The prostate gland is a vital component of the male reproductive system, playing a central role in producing seminal fluid and maintaining urinary function. Despite its small size, this walnut-sized organ influences fertility, hormone metabolism, and overall health. Nestled beneath the bladder and surrounding the urethra, the prostate’s complex structure and proximity to critical pelvic organs mean that even subtle changes can have far-reaching effects. This guide provides an in-depth exploration of the prostate’s anatomy, key functions, common disorders, diagnostic techniques, modern treatment options, and lifestyle practices to help maintain optimal prostate health.
Table of Contents
- Prostate Structure and Anatomy
- Functional Roles and Mechanisms
- Common Disorders and Conditions
- Diagnostic Methods and Assessments
- Therapeutic Approaches and Treatments
- Nutritional Support and Supplementation
- Preventative Care and Healthy Habits
- Trusted Resources and Further Reading
- Frequently Asked Questions
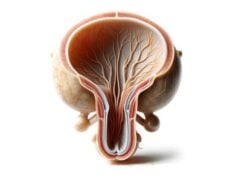
Prostate Structure and Anatomy
The prostate gland is an intricate organ comprised of both glandular and fibromuscular tissues. Located within the pelvic cavity, it forms a key part of the male reproductive system by encircling the proximal portion of the urethra. Its anatomical organization is crucial for its multiple functions, from contributing to seminal fluid production to affecting urinary control.
Macroscopic Anatomy
The prostate is typically described in terms of its zonal anatomy, which divides the gland into several distinct regions:
- Peripheral Zone:
This is the largest area, making up about 70% of the prostate’s volume. Situated at the back of the gland, it is the most common site for prostate cancer. This zone surrounds the distal urethra and is enclosed within the prostatic capsule. - Central Zone:
Accounting for roughly 25% of the prostate, the central zone encases the ejaculatory ducts. It is less frequently affected by inflammation or cancer compared to the peripheral region. - Transition Zone:
Making up about 5% of the prostate in younger men, this zone typically enlarges with age. Benign prostatic hyperplasia (BPH) most commonly arises from this area, leading to urinary difficulties by compressing the urethra. - Anterior Fibromuscular Zone:
This region consists of dense fibromuscular tissue, devoid of glandular components. It provides structural support and lies at the front of the prostate.
Microscopic Anatomy
At the cellular level, the prostate is characterized by a complex interplay between glandular elements and supportive stroma:
- Glandular Epithelium:
The prostate contains numerous acini (small sac-like structures) lined by secretory epithelial cells. These cells synthesize prostatic fluid, which is a key component of semen. Their secretions include enzymes, proteins, and minerals that enhance sperm motility and viability. - Stromal Component:
Surrounding the acini is the stroma, a dense mix of smooth muscle fibers, fibroblasts, collagen, and elastic fibers. During ejaculation, this fibromuscular stroma contracts to propel prostatic fluid into the urethra. - Ductal Network:
The prostatic ducts serve as conduits for transporting the secreted fluid from the acini to the prostatic urethra. The epithelial lining of these ducts transitions from columnar to stratified types as they approach the urethral lumen. - Capsular Layer:
The entire gland is encapsulated by a layer of fibrous tissue that demarcates it from the surrounding pelvic structures, providing both support and a barrier against disease spread.
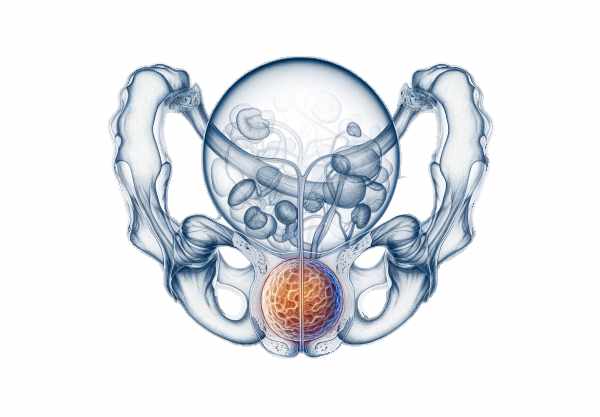
Vascular and Neural Supply
The prostate is richly supplied with blood and nerves, both of which are critical for its function:
- Blood Supply:
The inferior vesical artery, a branch of the internal iliac artery, provides the primary blood supply through several prostatic branches that penetrate the capsule. Venous drainage occurs via the prostatic venous plexus, which ultimately connects to the internal iliac veins. - Nerve Supply:
The autonomic nervous system innervates the prostate. Sympathetic fibers, originating from the hypogastric plexus, regulate the contraction of smooth muscle during ejaculation. Parasympathetic fibers, mainly from the pelvic nerve, control glandular secretion.
Surrounding Structures and Anatomical Relationships
The anatomical location of the prostate places it in close relation to several critical structures:
- Bladder:
The superior aspect of the prostate is contiguous with the bladder neck, impacting urinary function. - Seminal Vesicles:
These glands lie posterior to the bladder and superior to the prostate, contributing seminal fluid that mixes with prostatic secretions. - Rectum:
The prostate’s posterior surface is adjacent to the rectum, enabling digital rectal examination (DRE) for clinical evaluation. - Urethra:
The prostatic urethra, which runs centrally through the gland, serves as the common pathway for urine and semen.
Developmental Overview
The prostate gland originates during fetal development under the influence of androgens. It forms from embryonic tissue in the urogenital sinus and continues to grow and differentiate during puberty. In adulthood, the gland maintains a relatively stable size until later in life when benign growths or malignancies may develop.
Understanding the complex anatomy of the prostate is fundamental for diagnosing and treating prostate conditions. The zonal distinctions, cellular composition, and anatomical relationships are all key factors in clinical assessments and therapeutic strategies.
Functional Roles and Mechanisms
The prostate gland plays several vital roles in male reproductive and urinary systems, ensuring that semen is properly formed and that urinary functions remain efficient.
Production of Prostatic Fluid
The primary function of the prostate is the production of prostatic fluid, which constitutes about 20–30% of the total semen volume. This fluid is alkaline in nature, serving several key roles:
- Neutralization:
It counteracts the acidic environment of the female reproductive tract, providing a conducive medium for sperm survival. - Enzymatic Activity:
It contains enzymes like prostate-specific antigen (PSA) and acid phosphatase, which aid in the liquefaction of semen post-ejaculation. - Nutrient Supply:
The fluid is enriched with citrate, zinc, and other ions that provide energy and support sperm motility.
Ejaculatory Function
During ejaculation, the smooth muscle fibers in the prostatic stroma contract in a coordinated manner, expelling prostatic fluid into the urethra. This process is integral to the formation of semen, as prostatic secretions mix with sperm from the testes and fluids from the seminal vesicles.
Hormone Metabolism
The prostate also plays a role in the local metabolism of androgens:
- Conversion of Testosterone:
The enzyme 5-alpha reductase within the prostate converts testosterone to dihydrotestosterone (DHT), a more potent androgen that is essential for the maintenance and growth of the prostate. - Regulatory Role:
This conversion not only influences prostate size and function but also plays a part in the development of conditions like benign prostatic hyperplasia (BPH) and prostate cancer.
Urinary Function
Due to its anatomical proximity to the urethra, the prostate significantly influences urinary function:
- Urethral Support:
The prostate’s fibromuscular tissue helps maintain the integrity of the prostatic urethra, ensuring effective urinary flow. - Obstruction:
In conditions such as BPH, the enlarged prostate can impinge on the urethra, leading to urinary symptoms like hesitancy, weak stream, and incomplete bladder emptying.
Immune Protection
Prostatic fluid contains antimicrobial substances such as zinc, which help protect the male reproductive tract from infections. Additionally, the prostatic environment supports immune surveillance, playing a subtle yet important role in the body’s defense mechanisms.
Impact on Reproductive Health
By contributing to the formation of semen and facilitating the transport of sperm, the prostate gland is indispensable for male fertility. Its secretions optimize the seminal environment, enhancing sperm motility and viability, which are critical for successful fertilization.
Common Prostate Disorders
A range of disorders can affect the prostate, particularly as men age. These conditions vary in severity, from benign enlargements to malignant tumors, and can significantly impact quality of life.
Benign Prostatic Hyperplasia (BPH)
BPH is a non-cancerous enlargement of the prostate that typically occurs in men over 50. It results from the proliferation of prostate cells, especially in the transition zone, and leads to:
- Urinary Symptoms:
Frequent urination, nocturia (nighttime urination), hesitancy, weak stream, and incomplete bladder emptying. - Potential Complications:
If untreated, BPH may lead to urinary tract infections, bladder stones, or even acute urinary retention.
Prostatitis
Prostatitis refers to inflammation of the prostate and can be classified into several types:
- Acute Bacterial Prostatitis:
A sudden bacterial infection marked by high fever, chills, pelvic pain, and painful urination. Immediate antibiotic treatment is necessary. - Chronic Bacterial Prostatitis:
Characterized by recurrent infections that cause prolonged discomfort and urinary symptoms. - Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS):
The most common form, often non-bacterial, with symptoms including pelvic pain, urinary difficulties, and sexual dysfunction. - Asymptomatic Inflammatory Prostatitis:
Usually discovered incidentally during examinations for other conditions, this form may not present obvious symptoms but can be detected through laboratory tests.
Prostate Cancer
Prostate cancer is one of the most prevalent cancers among men, particularly in those over 65. Key points include:
- Risk Factors:
Age, family history, race (higher incidence in African-American men), and diet. - Symptoms:
Early stages may be asymptomatic, but advanced cancer can cause urinary difficulties, blood in urine or semen, pelvic pain, and bone pain due to metastasis. - Screening:
Regular PSA testing and digital rectal examinations (DRE) are crucial for early detection.
Elevated Prostate-Specific Antigen (PSA)
An increase in PSA levels may indicate various prostate conditions including BPH, prostatitis, or prostate cancer. However, PSA is not exclusively a marker for cancer and must be interpreted in conjunction with other clinical findings.
Prostate Cysts and Abscesses
- Prostate Cysts:
Typically benign and often asymptomatic, these fluid-filled sacs are usually discovered incidentally. In some cases, they may cause urinary obstruction or discomfort. - Prostate Abscesses:
A rare but serious condition involving a localized collection of pus within the prostate, leading to severe pain, fever, and systemic illness. They require prompt antibiotic therapy and sometimes surgical drainage.
Hormonal Imbalances
The prostate is highly sensitive to androgens. Abnormal levels of testosterone and DHT can contribute to the development of BPH and may play a role in prostate cancer progression. Hormonal therapies may be employed to modulate these levels in affected individuals.
Seminal Vesiculitis
Inflammation of the seminal vesicles can impact the prostate, causing symptoms such as pain during ejaculation, blood in semen, and lower abdominal discomfort. This condition is typically treated with antibiotics and anti-inflammatory medications.
Understanding these disorders is critical for early intervention, as many prostate conditions, when detected early, can be managed effectively to minimize complications and preserve quality of life.
Diagnostic Methods and Assessments
Accurate diagnosis of prostate conditions requires a multi-faceted approach that includes clinical evaluation, laboratory testing, imaging studies, and sometimes invasive procedures. These diagnostic tools help pinpoint the specific nature and severity of a disorder, guiding appropriate treatment.
Clinical Evaluation
- Medical History:
A comprehensive medical history is crucial, with a focus on urinary symptoms, pelvic discomfort, sexual dysfunction, and any family history of prostate disease. - Digital Rectal Examination (DRE):
A physician performs a DRE by inserting a gloved finger into the rectum to palpate the prostate. This exam helps detect irregularities in size, texture, and nodularity, which may indicate BPH or prostate cancer.
Laboratory Testing
- Prostate-Specific Antigen (PSA) Test:
Blood levels of PSA provide important clues about prostate health. Elevated levels can suggest BPH, prostatitis, or prostate cancer, though they are not definitive on their own. - Urinalysis:
Analysis of urine can reveal signs of infection or hematuria, supporting a diagnosis of prostatitis or other urinary tract conditions. - Semen Analysis:
This test examines the quality and quantity of sperm and seminal fluid, providing insight into the functional status of the prostate. - Hormonal Assays:
Blood tests to measure levels of testosterone, DHT, and other hormones can help assess hormonal imbalances that might affect the prostate.
Imaging Studies
- Transrectal Ultrasound (TRUS):
TRUS uses a specialized probe inserted into the rectum to generate images of the prostate. It is instrumental in measuring prostate volume, guiding biopsies, and evaluating structural abnormalities. - Magnetic Resonance Imaging (MRI):
Multiparametric MRI (mpMRI) offers high-resolution imaging to detect and characterize prostate lesions, especially in the context of suspected cancer. - Computed Tomography (CT) Scan:
Although less common for primary prostate evaluation, CT scans are useful for assessing metastatic spread in advanced prostate cancer. - Bone Scan:
This nuclear imaging technique helps identify skeletal metastases in patients with advanced prostate cancer.
Biopsy Procedures
- Transrectal Ultrasound-Guided Biopsy:
A needle biopsy, guided by TRUS, is the standard method for obtaining tissue samples for histological examination, particularly in suspected prostate cancer. - MRI-Targeted Biopsy:
Combining MRI imaging with ultrasound guidance, this approach enhances the detection of clinically significant tumors. - Transperineal Biopsy:
This method, which involves sampling tissue through the perineum, may reduce the risk of infection compared to the transrectal approach.
Urodynamic and Cystoscopic Evaluations
- Urodynamic Testing:
These tests assess bladder function and urine flow, which is critical in evaluating the impact of BPH on urinary function. - Cystoscopy:
A flexible or rigid scope is inserted through the urethra to visually inspect the bladder and urethra, aiding in the diagnosis of urethral obstruction or bladder abnormalities related to prostate enlargement.
Advanced Molecular and Genetic Testing
- Prostate Health Index (PHI) and 4Kscore:
These tests combine multiple biomarkers to improve the accuracy of prostate cancer risk assessment. - Genetic Testing:
In cases of familial prostate cancer or when genetic predispositions are suspected, testing for mutations such as BRCA1 and BRCA2 can provide valuable diagnostic and prognostic information.
By integrating these diagnostic techniques, clinicians can form a comprehensive picture of prostate health, enabling tailored treatment plans that address the specific nature and extent of any disorder.
Therapeutic Approaches and Treatments
The management of prostate disorders ranges from conservative medical treatment to invasive surgical procedures. Treatment strategies are tailored to the specific condition, its severity, and the patient’s overall health status.
Medical Therapies
Hormone Modulation and Replacement
- Hormone Replacement Therapy:
For patients with hypopituitarism or hormone deficiencies, replacement therapy may include corticosteroids, thyroid hormone, growth hormone, or sex hormones to restore normal function. - Androgen Deprivation Therapy (ADT):
For prostate cancer, ADT involves lowering androgen levels using LHRH agonists, anti-androgens, or estrogen therapy, which can slow tumor growth. - Dopamine Agonists:
Prolactinomas, which produce excessive prolactin, are effectively treated with medications like bromocriptine or cabergoline that reduce hormone levels and shrink tumor size. - Somatostatin Analogues and GH Receptor Antagonists:
These are used in managing growth hormone-secreting adenomas, such as in acromegaly, by inhibiting GH secretion or blocking its effects.
Alpha-Blockers and 5-Alpha Reductase Inhibitors
- Alpha-Blockers:
Medications such as tamsulosin, alfuzosin, and doxazosin relax smooth muscle fibers in the prostate and bladder neck, improving urine flow and reducing BPH symptoms. - 5-Alpha Reductase Inhibitors:
Finasteride and dutasteride work by reducing the conversion of testosterone to dihydrotestosterone (DHT), thereby decreasing prostate size and mitigating urinary symptoms associated with BPH.
Minimally Invasive Procedures
Transurethral Techniques
- Transurethral Resection of the Prostate (TURP):
A standard procedure for BPH, TURP involves the removal of excess prostate tissue via a resectoscope inserted through the urethra, significantly relieving urinary obstruction. - Transurethral Incision of the Prostate (TUIP):
TUIP involves making small incisions in the prostate to widen the urethral opening, offering a less invasive alternative to TURP for men with mild-to-moderate BPH. - Laser Therapies:
Procedures like holmium laser enucleation (HoLEP) and photoselective vaporization (PVP) use laser energy to remove or vaporize excess tissue, offering benefits such as minimal bleeding and quick recovery.
Novel Approaches
- Urolift System:
This innovative device uses small implants to retract obstructive prostate tissue away from the urethra, alleviating symptoms without removing tissue. - Transurethral Needle Ablation (TUNA):
TUNA uses radiofrequency energy delivered via needles to heat and destroy excess prostate tissue, providing symptom relief for BPH. - High-Intensity Focused Ultrasound (HIFU):
HIFU employs focused ultrasound waves to thermally ablate targeted prostate tissue, a non-invasive option for both BPH and localized prostate cancer.
Surgical Treatments
Radical and Conservative Surgery
- Radical Prostatectomy:
For localized prostate cancer, this surgery involves complete removal of the prostate gland and surrounding tissue. It can be performed through open, laparoscopic, or robotic-assisted techniques, with robotic surgery offering reduced recovery times and improved precision. - Cryotherapy:
This treatment freezes prostate tissue to destroy cancer cells and is used as an alternative for patients who are not candidates for surgery or radiation. - Brachytherapy:
Involves implanting radioactive seeds directly into the prostate to deliver a high dose of localized radiation, often used in early-stage prostate cancer.
Radiation Therapy
- External Beam Radiation Therapy (EBRT):
EBRT uses high-energy beams to target and destroy cancer cells. It can be used as a primary treatment or adjunctively with surgery. - Stereotactic Radiosurgery (SRS):
SRS, delivered by systems like Gamma Knife or CyberKnife, precisely targets the tumor with minimal damage to surrounding tissues, making it a popular choice for small or recurrent tumors.
Emerging and Innovative Treatments
- Proton Beam Therapy:
This advanced radiation therapy uses protons instead of X-rays, allowing for more precise targeting of tumor tissue while sparing surrounding healthy tissue. - Immunotherapy:
Agents such as sipuleucel-T (Provenge) harness the body’s immune system to attack prostate cancer cells, representing a promising approach for advanced prostate cancer. - Targeted Molecular Therapy:
Drugs such as PARP inhibitors target specific genetic mutations in prostate cancer, offering a more personalized and less toxic treatment option. - Cryoablation and Focal Therapies:
Minimally invasive procedures that aim to destroy cancerous tissue in a focal manner, preserving much of the prostate and reducing side effects.
The selection of treatment is highly individualized, based on the nature and stage of the disease, patient health, and personal preferences. A multidisciplinary team approach often yields the best outcomes for managing prostate disorders.
Nutritional Support and Supplementation
Diet and nutrition play an essential role in maintaining prostate health. A balanced diet rich in antioxidants, healthy fats, and essential vitamins can support hormonal balance and reduce the risk of prostate-related diseases. In addition, targeted supplementation may further enhance prostate function and protect against oxidative stress.
Essential Nutrients
- Vitamin D:
Crucial for immune regulation and overall endocrine function, vitamin D supports prostate health and may reduce the risk of prostate cancer. - Omega-3 Fatty Acids:
Found in fish oil, these anti-inflammatory fatty acids support cell membrane integrity and may lower the risk of prostate disease. - B Vitamins:
Vitamins such as B6 and B12 play key roles in energy metabolism and hormone synthesis, promoting optimal prostate function. - Magnesium:
This mineral is vital for enzymatic reactions and cellular function, aiding in hormone regulation and overall prostate health. - Zinc:
Zinc is essential for maintaining normal prostate function and immune health. Low zinc levels have been linked to an increased risk of BPH and prostate cancer.
Antioxidants
Antioxidants help neutralize free radicals and reduce oxidative stress, which is particularly important for prostate tissue.
- Vitamin C and E:
These vitamins protect cells from oxidative damage and support tissue repair. - Selenium:
An important trace element with antioxidant properties, selenium contributes to overall endocrine health. - Glutathione:
Often referred to as the master antioxidant, glutathione is critical for detoxification and cellular protection.
Herbal Supplements
Herbal supplements may offer natural support for prostate health:
- Saw Palmetto:
One of the most widely used supplements for managing BPH symptoms, saw palmetto can help improve urinary flow and reduce nighttime urination. - Beta-Sitosterol:
This plant sterol has been shown to alleviate urinary symptoms associated with BPH and improve overall prostate function. - Pygeum:
Extracted from the bark of the African cherry tree, pygeum has anti-inflammatory properties and can help manage both BPH and prostatitis. - Green Tea Extract:
Rich in polyphenols and catechins, green tea extract has antioxidant and anti-inflammatory effects that may reduce prostate cancer risk. - Lycopene:
A potent antioxidant found in tomatoes, lycopene is associated with a reduced risk of prostate cancer and promotes overall prostate health. - Pomegranate Extract:
High in antioxidants, pomegranate extract may slow prostate cancer progression and support cellular health. - Curcumin:
The active compound in turmeric, curcumin has strong anti-inflammatory and antioxidant properties that may benefit prostate health.
Melatonin Supplementation
Melatonin supports sleep regulation and may indirectly benefit prostate health by promoting hormonal balance and reducing oxidative stress. Adequate sleep is essential for the body’s overall endocrine function.
Integrating these nutrients and supplements into a balanced diet—emphasizing fruits, vegetables, lean proteins, and whole grains—can help maintain and enhance prostate function over the long term.
Preventative Care and Healthy Practices
Preventative strategies are key to maintaining optimal prostate health and reducing the risk of common prostate disorders. A holistic approach that includes lifestyle modifications, regular screenings, and proactive health management can preserve prostate function and enhance quality of life.
Dietary and Lifestyle Modifications
- Balanced Diet:
Focus on consuming nutrient-dense foods that are high in antioxidants, vitamins, and healthy fats. Incorporate tomatoes, berries, leafy greens, whole grains, and lean proteins to support overall prostate and endocrine health. - Hydration:
Drinking plenty of water supports urinary function and overall cellular health. - Regular Physical Activity:
Exercise improves blood circulation, aids in weight management, and reduces the risk of metabolic and prostate-related disorders. - Weight Management:
Maintaining a healthy body weight lowers the risk of BPH and prostate cancer, as obesity is linked to increased inflammation and hormonal imbalances.
Stress and Sleep
- Stress Management:
Techniques such as meditation, yoga, and deep breathing can lower stress levels, which may help prevent hormonal imbalances that affect the prostate. - Sleep Hygiene:
Aim for 7–9 hours of quality sleep per night. Good sleep supports the body’s hormonal rhythms and overall health.
Limiting Harmful Substances
- Avoid Smoking:
Smoking increases the risk of prostate cancer and exacerbates urinary symptoms. Quitting smoking is one of the most effective ways to protect prostate health. - Limit Alcohol and Caffeine:
Reducing the intake of alcohol and caffeine can help prevent irritation of the urinary tract and maintain a balanced hormonal environment.
Regular Medical Screening
- Routine Check-Ups:
Regular consultations with healthcare providers, including PSA testing and digital rectal examinations, are essential for early detection of prostate disorders. - Monitoring Symptoms:
Being aware of changes in urinary function, pelvic discomfort, or sexual performance can help catch issues early and allow for prompt intervention.
Environmental and Behavioral Considerations
- Stay Informed:
Keep up-to-date with the latest research and recommendations on prostate health. - Mindful Supplementation:
Consult healthcare professionals about incorporating supplements that support prostate health, ensuring that they complement your overall diet and lifestyle.
By adopting these preventative measures, you can support long-term prostate health, improve quality of life, and reduce the risk of developing prostate disorders.
Trusted Resources and Further Reading
For more information on prostate health, consider exploring the following trusted resources. These materials offer in-depth knowledge and practical guidance for both patients and healthcare professionals.
Books
- “The Whole Life Prostate Book: Everything That Every Man-at Every Age-Needs to Know About Maintaining Optimal Prostate Health” by H. Ballentine Carter, MD:
A comprehensive guide covering prevention, diagnosis, and treatment options for prostate health. - “Dr. Patrick Walsh’s Guide to Surviving Prostate Cancer” by Patrick C. Walsh, MD, and Janet Farrar Worthington:
This resource offers detailed insights into prostate cancer diagnosis, treatment options, and strategies for living with the disease. - “Prostate Health in 90 Days: Cure Your Prostate Naturally Using Nutrition, Supplements, Herbs, Exercise, and Other Natural Therapies” by Larry Clapp:
Focuses on natural approaches to improve and maintain prostate health through lifestyle and nutritional strategies.
Academic Journals
- The Journal of Urology:
A leading journal publishing research on prostate diseases, treatment modalities, and urological health. - Prostate Cancer and Prostatic Diseases:
This journal provides peer-reviewed articles on prostate cancer, benign conditions, and clinical advancements in prostate health.
Mobile Apps
- MyProstate:
An app that helps men track prostate health metrics, including PSA levels, symptoms, and appointments. - Urology Care Foundation’s Urology Health:
Offers educational resources and tools for understanding and managing prostate conditions. - WebMD:
A comprehensive health app that includes information, symptom checkers, and expert articles on prostate health.
Frequently Asked Questions on the Prostate Gland
What is the main function of the prostate gland?
The prostate gland produces prostatic fluid, a key component of semen that supports sperm viability and motility. It also plays a role in hormone metabolism and contributes to urinary function by surrounding the urethra.
What are common symptoms of prostate disorders?
Symptoms often include urinary frequency, hesitancy, weak stream, pelvic pain, and, in cases of cancer, blood in the urine or semen. Prostatitis may cause fever and discomfort, while BPH can lead to significant urinary issues.
How is prostate cancer detected?
Prostate cancer is typically detected through a combination of PSA testing, digital rectal examinations (DRE), and imaging studies such as MRI or transrectal ultrasound (TRUS), followed by a biopsy if needed.
What are the treatment options for benign prostatic hyperplasia (BPH)?
BPH treatment includes medications such as alpha-blockers and 5-alpha reductase inhibitors, minimally invasive procedures like TURP or laser therapy, and lifestyle modifications to improve urinary symptoms.
How can lifestyle changes support prostate health?
A balanced diet rich in antioxidants, regular exercise, adequate hydration, stress management, and avoiding smoking and excessive alcohol can all contribute to maintaining a healthy prostate.
Disclaimer: The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a healthcare provider for any concerns regarding your health.
Please share this article on Facebook, X (formerly Twitter), or your preferred social media platform to help spread awareness about prostate health and the latest treatment strategies.