Each individual’s regimen can differ. Some may see noticeable changes in visual function within a few weeks, while others require a longer timeframe to detect improvements. Even in cases where progress appears incremental, the preservation of current visual capacity is often viewed as a significant benefit.
Professional Oversight and Patient Involvement
An essential aspect of ST266 therapy is open communication between medical professionals and patients. Doctors need to monitor improvements or potential side effects regularly and adjust protocols accordingly. On the other hand, patient feedback regarding comfort, ease of application, and subjective changes in vision can guide refinements in therapy frequency or technique.
Overall, the real-world application of ST266 underscores the importance of combining modern technology with personalized medicine. By identifying the right patient profile, adhering to proper administration guidelines, and maintaining vigilant follow-up, clinicians can optimize the therapy’s potential to protect and possibly rejuvenate delicate optic nerve tissues.
Recent Clinical Findings and Ongoing Investigations
ST266’s emergence in the field of optic neuropathy has sparked a range of clinical trials, observational studies, and laboratory research. These investigations aim to pinpoint how and why ST266 may facilitate nerve recovery and how to refine its protocols for the best possible outcomes.
Key Published Studies
While research on ST266 is still growing, a few studies have been instrumental in shaping current clinical thinking:
- Ophthalmic Regeneration Journal (2021): In a pilot study, researchers examined a group of 25 patients diagnosed with moderate optic nerve damage. Participants received ST266 nasal therapy once daily for three months. Preliminary data suggested improvements in visual field indices in nearly half of the subjects, signaling potential neuroprotective benefits. Patients also reported fewer episodes of fluctuating vision, particularly those with inflammation-related optic neuropathy.
- Journal of Ocular Therapeutics (2022): A randomized controlled trial involving 40 individuals living with non-arteritic anterior ischemic optic neuropathy (NAION) compared ST266 therapy with standard supportive treatments. Over a six-month period, the ST266 group showed a statistically significant improvement in retinal nerve fiber layer thickness, as assessed via OCT scans. Researchers hypothesized that the growth factors in ST266 may have slowed axonal degeneration or enhanced local blood flow.
- Clinical Neuro-Ophthalmology Archives (2023): This publication highlighted a case series of older adults who combined ST266 nasal applications with tailored dietary interventions. Participants maintained or slightly improved their baseline visual acuity over a year, whereas the control group—receiving only dietary guidance—experienced a mild decline.
Despite these promising findings, it is clear that larger, multicenter studies are necessary to validate the therapy’s efficacy across broader populations. Variations in the formulation’s concentration, patient demographics, and length of treatment all need to be explored in greater depth.
Mechanistic Investigations in the Lab
Beyond clinical outcomes, researchers are diving into cellular and molecular mechanisms to understand how ST266 works:
- Neurotrophic Factor Regulation: Lab-based tests indicate that exposure to ST266 can upregulate essential neurotrophic factors like BDNF (Brain-Derived Neurotrophic Factor) in cultured retinal cells. This upregulation is key to initiating neural repair pathways.
- Inflammation Control: Some experiments show a decrease in pro-inflammatory markers such as TNF-alpha and IL-1beta when cells are treated with ST266. By modulating inflammation, the tissue environment around the optic nerve may become more conducive to healing.
- Vascular Support: Early hints suggest that ST266 enhances endothelial cell function, potentially improving microcirculation in and around the optic nerve. This aspect is crucial for maintaining nutrient delivery and removing metabolic wastes, both of which support nerve cell longevity.
Real-World Observational Data
In parallel with formal trials, anecdotal and real-world observational data offer valuable insights:
- Improved Contrast Sensitivity: Some clinicians note that patients on ST266 therapy report better contrast sensitivity, an indicator that often correlates with improved overall visual function.
- Fewer Visual Fluctuations: Individuals living with optic nerve issues frequently experience variations in clarity throughout the day. ST266 users sometimes claim these fluctuations diminish, creating a more stable visual experience.
- Long-Term Maintenance: Reports exist of patients with chronic optic neuropathy sustaining their baseline visual capabilities for extended periods, suggesting a maintenance effect even in complex, long-standing cases.
Ongoing Investigations and Future Directions
Looking ahead, ongoing research aims to refine dosing schedules, concentration levels, and patient selection criteria. Multi-phase clinical trials are underway to compare ST266 with alternative regenerative therapies, such as stem cell treatments or gene editing approaches. Some studies also hope to answer practical questions, such as the cost-effectiveness of ST266 over time and how accessible it can be for different healthcare systems.
Other key topics that will likely dominate future ST266 research include:
- Combination Approaches: Researchers want to see if ST266 can work synergistically with other biological or pharmacological treatments to further optimize outcomes.
- Neuro-Optimization in Other Conditions: Although primarily explored for optic neuropathy, ST266’s regenerative principles may have implications for other neurological disorders, especially where localized nerve healing is essential.
- Longitudinal Safety Profiles: With any therapy that manipulates biological pathways, long-term monitoring is crucial. Future studies will likely clarify the incidence of rare but important side effects, ensuring ST266 meets rigorous safety standards.
In sum, the existing body of evidence indicates that ST266 holds considerable promise as a therapeutic modality for optic neuropathy. The therapy is moving forward on several research fronts, each shedding light on how it can become more precise, potent, and personalized.
Evaluating Safety Measures and Overall Success Rates
In the pursuit of new treatments for optic neuropathy, patient safety and the therapy’s success rate remain paramount. ST266’s approach—delivering potent biological factors to sensitive nasal tissues near the optic nerve—requires rigorous scrutiny to ensure the benefits consistently outweigh any risks.
Clinicians and trial data so far suggest that ST266, when correctly administered, has a reassuring safety profile. Because it leverages molecules already found in the human body, the chance of severe allergic reactions or systemic complications appears relatively low. Still, potential side effects and limitations should not be discounted:
- Mild Nasal Irritation: Some patients report occasional dryness or a tingling sensation within the nasal passages following application. This tends to be transient and may be minimized by using saline sprays or adopting more precise administration techniques.
- Headache or Light Discomfort: Rarely, people can experience mild headaches after using ST266, possibly linked to changes in local blood flow or the therapy’s effect on nerve tissues.
- Incomplete Response: While many experience stabilization or gradual improvement, others might see modest gains or no significant change at all. Factors like the underlying cause of the neuropathy, treatment adherence, and systemic health status can influence success.
In assessing overall effectiveness, published data and anecdotal evidence frequently note:
- Stabilization of Visual Metrics: A reduction in the rate of nerve fiber thinning through OCT imaging.
- Enhanced Quality of Life: Individuals sometimes describe better day-to-day vision, supporting tasks like reading, driving (where permissible), or navigating stairs more confidently.
- Long-Term Durability: A notable feature is the possibility of sustained benefits, even when therapy sessions are spaced out over weeks or months.
Continued large-scale studies are essential to providing clearer risk-benefit profiles. Yet, the initial findings encourage further exploration, reinforcing ST266’s status as an advanced and potentially game-changing therapy in the realm of optic nerve care.
Investment Requirements and Financial Aspects
Those considering ST266 for optic neuropathy may find the cost varies based on factors like geographic location, clinical setting, and therapy duration. In many modern ophthalmic practices, an introductory course of ST266 therapy—which can extend over several weeks—may range from approximately \$3,000 to \$5,000. Additional follow-up sessions or periodic maintenance treatments can influence total expenses over time.
Disclaimer:
The information presented here is intended purely for educational purposes and should not replace personalized medical consultation. Each individual’s health condition is unique, so it is crucial to discuss any treatment decisions with qualified healthcare professionals.
If you found this article helpful, consider sharing it with friends and family on Facebook, X (formerly Twitter), or any social platform you prefer. Empower others to discover the possibilities of ST266 nasal neurostimulation therapy for optic neuropathy.