The pituitary gland, often called the “master gland,” is a small, pea-sized organ that plays a critical role in regulating the body’s endocrine system. Nestled within the sella turcica at the base of the skull, it governs growth, metabolism, reproduction, and stress responses through its intricate network of hormone secretions. Its close functional relationship with the hypothalamus forms the hypothalamic-pituitary axis, essential for maintaining homeostasis. Understanding the anatomy, physiology, and common disorders of the pituitary gland is key to managing various hormonal imbalances and achieving overall well-being. This guide provides in-depth insights into the pituitary gland, along with practical treatment options and lifestyle tips.
Table of Contents
- Anatomical Insights and Structure
- Physiological Mechanisms and Functions
- Common Disorders and Conditions
- Diagnostic Methods and Assessments
- Treatment Approaches and Therapies
- Nutritional Support and Supplementation
- Preventative Care and Healthy Practices
- Trusted Resources and Further Reading
- Frequently Asked Questions
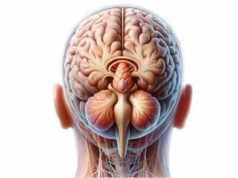
Anatomical Insights and Structure
The pituitary gland is a small, oval-shaped endocrine organ weighing about 0.5 grams and measuring roughly 1 centimeter in diameter. Housed within the bony confines of the sella turcica—a depression in the sphenoid bone at the skull’s base—it is uniquely positioned to communicate directly with the hypothalamus via the pituitary stalk (infundibulum). This intimate anatomical relationship enables the hypothalamus to regulate the gland’s hormone production efficiently.
Anatomical Divisions
The gland is traditionally divided into two distinct lobes:
- Anterior Pituitary (Adenohypophysis):
Constituting approximately 80% of the gland’s mass, the anterior pituitary is further subdivided into three regions: the pars distalis, pars tuberalis, and pars intermedia. - Pars Distalis:
This is the largest portion and is responsible for producing a variety of hormones. It contains several specialized cell types:- Somatotrophs: Secrete growth hormone (GH), crucial for somatic growth and metabolic regulation.
- Lactotrophs: Produce prolactin (PRL), essential for lactation and reproductive functions.
- Corticotrophs: Secrete adrenocorticotropic hormone (ACTH), which stimulates cortisol production from the adrenal cortex.
- Thyrotrophs: Release thyroid-stimulating hormone (TSH), which controls thyroid gland activity.
- Gonadotrophs: Produce luteinizing hormone (LH) and follicle-stimulating hormone (FSH), which regulate reproductive processes.
- Pars Tuberalis:
A thin layer of cells encasing the pituitary stalk, primarily involved in vascular support and minor hormone production. - Pars Intermedia:
A slender transitional zone that lies between the anterior and posterior lobes; in humans, it is less pronounced but can secrete melanocyte-stimulating hormone (MSH) in some species. - Posterior Pituitary (Neurohypophysis):
An extension of the hypothalamus, the posterior pituitary stores and releases hormones synthesized in the hypothalamic neurons. It primarily releases: - Antidiuretic Hormone (ADH): Regulates water balance in the kidneys.
- Oxytocin: Facilitates uterine contractions during labor and milk ejection during breastfeeding, and plays a role in social bonding.
Blood Supply and Innervation
The pituitary gland receives an abundant blood supply from branches of the internal carotid arteries:
- Superior Hypophyseal Arteries:
These vessels supply the median eminence and upper pituitary stalk, forming a capillary network that delivers hypothalamic hormones to the anterior pituitary via the hypophyseal portal system. - Inferior Hypophyseal Arteries:
These supply the posterior pituitary, ensuring efficient release of ADH and oxytocin into systemic circulation.
Innervation, primarily from the hypothalamus, involves autonomic fibers that modulate hormone release. This robust vascular and neural network is essential for the gland’s role as the body’s central endocrine regulator.
Histological Structure
Histologically, the anterior and posterior lobes exhibit distinct cellular organizations:
- Anterior Pituitary:
Composed of epithelial cells arranged in clusters, the anterior pituitary shows varied staining properties that help identify different hormone-producing cells. Acidophils (somatotrophs and lactotrophs) and basophils (corticotrophs, thyrotrophs, and gonadotrophs) are interspersed with chromophobes, which appear less active. - Posterior Pituitary:
Contains unmyelinated nerve fibers terminating in a rich capillary plexus. Supportive pituicytes (glial cells) maintain the local environment for hormone storage and release.
Embryological Development
The pituitary gland originates from two embryological sources:
- Rathke’s Pouch:
An ectodermal outpouching from the primitive oral cavity that gives rise to the anterior pituitary. - Neuroectoderm:
The posterior pituitary develops from the downward extension of the diencephalon’s neuroectoderm.
This dual origin establishes the gland’s complex structure and diverse functions, as it integrates neuroendocrine regulation with systemic hormone distribution.
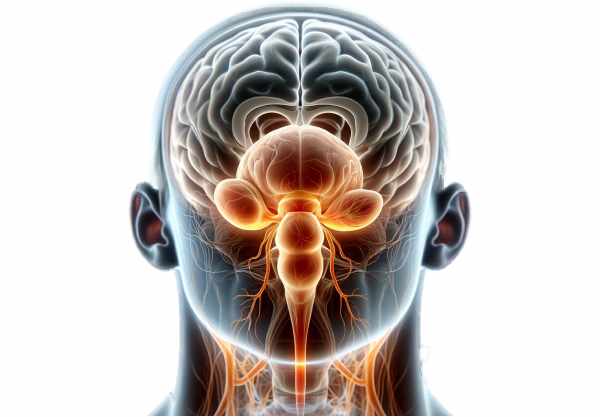
Physiological Mechanisms and Functions
The pituitary gland orchestrates a multitude of bodily processes by releasing hormones that act on peripheral endocrine glands and target tissues. Its activities are integral to growth, metabolism, stress responses, reproductive function, and water balance.
Regulation of Growth and Development
Growth Hormone (GH):
Secreted by somatotrophs in the anterior pituitary, GH plays a vital role in stimulating tissue growth, muscle and bone development, and metabolic regulation. Its actions are mediated through the production of insulin-like growth factor 1 (IGF-1), which promotes cellular growth and differentiation.
Reproductive Function
Gonadotropins (LH and FSH):
The anterior pituitary produces LH and FSH from gonadotrophs, which are essential for regulating reproductive processes in both males and females. In females, FSH supports follicular development and estrogen production, while LH triggers ovulation and supports the corpus luteum. In males, these hormones are critical for spermatogenesis and testosterone production.
Prolactin (PRL):
Produced by lactotrophs, prolactin is primarily involved in stimulating milk production postpartum. It also plays roles in reproductive health and modulating the immune system.
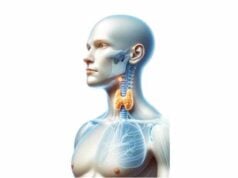
Metabolic and Energy Regulation
Thyroid-Stimulating Hormone (TSH):
Thyrotrophs in the anterior pituitary release TSH, which acts on the thyroid gland to stimulate the synthesis and release of thyroid hormones (T3 and T4). These hormones are crucial for regulating metabolic rate, energy production, and overall growth.
Stress Response and Cortisol Production
Adrenocorticotropic Hormone (ACTH):
Corticotrophs secrete ACTH, which stimulates the adrenal cortex to produce cortisol. Cortisol is a glucocorticoid that plays a central role in the stress response, affecting metabolism, immune response, and energy regulation. Its release is tightly controlled to balance the body’s response to stress.
Water and Blood Pressure Regulation
Antidiuretic Hormone (ADH):
Released by the posterior pituitary, ADH is essential for maintaining water balance. It acts on the kidneys to increase water reabsorption, reducing urine output and helping to regulate blood pressure.
Uterine Contraction and Milk Ejection
Oxytocin:
Also produced by the posterior pituitary, oxytocin is critical for reproductive functions. It induces uterine contractions during labor and stimulates the milk ejection reflex during breastfeeding. Oxytocin additionally fosters social bonding and maternal behaviors.
Neuroendocrine Integration
The pituitary gland serves as the central conduit for the hypothalamic-pituitary axis, linking the nervous system to the endocrine system. The hypothalamus secretes releasing and inhibiting hormones that travel through the hypophyseal portal system to modulate anterior pituitary hormone secretion. This integration ensures that the body’s hormonal output is synchronized with internal and external stimuli, maintaining homeostasis and adapting to changing conditions.
Common Disorders and Conditions
A variety of disorders can affect the pituitary gland, often leading to significant hormonal imbalances and a broad spectrum of clinical symptoms. These conditions may arise from tumors, genetic defects, inflammation, or secondary effects from other diseases.
Pituitary Tumors (Adenomas)
Pituitary adenomas are the most common pituitary disorders. Although generally benign, their impact on hormone secretion can lead to diverse clinical syndromes:
- Prolactinomas:
The most frequent type, these tumors secrete excessive prolactin, causing symptoms such as galactorrhea, amenorrhea in women, and sexual dysfunction in men. - Growth Hormone-Secreting Adenomas:
Overproduction of GH results in acromegaly in adults—characterized by enlarged extremities, facial changes, and metabolic disturbances—and gigantism in children. - ACTH-Secreting Adenomas:
These cause Cushing’s disease by stimulating excess cortisol production, leading to obesity, hypertension, diabetes, and osteoporosis. - TSH-Secreting Adenomas:
Rare tumors that produce excess TSH, causing hyperthyroidism with symptoms such as weight loss, rapid heartbeat, and nervousness. - Non-Functioning Adenomas:
Tumors that do not secrete hormones but may cause mass effects, such as headaches, visual disturbances (especially bitemporal hemianopia), and hypopituitarism due to compression of normal pituitary tissue.
Hypopituitarism
Hypopituitarism is a condition characterized by reduced hormone production by the pituitary gland. It can be partial (selective hormone deficiencies) or complete (panhypopituitarism) and may result from:
- Tumors:
Either due to direct compression or following treatment of pituitary adenomas. - Trauma or Surgery:
Injury to the gland during cranial surgery or head trauma. - Radiation Therapy:
Damage from radiation for other brain tumors. - Infiltrative Diseases:
Such as hemochromatosis or sarcoidosis.
Symptoms vary depending on which hormones are deficient, ranging from fatigue and weight loss to reproductive issues and cold intolerance.
Diabetes Insipidus
Diabetes insipidus (DI) is characterized by an inability of the kidneys to conserve water due to insufficient ADH secretion (central DI) or renal resistance to ADH (nephrogenic DI). Central DI, linked to pituitary or hypothalamic damage, results in excessive urination and intense thirst, risking dehydration if untreated.
Hyperprolactinemia
Excessively high prolactin levels, often due to prolactinomas, can lead to reproductive dysfunction. In women, hyperprolactinemia may cause menstrual irregularities, infertility, and inappropriate lactation; in men, it can result in decreased libido, erectile dysfunction, and infertility.
Empty Sella Syndrome
Empty sella syndrome occurs when the pituitary gland is either partially or completely flattened within the sella turcica. This condition may be primary (congenital) or secondary to pituitary surgery, radiation, or apoplexy. It can be asymptomatic or associated with hormonal deficiencies.
Pituitary Apoplexy
A rare but life-threatening condition, pituitary apoplexy is characterized by sudden hemorrhage or infarction of the pituitary gland, often in the setting of an existing adenoma. Rapid onset of severe headache, visual disturbances, altered consciousness, and hormonal imbalances necessitate urgent medical intervention.
Genetic and Inherited Disorders
Certain genetic syndromes affect pituitary function:
- Congenital Hypopituitarism:
Genetic mutations can impair pituitary development, leading to lifelong hormone deficiencies. - Multiple Endocrine Neoplasia (MEN) Syndromes:
These hereditary disorders predispose individuals to tumors in multiple endocrine glands, including the pituitary.
Diagnostic Methods and Assessments
Accurate diagnosis of pituitary disorders relies on a comprehensive approach combining clinical evaluation, laboratory testing, imaging studies, and specialized procedures.
Clinical Evaluation
A thorough history and physical examination are the first steps:
- Medical History:
The clinician collects detailed information regarding symptoms such as headaches, visual changes, fatigue, menstrual irregularities, sexual dysfunction, and growth abnormalities. Past history of head trauma, surgery, or radiation is also considered. - Physical Examination:
A complete neurological and endocrine evaluation is performed. Special attention is given to visual field testing to detect potential compression of the optic chiasm, which may manifest as peripheral vision loss.
Laboratory Tests
Hormonal assays are central to evaluating pituitary function:
- Basal Hormone Levels:
Blood tests measure levels of GH (via IGF-1), prolactin, ACTH, cortisol, TSH, thyroid hormones, LH, FSH, and ADH. These values help identify deficiencies or excesses. - Dynamic Testing:
Stimulation and suppression tests are used to assess the functional reserve of the pituitary: - ACTH Stimulation Test: Evaluates adrenal response.
- Dexamethasone Suppression Test: Assesses cortisol feedback mechanisms.
- Glucose Tolerance Test: Used to diagnose acromegaly by measuring GH suppression.
- Tumor Marker Analysis:
In cases of suspected germ cell tumors, markers such as alpha-fetoprotein (AFP) and beta-human chorionic gonadotropin (β-hCG) are measured.
Imaging Studies
Imaging is indispensable for visualizing the pituitary and its surroundings:
- Magnetic Resonance Imaging (MRI):
MRI is the gold standard for evaluating pituitary lesions, offering high-resolution images that reveal tumor size, location, and effects on adjacent structures. - Computed Tomography (CT):
CT scans are useful for detecting calcifications, bony erosion of the sella turcica, and when MRI is contraindicated. - Visual Field Testing:
Perimetry tests assess for visual field defects, which can indicate mass effect on the optic chiasm.
Additional Diagnostic Techniques
- Inferior Petrosal Sinus Sampling:
A specialized procedure for patients with Cushing’s syndrome to differentiate between pituitary and ectopic sources of ACTH. - Genetic Testing:
Performed in cases of suspected congenital hypopituitarism or MEN syndromes to identify specific genetic mutations. - Bone Density Testing:
DEXA scans evaluate bone mineral density, particularly in patients with long-term hormonal imbalances.
Treatment Approaches and Therapies
Management of pituitary disorders is highly individualized, depending on the nature and severity of the condition. Therapeutic strategies range from medical management to surgical intervention and radiation therapy, often integrated into a multimodal approach.
Medical Management
Hormone Replacement Therapy
For patients with hypopituitarism, hormone replacement is critical:
- Corticosteroids:
Synthetic corticosteroids such as hydrocortisone or prednisone replace deficient cortisol. - Thyroid Hormone Replacement:
Levothyroxine is administered to address TSH deficiency. - Growth Hormone Replacement:
Somatropin is used in children with growth delays and adults with GH deficiency. - Sex Hormone Replacement:
Estrogen/progesterone in women and testosterone in men correct reproductive hormone deficiencies. - Desmopressin:
Used in central diabetes insipidus to mimic ADH, reducing urine output and alleviating thirst.
Pharmacotherapy for Specific Adenomas
- Dopamine Agonists:
Bromocriptine and cabergoline lower prolactin levels in prolactinomas, often reducing tumor size. - Somatostatin Analogues:
Octreotide and lanreotide inhibit GH secretion, beneficial in acromegaly. - GH Receptor Antagonists:
Pegvisomant blocks GH receptors to counteract the effects of excess GH in acromegaly.
Surgical Intervention
Surgery is the primary treatment for many pituitary adenomas, particularly when there is mass effect or resistance to medical therapy.
- Transsphenoidal Surgery:
The most common approach, accessing the gland through the nasal cavity and sphenoid sinus. This minimally invasive technique reduces recovery time and minimizes damage to surrounding tissues. - Craniotomy:
Employed when tumors are large, invasive, or not amenable to the transsphenoidal route.
Radiation Therapy
When surgery and medical therapy are insufficient, radiation can help control tumor growth:
- Conventional Radiation Therapy:
Multiple sessions of targeted radiation aim to reduce tumor size and slow progression. - Stereotactic Radiosurgery (SRS):
Techniques such as Gamma Knife or CyberKnife deliver high-dose radiation precisely to the tumor, sparing healthy tissue.
Innovative and Emerging Treatments
Recent advances offer new avenues for managing pituitary disorders:
- Proton Beam Therapy:
An advanced form of radiation that uses protons for highly targeted tumor treatment. - Immunotherapy:
Experimental approaches aim to harness the immune system to target pituitary tumors. - Gene Therapy:
Research is ongoing into correcting genetic mutations underlying congenital pituitary dysfunction.
Nutritional Support and Supplementation
A balanced diet and targeted nutritional supplementation can support pituitary health and help regulate hormone levels. Dietary strategies not only bolster the endocrine system but also contribute to overall well-being.
Essential Nutrients
- Vitamin D:
Vital for bone health and immune regulation, vitamin D supports the function of the pituitary and other endocrine organs. - Omega-3 Fatty Acids:
Found in fish oil, these fatty acids reduce inflammation and support neural function. - B Vitamins (B6 and B12):
Crucial for energy metabolism and hormone synthesis, these vitamins help maintain optimal endocrine function. - Magnesium:
Essential for numerous enzymatic reactions, magnesium supports hormone production and overall cellular health. - Zinc:
A key mineral for immune and endocrine function, zinc plays a role in the synthesis and regulation of various hormones.
Antioxidants
Antioxidants protect the pituitary gland from oxidative stress:
- Vitamin C and E:
These vitamins neutralize free radicals and support cellular repair mechanisms. - Selenium:
An essential trace element with antioxidant properties, selenium contributes to maintaining endocrine health. - Glutathione:
The master antioxidant, glutathione, is critical for detoxification and cellular protection.
Herbal Supplements
Certain herbal supplements may promote endocrine balance:
- Ashwagandha:
An adaptogenic herb that helps mitigate stress and supports overall hormonal equilibrium. - Ginkgo Biloba:
Known to enhance blood circulation, it may indirectly benefit pituitary function. - Maca Root:
Traditionally used for hormonal balance, maca root can support overall endocrine health.
Melatonin Supplementation
Melatonin supplementation can assist with sleep regulation, which is essential for the pituitary’s rhythmic hormone secretion. Adequate sleep supports the entire endocrine system and improves overall well-being.
Integrating these nutrients through a varied, whole-food diet—rich in fruits, vegetables, lean proteins, and healthy fats—along with targeted supplementation, can help maintain and enhance pituitary gland function.
Preventative Care and Healthy Practices
Maintaining the health of the pituitary gland involves adopting a holistic approach that encompasses lifestyle, dietary habits, and regular health monitoring. Proactive steps can prevent hormonal imbalances and ensure overall endocrine stability.
Key Preventative Measures
- Balanced Nutrition:
Emphasize a nutrient-dense diet to support endocrine and overall health. - Regular Exercise:
Engage in physical activity to improve blood circulation, reduce stress, and promote hormonal balance. - Adequate Sleep:
Aim for 7–9 hours of quality sleep each night to support the pituitary’s circadian rhythm and hormone regulation. - Stress Management:
Utilize techniques such as meditation, yoga, and deep breathing to reduce chronic stress, which can disrupt hormonal balance. - Avoid Toxins:
Refrain from smoking and limit alcohol consumption, as these can adversely affect the endocrine system. - Regular Health Screenings:
Schedule routine check-ups and endocrine evaluations to detect and address hormonal imbalances early. - Weight Management:
Maintain a healthy weight to lower the risk of metabolic and endocrine disorders. - Hydration:
Stay adequately hydrated to support all cellular functions, including hormone synthesis. - Mindful Supplementation:
Consult with healthcare professionals before beginning any supplementation regimen.
By incorporating these preventative practices into your daily routine, you can safeguard your pituitary gland’s function, enhance overall hormonal balance, and improve long-term health outcomes.
Trusted Resources and Further Reading
Staying informed about pituitary health is essential for both patients and healthcare professionals. The following resources provide reliable, up-to-date information and serve as valuable tools for further education and support.
Recommended Books
- “Endocrine Physiology” by Patricia E. Molina:
A comprehensive resource covering the principles of endocrine function, including detailed chapters on the pituitary gland. - “Williams Textbook of Endocrinology” by Shlomo Melmed et al.:
An authoritative text on endocrine disorders, providing in-depth coverage of pituitary pathologies and treatment strategies. - “Pituitary Disorders: Diagnosis and Management” by Edward R. Laws Jr. and Stephanie L. Lee:
This book offers detailed insights into pituitary diseases, including clinical presentations and modern management techniques.
Academic Journals
- The Journal of Clinical Endocrinology & Metabolism (JCEM):
A leading journal that publishes cutting-edge research on endocrine disorders, including studies on pituitary gland function and treatment. - Endocrine Reviews:
Comprehensive reviews on the latest advancements in endocrine research, with a focus on hormonal regulation and pituitary disorders.
Mobile Applications
- MyHormones:
An app designed to help users track hormone levels, manage symptoms, and understand endocrine health. - Endocrine Society Clinical Practice Guidelines:
Provides access to the latest clinical guidelines and research for endocrinologists and patients alike. - MyFitnessPal:
A widely used app for tracking diet, exercise, and weight management, supporting overall endocrine well-being.
Frequently Asked Questions on the Pituitary Gland
What is the role of the pituitary gland in the body?
The pituitary gland, often termed the “master gland,” regulates numerous bodily functions by secreting hormones that influence growth, metabolism, reproduction, and stress responses. Its tight connection with the hypothalamus helps maintain overall endocrine balance.
How are pituitary disorders diagnosed?
Diagnosis typically involves a comprehensive approach including clinical evaluations, laboratory hormone assays, dynamic stimulation/suppression tests, and imaging studies such as MRI or CT scans, along with specialized tests like inferior petrosal sinus sampling when necessary.
What are common symptoms of pituitary tumors?
Symptoms of pituitary tumors can include headaches, visual disturbances (especially peripheral vision loss), hormonal imbalances (such as menstrual irregularities or sexual dysfunction), and signs of hypopituitarism, depending on the tumor type and size.
How is hypopituitarism managed?
Hypopituitarism is typically managed with hormone replacement therapy, where deficient hormones like cortisol, thyroid hormones, growth hormone, and sex hormones are supplemented to restore normal physiological functions.
Can lifestyle changes support pituitary gland health?
Yes, maintaining a balanced diet, engaging in regular physical activity, managing stress, ensuring adequate sleep, and avoiding harmful substances such as tobacco and excessive alcohol can support overall endocrine function and promote pituitary health.
Disclaimer: The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult with a healthcare provider for any concerns regarding your health.
Please share this article on Facebook, X (formerly Twitter), or your preferred social media platform to help spread awareness about pituitary gland health and the latest treatment strategies.