The pharynx is a vital structure that plays a central role in both the respiratory and digestive systems. Acting as a shared pathway for air and food, it not only facilitates breathing and swallowing but also contributes to voice production and immune defense. Understanding the pharynx’s complex anatomy and functions is crucial for diagnosing related disorders and implementing effective treatments. This comprehensive guide offers an in‐depth look into the structural details, physiological processes, common conditions, and modern therapeutic options, along with practical health tips to maintain optimal pharyngeal wellness.
Table of Contents
- Pharyngeal Structure and Detailed Anatomy
- Physiological Roles and Functional Mechanisms
- Pharyngeal Disorders and Conditions
- Diagnostic Methods for Pharyngeal Issues
- Therapeutic and Management Strategies
- Nutritional Strategies and Supplementation
- Preventative Care and Healthy Habits
- Trusted Information and Further Resources
- Frequently Asked Questions
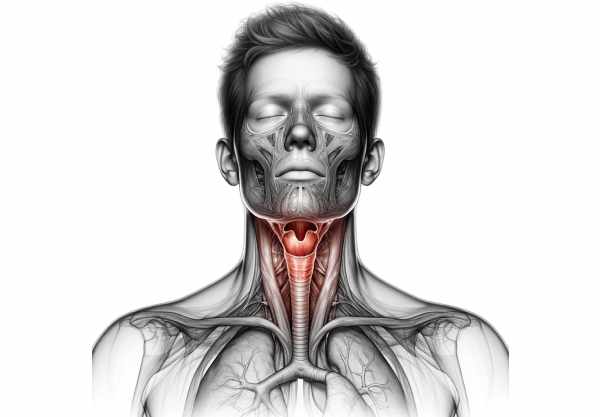
Pharyngeal Structure and Detailed Anatomy
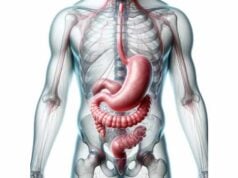
The pharynx is a complex, muscular tube that forms an integral part of the upper aerodigestive tract. It is divided into three major regions—each with distinctive anatomical features and functions—that collectively facilitate breathing, swallowing, and voice production.
Subdivisions of the Pharynx
Nasopharynx
Located posterior to the nasal cavities, the nasopharynx extends from the base of the skull to the upper surface of the soft palate. Its main functions include:
- Pharyngeal Tonsils (Adenoids): Lymphoid tissues that line the posterior wall, playing a pivotal role in immune surveillance by capturing inhaled pathogens.
- Eustachian Tubes: Openings on the lateral walls that connect the nasopharynx to the middle ear, ensuring pressure equalization essential for proper auditory function.
Oropharynx
Situated behind the oral cavity, the oropharynx spans from the soft palate to the upper border of the epiglottis. It functions as a common pathway for both food and air. Key structures include:
- Palatine Tonsils: Paired lymphoid tissues flanking the oropharynx, which contribute to immune defense.
- Uvula: A conical projection from the soft palate that aids in speech articulation and swallowing by helping close off the nasopharynx.
- Fauces: The gateway between the oral cavity and the oropharynx, critical in directing the passage of food.
Laryngopharynx (Hypopharynx)
The laryngopharynx extends from the upper border of the epiglottis down to the lower border of the cricoid cartilage, where it meets the esophagus. It channels both air into the larynx and food into the esophagus. Important components include:
- Epiglottis: A flexible, leaf-shaped cartilage that covers the glottis during swallowing, preventing food from entering the airways.
- Piriform Sinuses: Recesses that flank the laryngeal inlet, directing ingested materials toward the esophagus.
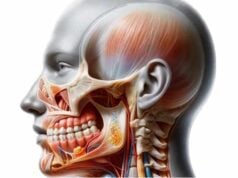
Muscular Composition and Support
The pharynx is composed of several layers of muscles that ensure its dynamic function. These include:
- Pharyngeal Constrictors: The superior, middle, and inferior constrictor muscles form a continuous muscular ring. They contract sequentially during swallowing, effectively pushing the bolus downward.
- Longitudinal Muscles: Muscles such as the stylopharyngeus, palatopharyngeus, and salpingopharyngeus help elevate the pharynx and larynx during swallowing and speech, contributing to both the movement and structural integrity of the pharynx.
Innervation and Blood Supply
Neural Control
The pharynx is innervated by a complex network known as the pharyngeal plexus. This network is primarily formed by:
- Vagus Nerve (Cranial Nerve X): Supplies motor fibers that control muscle contraction and autonomic functions.
- Glossopharyngeal Nerve (Cranial Nerve IX): Provides significant sensory input, particularly in the oropharynx.
- Maxillary Branch of the Trigeminal (Cranial Nerve V): Contributes sensory fibers to the nasopharynx.
Vascularization
Blood supply to the pharynx is rich and predominantly derived from branches of the external carotid artery, such as:
- Ascending Pharyngeal Artery: Supplies the upper regions.
- Facial and Lingual Arteries: Contribute to the vascular network, ensuring sufficient oxygenation and nutrient delivery.
Venous drainage occurs through the pharyngeal venous plexus, which ultimately channels blood to the internal jugular vein.
Lymphatic Drainage
The lymphatic system of the pharynx is crucial for immune defense and maintaining fluid balance. Lymph from the pharynx drains primarily into the deep cervical lymph nodes, which act as a filtration system to remove pathogens and debris.
Histological Features
The inner lining of the pharynx varies by region:
- Nasopharynx: Lined with pseudostratified ciliated columnar epithelium, which traps particles and moistens inhaled air.
- Oropharynx and Laryngopharynx: These areas are covered with stratified squamous epithelium, providing protection against abrasion from food and mechanical stress during swallowing.
This intricate anatomical design allows the pharynx to serve its multiple functions with remarkable efficiency, while also playing a central role in immune defense.
Physiological Roles and Functional Mechanisms
The pharynx is indispensable for several fundamental bodily functions. Its coordinated physiological processes are essential for both the respiratory and digestive systems, ensuring that air and food follow their proper pathways.
Swallowing (Deglutition)
Swallowing is a multistage process that involves:
- Oral Phase: The voluntary phase where the tongue shapes the bolus and propels it into the oropharynx.
- Pharyngeal Phase: An involuntary reflex phase during which the soft palate rises to block the nasopharynx, and the epiglottis folds over the laryngeal inlet. Simultaneously, the pharyngeal constrictor muscles contract sequentially to move the bolus into the esophagus.
- Esophageal Phase: Peristaltic waves in the esophagus propel the food toward the stomach.
This coordinated effort ensures that food is directed away from the airway, preventing aspiration.
Breathing
As part of the respiratory system, the pharynx provides a passage for air from the nasal and oral cavities to the larynx and trachea. Its open, muscular structure maintains airway patency during both inhalation and exhalation. The tone of the pharyngeal muscles, regulated by neural inputs, is critical for unobstructed airflow.
Vocalization
The pharynx acts as a resonating chamber that influences the sound produced by the vocal cords. By modifying the shape and volume of its cavity, the pharynx can alter the pitch, tone, and quality of the voice. This role is essential for clear speech and effective communication.
Immune Defense
The pharynx contains lymphoid tissues such as the adenoids and tonsils, which serve as the first line of immune defense. These tissues capture and neutralize pathogens that enter through the nasal or oral routes. The generation of lymphocytes and antibodies within these tissues is vital for both local and systemic immune responses.
Pressure Equalization
The Eustachian tubes, which open into the nasopharynx, balance the air pressure between the middle ear and the external environment. This function is especially important during altitude changes, such as during airplane travel or diving, preventing discomfort and potential damage to the ear.
Coordination and Integration
All these functions are integrated seamlessly by the pharynx, whose complex anatomy and muscular coordination allow it to perform multiple roles simultaneously. Any disruption in these processes—whether due to infection, injury, or structural abnormalities—can significantly impair breathing, swallowing, and speech.
The pharynx’s ability to adapt to various functional demands underscores its importance in maintaining overall health and quality of life.
Pharyngeal Disorders and Conditions
A range of disorders can affect the pharynx, compromising its function and impacting overall well-being. These conditions may arise from infections, inflammation, structural abnormalities, or neoplastic processes. Early diagnosis and effective treatment are essential for preventing complications.
Pharyngitis
Pharyngitis, commonly referred to as a sore throat, is characterized by inflammation of the pharyngeal mucosa. It can be caused by:
- Viral Infections: Such as the common cold or influenza.
- Bacterial Infections: Notably streptococcal bacteria, leading to strep throat.
- Allergic Reactions: Environmental allergens may trigger inflammation.
Symptoms include:
- Pain and discomfort in the throat.
- Redness and swelling.
- Fever and enlarged lymph nodes in bacterial cases.
Treatment typically involves rest, hydration, and analgesics; bacterial cases may require antibiotics.
Tonsillitis
Tonsillitis is the inflammation of the palatine tonsils, which are located in the oropharynx. It is commonly caused by viral or bacterial infections and may result in:
- Severe throat pain.
- Swollen, red tonsils sometimes with white patches.
- Difficulty swallowing and high fever.
Chronic or recurrent tonsillitis may necessitate surgical removal of the tonsils (tonsillectomy).
Obstructive Sleep Apnea (OSA)
Obstructive sleep apnea is characterized by repetitive episodes of upper airway obstruction during sleep. In many cases, the pharynx is the site of obstruction.
Key symptoms include:
- Loud snoring and gasping during sleep.
- Daytime sleepiness and fatigue.
- Cognitive impairment due to fragmented sleep.
Treatment may involve lifestyle changes, use of continuous positive airway pressure (CPAP) devices, or surgical interventions to remove or reduce obstructive tissues.
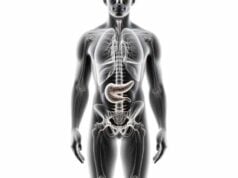
Laryngopharyngeal Reflux (LPR)
LPR occurs when gastric contents reflux into the laryngopharynx, leading to inflammation and irritation. Unlike classic gastroesophageal reflux disease (GERD), LPR often presents without heartburn.
Common symptoms include:
- Chronic throat clearing and cough.
- Hoarseness and a sensation of a lump in the throat.
- Sore throat and difficulty swallowing.
Management includes dietary modifications, weight loss, and acid-suppressive medications such as proton pump inhibitors (PPIs).
Additional Conditions
Other disorders affecting the pharynx include:
- Pharyngeal Cancer: Rare malignancies that often present with persistent throat pain, difficulty swallowing, unexplained weight loss, and changes in voice. Treatment may involve a combination of surgery, radiation therapy, and chemotherapy.
- Epiglottitis: A life-threatening condition marked by inflammation of the epiglottis, leading to airway obstruction. Immediate medical intervention is required.
- Peritonsillar Abscess: A complication of tonsillitis where pus accumulates near the tonsils, causing severe pain, fever, and difficulty opening the mouth. Treatment involves antibiotics and, frequently, surgical drainage.
Understanding these conditions and their underlying causes is crucial for early detection and timely intervention, thereby minimizing the risk of serious complications.
Diagnostic Methods for Pharyngeal Issues
Accurate diagnosis of pharyngeal disorders is critical for implementing effective treatment plans. Clinicians employ a combination of clinical evaluations, imaging techniques, endoscopic examinations, and laboratory tests to arrive at a definitive diagnosis.
Clinical Assessment
The diagnostic process generally begins with:
- Medical History: Detailed information on symptom onset, duration, severity, and associated factors such as recent infections or allergies.
- Physical Examination: A thorough inspection of the pharynx using lighted instruments to identify signs of inflammation, swelling, lesions, or abnormal tissue. Palpation of the neck to assess lymph node enlargement is also performed.
Imaging Techniques
Various imaging modalities provide crucial insights into pharyngeal structure and function:
- X-rays and Barium Swallow Studies: Useful for evaluating the soft tissue contours of the pharynx and assessing swallowing function.
- Computed Tomography (CT) Scans: Provide cross-sectional images that help detect masses, abscesses, or structural abnormalities.
- Magnetic Resonance Imaging (MRI): Offers high-resolution images of soft tissues and is particularly useful in evaluating tumors, infections, and complex anatomical details.
Endoscopic Examinations
Endoscopy allows for direct visualization of the pharyngeal mucosa:
- Nasopharyngoscopy: A flexible endoscope is inserted through the nose to inspect the nasopharynx and upper larynx.
- Laryngoscopy: Direct examination of the larynx and hypopharynx using either a flexible or rigid scope, enabling detection of lesions or structural anomalies.
Biopsies can be taken during endoscopic procedures if suspicious tissues are identified.
Laboratory Investigations
Laboratory tests aid in confirming infections and inflammatory conditions:
- Throat Swab Cultures and Rapid Antigen Detection Tests (RADT): Essential for identifying bacterial pathogens, particularly in cases of streptococcal pharyngitis.
- Blood Tests: Including complete blood count (CBC) and inflammatory markers, which can indicate systemic infection or immune response.
- Allergy Testing: Skin prick tests or serum IgE measurements may be conducted if allergic pharyngitis is suspected.
Functional Assessments
Specialized tests evaluate the dynamic functions of the pharynx:
- Videofluoroscopic Swallow Study (VFSS): A real-time X-ray study that visualizes the swallowing process and detects dysfunction during the pharyngeal phase.
- Manometry: Measures the pressure within the pharynx and esophagus during swallowing, providing insights into muscular coordination and function.
- Sleep Studies (Polysomnography): Used to diagnose obstructive sleep apnea by monitoring breathing patterns, oxygen saturation, and other physiological parameters during sleep.
These comprehensive diagnostic methods enable clinicians to develop a targeted treatment plan tailored to the specific pharyngeal disorder.
Therapeutic and Management Strategies
Treatment of pharyngeal disorders is multifaceted and depends on the specific condition, its severity, and the overall health of the patient. Therapeutic options range from conservative medical management to surgical intervention and innovative therapies.
Medical Treatments
Medications play a key role in managing pharyngeal conditions:
- Antibiotics: Prescribed for bacterial infections such as streptococcal pharyngitis and tonsillitis.
- Antiviral Agents: Used in cases of viral pharyngitis to reduce symptom severity.
- Anti-inflammatory Drugs: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen help alleviate pain and inflammation.
- Corticosteroids: May be used to reduce severe inflammation or allergic responses.
- Acid-Suppressive Medications: Proton pump inhibitors (PPIs) and H2 blockers are critical in treating laryngopharyngeal reflux (LPR) by decreasing gastric acid production.
Surgical Interventions
When conservative management fails, surgical options may be indicated:
- Tonsillectomy and Adenoidectomy: Removal of chronically inflamed tonsils and adenoids to alleviate recurrent infections and airway obstruction.
- Uvulopalatopharyngoplasty (UPPP): Surgical removal of excess tissue in the oropharynx and soft palate to treat obstructive sleep apnea.
- Endoscopic Sinus Surgery: For patients with chronic sinusitis affecting the nasopharynx.
- Transoral Robotic Surgery (TORS): A modern, minimally invasive approach for removing tumors or other abnormalities from the pharynx.
Supportive and Innovative Therapies
Supportive Treatments include:
- Speech and Swallowing Therapy: Rehabilitation programs led by speech-language pathologists help improve swallowing mechanics and vocal function.
- Physical Therapy: May benefit patients with muscular dysfunction affecting the pharynx.
- Continuous Positive Airway Pressure (CPAP): The primary treatment for obstructive sleep apnea, maintaining airway patency during sleep.
Innovative Approaches:
- Radiofrequency Ablation: Minimally invasive technique that uses radiofrequency energy to reduce hypertrophic tissue in obstructive sleep apnea.
- Implantable Devices: Emerging therapies such as hypoglossal nerve stimulation (Inspire Therapy) offer new options for maintaining airway patency in sleep-disordered breathing.
The choice of treatment is tailored to each patient’s needs, with an emphasis on restoring normal function, relieving symptoms, and preventing complications.
Nutritional Strategies and Supplementation
Optimal pharyngeal health is supported not only by medical interventions but also by proper nutrition and targeted supplementation. A well-balanced diet and specific supplements can bolster the immune system, reduce inflammation, and maintain mucosal integrity.
Key Nutrients and Vitamins
- Vitamin C:
Acts as a potent antioxidant that promotes immune function and protects the mucosal lining from infections. Adequate vitamin C intake may reduce the severity and duration of common colds and sore throats. - Vitamin D:
Essential for immune regulation and maintaining respiratory health, vitamin D helps prevent infections and supports overall mucosal integrity in the pharynx. - Zinc:
Known for its immune-boosting properties, zinc aids in reducing the duration of upper respiratory infections and supports tissue repair.
Herbal and Natural Supplements
- Echinacea:
A herbal remedy celebrated for its ability to stimulate the immune system. Echinacea may help reduce the incidence and severity of pharyngeal infections. - Slippery Elm:
This natural supplement soothes the mucous membranes of the throat, reducing irritation and providing relief from discomfort associated with inflammation. - Licorice Root:
Known for its anti-inflammatory and demulcent properties, licorice root can ease throat pain and reduce pharyngeal inflammation, though long-term use should be monitored. - Omega-3 Fatty Acids:
Found in fish oil, omega-3s have strong anti-inflammatory effects, which can help mitigate inflammation in the pharynx and support overall respiratory health.
Probiotics
Probiotics enhance gut and immune health, indirectly contributing to the prevention of upper respiratory infections. Maintaining a balanced gut flora can have beneficial effects on the immune responses in the pharyngeal region.
Integrating these nutritional strategies into a daily regimen—along with a balanced diet rich in fruits, vegetables, lean proteins, and whole grains—can have a synergistic effect on pharyngeal health and overall well-being.
Preventative Care and Healthy Habits
Preventing pharyngeal disorders begins with adopting a lifestyle that supports optimal mucosal and immune health. Small, consistent habits can significantly reduce the risk of infections and chronic inflammation.
Key Preventative Measures
- Hydration:
Drinking adequate water keeps the pharyngeal mucosa moist, reducing irritation and preventing dryness. - Oral Hygiene:
Regular brushing, flossing, and tongue cleaning prevent the buildup of bacteria that could ascend to the pharynx and cause infections. - Avoidance of Smoking:
Smoking irritates the pharyngeal tissues and compromises the immune defense, increasing the risk of chronic pharyngitis and cancer. - Moderate Alcohol Consumption:
Excessive alcohol can dehydrate and irritate the throat, so moderation is key to maintaining mucosal health. - Humidification:
Using a humidifier, especially during dry seasons or in arid climates, helps keep the airways moist and reduces throat irritation.
Dietary and Lifestyle Recommendations
- Balanced Diet:
Focus on nutrient-dense foods that bolster the immune system—fruits, vegetables, lean proteins, and whole grains support overall health. - Regular Exercise:
Physical activity improves cardiovascular health and enhances immune function, which can indirectly benefit pharyngeal health. - Stress Management:
Chronic stress can weaken the immune system. Practices such as meditation, yoga, and deep breathing can help reduce stress levels. - Safe Eating Practices:
Chewing food thoroughly and avoiding talking while eating can prevent choking and minimize the risk of pharyngeal injury. - Management of Acid Reflux:
If you suffer from acid reflux, lifestyle modifications and dietary changes are essential to protect the pharyngeal mucosa from acid-induced irritation.
Regular Medical Check-Ups
Routine health screenings and prompt medical attention when symptoms arise are vital. Regular check-ups help detect early signs of pharyngeal disorders, allowing for timely intervention before complications develop.
By incorporating these preventative strategies, you can significantly enhance your pharyngeal health and overall quality of life.
Trusted Information and Further Resources
Access to reliable information is critical for managing pharyngeal health. Whether you are a patient seeking advice or a healthcare professional looking for the latest research, a variety of reputable sources are available.
Recommended Books
- “The Throat and Esophagus: The Voice and Swallowing Disorders Sourcebook” by John M. Rubin:
This comprehensive guide explores disorders of the throat and esophagus, offering insights into diagnosis and treatment options. - “Pharyngeal Diseases and Treatment” by Michael Gleeson:
An in-depth resource focusing on the diseases affecting the pharynx and the modern therapeutic strategies used in treatment. - “Otolaryngology: A Color Handbook” by Rogan Corbridge:
A visually engaging handbook that covers the anatomy, physiology, and pathologies of the ear, nose, and throat, including pharyngeal disorders.
Academic Journals
- The Laryngoscope:
A peer-reviewed journal featuring the latest research and advancements in otolaryngology, with a focus on pharyngeal health and related disorders. - Journal of Voice:
This publication offers research articles on voice disorders, including studies on how pharyngeal conditions affect vocal function.
Mobile Applications
- MySwallowing Aid:
An app designed to assist individuals with swallowing difficulties by providing guided exercises and tracking progress. - CPAP Tracker:
Essential for patients with sleep apnea, this app monitors CPAP usage and offers tips for optimizing therapy. - Allergy Plus by Pollen.com:
Provides real-time allergy forecasts and tips to help manage allergic reactions that can affect the pharynx.
These resources offer a wealth of information and practical tools to help you manage and maintain your pharyngeal health effectively.
Frequently Asked Questions on the Pharynx
What is the primary role of the pharynx?
The pharynx is a critical component of the respiratory and digestive systems. It serves as a passageway for both air and food, aids in swallowing, and acts as a resonating chamber for vocalization while also playing an important role in immune defense.
How does the pharynx contribute to swallowing?
During swallowing, the pharynx coordinates muscle contractions to safely propel food from the mouth into the esophagus. The soft palate elevates to prevent nasal regurgitation, while the epiglottis covers the laryngeal inlet to protect the airway.
What are common causes of pharyngitis?
Pharyngitis is most commonly caused by viral infections, but bacterial infections such as strep throat, as well as allergens and irritants, can also lead to inflammation of the pharyngeal mucosa, resulting in a sore throat and discomfort.
How is obstructive sleep apnea related to pharyngeal function?
Obstructive sleep apnea occurs when the pharyngeal airway becomes partially or completely blocked during sleep. This blockage, often due to relaxed pharyngeal muscles, results in interrupted breathing, snoring, and daytime fatigue.
What lifestyle changes can improve pharyngeal health?
Maintaining good hydration, practicing proper oral hygiene, avoiding smoking and excessive alcohol, using a humidifier, and managing acid reflux through diet and weight control are key strategies to support and improve pharyngeal health.
Disclaimer: The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a healthcare provider for any concerns regarding your health.
Please share this article on Facebook, X (formerly Twitter), or your preferred social media platform to help spread awareness about pharyngeal health and modern treatment strategies.