The sebaceous glands are vital components of the skin, playing a crucial role in maintaining its health and protecting it from environmental challenges. These exocrine glands produce sebum—a lipid-rich substance that moisturizes the skin, prevents water loss, and serves as a first line of defense against pathogens. Found throughout the body, particularly on the face, scalp, and upper trunk, sebaceous glands are integral to our skin’s appearance and function. Their proper functioning is essential not only for dermatological health but also for preventing inflammatory conditions such as acne and seborrheic dermatitis. This guide provides an in-depth exploration of sebaceous gland anatomy, physiological roles, common disorders, diagnostic methods, treatment options, and practical tips for maintaining healthy skin.
Table of Contents
- Anatomical Structure & Histology
- Physiological Roles & Mechanisms
- Disorders & Conditions
- Diagnostic Techniques
- Treatment Strategies
- Nutritional Support & Supplementation
- Preventative Care & Healthy Practices
- Trusted Resources & Further Reading
- Frequently Asked Questions
Anatomical Structure & Histology
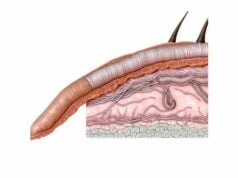
Sebaceous glands are specialized exocrine glands distributed throughout the skin, primarily associated with hair follicles, forming the pilosebaceous unit. They are responsible for the synthesis and secretion of sebum—a lipid-rich fluid that maintains skin moisture and acts as a barrier against microbial invasion.
Location and Distribution
Sebaceous glands are found in most parts of the body; however, their density and size vary significantly:
- High-Density Areas: The face (especially the forehead, nose, and chin), scalp, upper chest, and back house the largest and most active sebaceous glands.
- Low-Density Areas: In regions such as the palms, soles, and certain parts of the limbs, sebaceous glands are sparse or absent.
Gross Anatomy
The glands are typically microscopic in size, yet they collectively cover a large surface area. Each gland is composed of:
- Lobular Organization: Multiple lobules form a branched, alveolar structure. Each lobule contains clusters of acini—spherical structures that are the primary sites of sebum production.
- Ductal System: A single duct collects sebum from the lobules and directs it either into the hair follicle or directly onto the skin surface. In hair-bearing areas, these ducts usually open into the hair follicle, whereas in non-hairy regions, they open directly onto the epidermis.
Microscopic Features
Under the microscope, sebaceous glands reveal several distinctive histological characteristics:
- Sebocytes:
These specialized epithelial cells, known as sebocytes, are the functional units of the gland. They accumulate lipids in their cytoplasm as they mature. During holocrine secretion, sebocytes disintegrate entirely to release their lipid contents into the duct. - Basal Cells:
Surrounding the periphery of the gland, basal cells act as progenitors that continuously divide and differentiate into mature sebocytes. This regenerative capacity is essential for maintaining consistent sebum production. - Ductal Epithelium:
The ducts are lined by stratified squamous epithelium, which often keratinizes as it approaches the skin’s surface. This epithelial lining ensures that sebum is delivered effectively to the skin.
Vascular and Neural Supply
Sebaceous glands are well vascularized:
- Arterial Supply:
They receive nutrients from the surrounding dermal capillary networks that branch off from larger arteries supplying the skin. - Nerve Innervation:
Innervation is primarily autonomic. Sympathetic nerve fibers regulate glandular activity, responding to hormonal signals and stress, thereby modulating sebum production.
Hormonal Regulation
Sebaceous glands are highly sensitive to hormonal influences, particularly androgens:
- Androgens (Testosterone & DHT):
Androgens stimulate sebocyte differentiation and lipid synthesis. This explains the increase in sebum production during puberty and the hormonal fluctuations that contribute to acne. - Other Hormones:
Estrogens and progesterone can also affect sebaceous activity, although their impact is less pronounced compared to androgens.
Developmental Aspects
During embryogenesis, sebaceous glands arise from the same ectodermal tissue that forms hair follicles. Their development is intricately regulated by epithelial–mesenchymal interactions. By the fifth month of gestation, sebaceous glands are fully formed, with their activity modulated by hormonal changes occurring at puberty.
Physiological Roles & Mechanisms
The primary function of sebaceous glands is to produce sebum, a complex lipid mixture that is essential for skin and hair health. However, their roles extend into several vital physiological processes that contribute to the overall integrity and protection of the skin.
Sebum Production and Composition
Sebum is a complex fluid composed of:
- Lipids:
Including triglycerides, wax esters, squalene, and free fatty acids. These lipids are synthesized within sebocytes and stored until released. - Function of Sebum:
- Moisturization:
Sebum creates a hydrophobic barrier on the skin that prevents water loss, keeping the skin soft and supple. - Protection:
It serves as a barrier against environmental pollutants, microbial invasion, and UV radiation. - Antimicrobial Action:
Certain free fatty acids in sebum have antimicrobial properties, contributing to the skin’s innate defense mechanisms.
Holocrine Secretion
The unique process of holocrine secretion distinguishes sebaceous glands from other exocrine glands:
- Process:
As sebocytes mature, they accumulate lipids, and eventually, the entire cell disintegrates to release its contents. This process not only provides a continuous supply of sebum but also contributes cellular debris to the skin surface. - Regeneration:
Basal cells continuously replace the lost sebocytes, ensuring sustained gland function.
Role in Hair Health
Sebum produced by sebaceous glands is critical for:
- Lubrication of Hair:
Coating the hair shaft with sebum reduces friction, preventing breakage and promoting healthy hair texture. - Scalp Protection:
Sebum helps maintain the moisture balance of the scalp, reducing the risk of dandruff and seborrheic dermatitis.
Interaction with the Skin Microbiome
Sebum influences the skin’s microbial environment:
- Nutrient Source:
The lipids in sebum serve as nutrients for commensal bacteria, helping to maintain a balanced microbiome. - Antimicrobial Factors:
By providing antimicrobial free fatty acids, sebum helps keep pathogenic organisms in check, supporting overall skin health.
Thermoregulation
The lipid film created by sebum contributes to the skin’s barrier function, which plays a role in thermoregulation by:
- Reducing Evaporative Heat Loss:
A well-lubricated skin surface minimizes water loss and helps maintain stable skin temperature. - Protection Against Temperature Extremes:
The sebum layer offers a measure of insulation, protecting against cold and heat.
Hormonal Influence on Sebaceous Function
Hormones, particularly androgens, have a significant impact on sebaceous gland activity:
- Stimulation by Androgens:
Increased androgen levels during puberty lead to heightened sebum production, a common factor in acne development. - Modulatory Effects:
Other hormones, including estrogens and progesterone, can modulate sebaceous activity, affecting the overall oiliness and condition of the skin.
Disorders and Conditions
Sebaceous glands, while essential for skin health, are involved in a variety of common dermatological conditions. Abnormalities in sebum production or gland function can lead to disorders that affect both the appearance and health of the skin.
Acne Vulgaris
Acne vulgaris is the most prevalent condition associated with sebaceous gland dysfunction.
- Pathogenesis:
Excess sebum production, combined with abnormal keratinization and bacterial colonization (especially by Propionibacterium acnes), leads to clogged hair follicles and inflammation. - Lesion Types:
- Comedones: Open (blackheads) and closed (whiteheads) lesions formed by clogged follicles.
- Inflammatory Lesions: Papules, pustules, nodules, and cysts that result from immune responses to bacterial proliferation.
- Triggers:
Hormonal fluctuations, stress, diet, and genetic predisposition contribute to the severity and onset of acne.
Seborrheic Dermatitis
Seborrheic dermatitis is a chronic inflammatory skin condition affecting areas rich in sebaceous glands.
- Characteristics:
Red, greasy skin with flaky scales, often on the scalp (dandruff), face, and upper torso. - Etiology:
Factors include overgrowth of Malassezia yeast, excessive sebum production, and abnormal immune responses. - Impact:
This condition can cause itching, discomfort, and visible scaling, affecting quality of life and self-esteem.
Rosacea
Rosacea is a chronic inflammatory skin disorder that frequently affects the central face, where sebaceous glands are abundant.
- Manifestations:
Persistent redness, papules, pustules, and sometimes thickening of the skin (rhinophyma). - Exacerbating Factors:
Sun exposure, hot beverages, spicy foods, alcohol, and stress can worsen rosacea symptoms. - Subtypes:
Various forms exist, including erythematotelangiectatic, papulopustular, and phymatous, each with distinct clinical features.
Sebaceous Hyperplasia
Sebaceous hyperplasia involves the benign enlargement of sebaceous glands.
- Clinical Presentation:
Small, yellowish papules with a central depression, commonly found on the forehead, cheeks, and nose. - Etiology:
Often related to aging, hormonal changes, and prolonged sun exposure. - Significance:
Although typically harmless, sebaceous hyperplasia can be cosmetically distressing and may be mistaken for basal cell carcinoma.
Sebaceous Cysts
Sebaceous cysts (epidermoid or keratinous cysts) are benign, fluid-filled lesions that develop when a sebaceous gland or duct becomes blocked.
- Features:
They appear as firm, round nodules under the skin that may become inflamed or infected. - Management:
Treatment options range from conservative observation to surgical excision, especially if recurrent or symptomatic.
Hidradenitis Suppurativa
Though primarily affecting apocrine glands, hidradenitis suppurativa also involves sebaceous glands in affected regions.
- Symptoms:
Painful, recurrent nodules, abscesses, and sinus tracts primarily in the axillary, inguinal, and perianal areas. - Pathophysiology:
Chronic inflammation, follicular occlusion, and bacterial infection contribute to this debilitating condition.
Hyperseborrhea
Hyperseborrhea is characterized by the overproduction of sebum, resulting in oily skin and scalp.
- Clinical Effects:
Shiny, greasy skin; frequent need for hair washing; and potential exacerbation of acne. - Underlying Causes:
Hormonal imbalances, genetic predisposition, and environmental factors such as high humidity.
Sebaceous Carcinoma
Sebaceous carcinoma is a rare but aggressive malignancy originating in the sebaceous glands.
- Clinical Presentation:
Firm, painless nodules that may be yellowish and often occur on the eyelids but can also appear elsewhere. - Risk Factors:
More common in older adults and individuals with Muir-Torre syndrome, a genetic condition associated with various cancers. - Management:
Requires prompt surgical excision with clear margins, often accompanied by radiation therapy and, in some cases, chemotherapy.
Diagnostic Techniques and Testing
Accurate diagnosis of sebaceous gland disorders relies on a combination of clinical evaluation, imaging studies, laboratory tests, and specialized procedures. These methods enable clinicians to assess the nature and extent of the condition and guide effective treatment.
Clinical Assessment
- Medical History:
A detailed history is obtained regarding the onset, duration, and progression of skin lesions. Questions about previous treatments, family history, and associated symptoms (such as pain, itching, or swelling) are essential. - Physical Examination:
A thorough skin examination is conducted. Clinicians assess lesion characteristics (size, shape, color, texture) and distribution, and palpate affected areas to determine any underlying masses or tenderness.
Dermoscopy
Dermoscopy employs a handheld device that magnifies and illuminates the skin, allowing for detailed visualization of surface patterns and vascular structures. This non-invasive technique is useful for:
- Distinguishing benign conditions like sebaceous hyperplasia from malignant lesions.
- Assessing the morphology of cysts and nodules.
Biopsy and Histopathology
When clinical evaluation raises concerns:
- Skin Biopsy:
A sample of the affected tissue is removed using techniques such as punch, excisional, or incisional biopsy. Histopathological examination provides definitive diagnosis by revealing cellular details such as sebocyte structure, inflammatory infiltrates, and atypia. - Fine-Needle Aspiration (FNA):
FNA can be used for cystic or nodular lesions to obtain cells for cytological analysis, aiding in distinguishing benign from malignant processes.
Imaging Studies
Imaging techniques complement clinical assessments:
- Ultrasound:
High-frequency ultrasound imaging is particularly effective in evaluating the size, composition, and vascularity of sebaceous cysts and deep lesions. - Magnetic Resonance Imaging (MRI):
MRI provides high-resolution images of soft tissue structures and is beneficial when lesions are deep-seated or when malignancy is suspected. - Computed Tomography (CT):
CT scans are useful for identifying calcifications, particularly in conditions where excessive keratinization or chronic inflammation is present.
Laboratory Tests
Laboratory tests may support the diagnosis:
- Microbial Cultures:
When infection is suspected, cultures of exudate or cyst contents can identify bacterial or fungal pathogens. - Hormonal Assays:
In cases where hormonal imbalances are suspected (e.g., acne related to androgen excess), blood tests for testosterone and other relevant hormones may be conducted. - Inflammatory Markers:
Blood tests for markers like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) may indicate an underlying inflammatory process.
Advanced Molecular Techniques
For rare or complex cases:
- Immunohistochemistry (IHC):
IHC uses specific antibodies to detect proteins in tissue samples, aiding in the differentiation between benign and malignant lesions. - Fluorescence In Situ Hybridization (FISH):
This molecular technique identifies genetic abnormalities that may be associated with sebaceous carcinoma or other malignant processes. - Optical Coherence Tomography (OCT):
A non-invasive imaging technique that provides cross-sectional images of the skin at a microscopic level, useful for early detection of structural abnormalities in sebaceous glands.
Therapeutic Approaches and Treatments
The treatment of sebaceous gland disorders is highly variable and depends on the specific condition and its severity. Approaches range from conservative measures and topical therapies to advanced surgical procedures and emerging treatments.
Management of Acne Vulgaris
Acne vulgaris is often the result of overactive sebaceous glands, abnormal keratinization, and bacterial colonization.
- Topical Treatments:
- Retinoids: Tretinoin, adapalene, and tazarotene help regulate cell turnover and reduce clogged pores.
- Benzoyl Peroxide: This antimicrobial agent reduces Propionibacterium acnes and inflammation.
- Topical Antibiotics: Clindamycin and erythromycin help control bacterial growth.
- Oral Therapies:
- Antibiotics: Tetracyclines (e.g., doxycycline, minocycline) are prescribed for moderate to severe inflammatory acne.
- Hormonal Treatments: Oral contraceptives and anti-androgens such as spironolactone are effective in women.
- Isotretinoin: A potent oral retinoid that significantly reduces sebum production and is reserved for severe, recalcitrant cases.
- Procedural Treatments:
- Chemical Peels: Help exfoliate the skin and reduce acne lesions.
- Laser and Light Therapies: Target the sebaceous glands to reduce inflammation and bacterial load.
Treatment of Seborrheic Dermatitis
Seborrheic dermatitis, characterized by flaky, red, and oily skin, is managed through both topical and systemic therapies.
- Topical Antifungals:
Agents such as ketoconazole, ciclopirox, and selenium sulfide help control Malassezia yeast proliferation. - Topical Corticosteroids:
Low-potency steroids reduce inflammation and itching but should be used sparingly. - Non-Steroidal Alternatives:
Calcineurin inhibitors (tacrolimus, pimecrolimus) offer anti-inflammatory benefits without the side effects of steroids. - Medicated Shampoos:
Shampoos containing salicylic acid, tar, or antifungal agents help manage scalp involvement.
Management of Rosacea
Rosacea often involves inflammatory changes in the skin associated with sebaceous gland activity.
- Topical Agents:
Metronidazole, azelaic acid, and ivermectin reduce inflammation and improve the appearance of rosacea. - Oral Antibiotics:
Doxycycline or minocycline may be prescribed for moderate to severe cases. - Laser Treatments:
Vascular lasers help reduce persistent redness and visible blood vessels. - Lifestyle Modifications:
Avoiding known triggers such as hot beverages, spicy foods, and extreme temperatures can reduce flare-ups.
Treatment of Sebaceous Hyperplasia
Sebaceous hyperplasia is a benign condition characterized by enlarged sebaceous glands.
- Topical Retinoids:
Retinoids help normalize sebocyte turnover and reduce the appearance of hyperplasia. - Laser Therapy:
CO2 or erbium lasers can selectively target and reduce hyperplastic lesions. - Cryotherapy:
Liquid nitrogen can be used to freeze and reduce these benign lesions.
Management of Sebaceous Cysts
Sebaceous cysts are generally benign but may become inflamed or infected.
- Conservative Management:
If asymptomatic, cysts may simply be monitored. - Incision and Drainage:
For infected or painful cysts, a minor surgical procedure can release the cyst contents. - Excisional Surgery:
Complete removal of the cyst is performed in cases of recurrence or if there is cosmetic concern.
Treatment of Hidradenitis Suppurativa
Although primarily affecting apocrine glands, hidradenitis suppurativa often involves sebaceous gland dysfunction.
- Topical Treatments:
Antibiotic gels (e.g., clindamycin) help reduce inflammation. - Oral Antibiotics and Hormonal Therapies:
Combination regimens may be necessary for moderate to severe cases. - Biologic Agents:
TNF inhibitors such as adalimumab are used for refractory cases. - Surgical Interventions:
Incision, drainage, and wide excision may be required for chronic, severe lesions.
Management of Hyperseborrhea
Hyperseborrhea leads to an oily complexion and can exacerbate acne.
- Topical Antiseborrheic Agents:
Shampoos containing zinc pyrithione, selenium sulfide, or ketoconazole help reduce sebum production. - Systemic Medications:
In severe cases, isotretinoin may be prescribed to significantly lower sebaceous activity.
Treatment of Sebaceous Carcinoma
Sebaceous carcinoma is a rare, aggressive skin cancer.
- Surgical Excision:
The mainstay of treatment is complete surgical removal with clear margins. - Radiation Therapy:
Postoperative radiation is used to reduce the risk of recurrence. - Chemotherapy:
May be considered in metastatic or recurrent cases.
Nutritional Support and Supplementation
Optimal sebaceous gland health is supported by a balanced diet and targeted nutritional supplementation. Adequate nutrition helps regulate sebum production, reduce inflammation, and promote overall skin health.
Essential Nutrients
- Zinc:
Critical for immune function and regulation of sebaceous activity, zinc helps reduce inflammation and is often used in managing acne. - Vitamin A:
Vitamin A and its derivatives, such as retinoids, are essential for normal skin cell turnover and sebum regulation. - Omega-3 Fatty Acids:
Anti-inflammatory properties of omega-3s from fish oil or flaxseed oil can help reduce skin inflammation and improve acne. - B Vitamins (B6 and B12):
These vitamins support metabolic processes and skin health, contributing to proper gland function. - Magnesium:
Vital for numerous biochemical reactions, magnesium helps maintain cellular integrity and hormonal balance. - Vitamin E:
An antioxidant that protects the skin from oxidative damage and promotes healing.
Antioxidants
Antioxidants counteract free radicals and oxidative stress that can damage sebaceous glands:
- Vitamin C:
Helps in collagen synthesis and tissue repair. - Selenium:
A trace mineral that supports antioxidant defenses. - Glutathione:
The master antioxidant that is essential for detoxification and cellular protection.
Herbal and Natural Supplements
Herbal remedies may offer natural support for sebaceous gland function:
- Saw Palmetto:
Commonly used for hormonal regulation, saw palmetto may help reduce androgenic stimulation of sebaceous glands, thereby improving acne. - Green Tea Extract:
Rich in polyphenols, it offers potent anti-inflammatory and antioxidant benefits that may reduce sebum production. - Licorice Root:
Exhibits anti-inflammatory and antimicrobial properties, beneficial for conditions like acne and seborrheic dermatitis. - Turmeric (Curcumin):
Known for its strong anti-inflammatory effects, curcumin can alleviate inflammation in sebaceous gland disorders.
Probiotics
Maintaining a healthy gut microbiome with probiotics can have indirect benefits for skin health by reducing systemic inflammation and balancing the immune response.
Hydration and Electrolytes
Proper hydration is essential for overall skin health. Adequate water intake helps maintain the moisture balance of the skin and supports the function of sebaceous glands.
Preventative Care and Healthy Practices
Preventative strategies play a critical role in maintaining healthy sebaceous glands and overall skin wellness. Adopting a proactive approach can help mitigate common skin disorders and enhance the natural barrier functions of the skin.
Dietary and Lifestyle Modifications
- Hydration:
Consistently drinking water throughout the day supports optimal skin moisture and gland function. - Balanced Diet:
Consume a nutrient-rich diet high in fruits, vegetables, lean proteins, and whole grains. Antioxidant-rich foods like berries, tomatoes, and leafy greens help reduce inflammation. - Regular Exercise:
Physical activity improves blood circulation, reduces stress, and supports overall skin health. - Weight Management:
Maintaining a healthy weight can lower systemic inflammation and hormonal imbalances that affect sebum production.
Skincare and Oral Hygiene
- Gentle Cleansing:
Use mild cleansers suitable for your skin type to remove excess oil without stripping the skin of essential lipids. - Non-Comedogenic Products:
Choose skincare and cosmetic products labeled non-comedogenic to prevent clogged pores. - Regular Exfoliation:
Gentle exfoliation removes dead skin cells and helps prevent the buildup that can block sebaceous ducts. - Sun Protection:
Use a broad-spectrum sunscreen (SPF 30 or higher) to protect your skin from UV radiation, which can exacerbate oiliness and accelerate aging.
Behavioral and Environmental Factors
- Stress Management:
Employ stress-reduction techniques like meditation, yoga, and deep breathing exercises to help control hormonal fluctuations that affect sebum production. - Adequate Sleep:
Ensure 7–9 hours of quality sleep per night to support the body’s natural repair processes and hormonal balance. - Avoid Irritants:
Reduce exposure to harsh chemicals, extreme temperatures, and pollution that can disrupt skin homeostasis. - Regular Dermatological Check-Ups:
Early detection through routine skin examinations can help manage conditions like acne, seborrheic dermatitis, and other disorders before they worsen.
Consistent Skincare Routine
Developing a consistent skincare routine is essential:
- Morning and Evening Regimen:
Cleanse, tone, and moisturize regularly to maintain skin hydration and balance. - Targeted Treatments:
Use products containing retinoids, antioxidants, and anti-inflammatory ingredients as recommended by a dermatologist.
Trusted Resources and Further Reading
For additional information on salivary gland health and related topics, the following resources provide reliable, research-based insights and practical guidance:
Books
- “The Mouth-Body Connection: How Your Oral Health Affects Your Whole Body” by Dr. Gerald P. Curatola and Diane Reverand:
Explores the interconnection between oral health and overall well-being, highlighting the importance of healthy salivary glands. - “Essentials of Oral and Maxillofacial Surgery” by M. Anthony Pogrel, Karl-Erik Kahnberg, and Lars Andersson:
A comprehensive guide covering a range of oral disorders, including detailed sections on salivary gland pathology. - “Textbook of Salivary Gland Disorders” by Robert L. Witt:
Provides in-depth coverage of the diagnosis, treatment, and management of salivary gland conditions.
Academic Journals
- The Journal of Urology:
While focused on urology, this journal also publishes relevant research on salivary gland tumors and related conditions. - Prostate Cancer and Prostatic Diseases:
Though mainly on prostate topics, it occasionally covers comparative studies on glandular tumors and diagnostic techniques. - Oral Surgery, Oral Medicine, Oral Pathology, and Oral Radiology:
A peer-reviewed journal offering extensive research on oral and salivary gland disorders.
Mobile Apps
- MySwallowing Aid:
An app designed to help users with swallowing issues, indirectly supporting salivary gland function. - Urology Care Foundation’s Urology Health:
Provides educational resources on oral and glandular health. - WebMD:
A comprehensive health app that includes information on salivary gland disorders, treatment options, and expert advice.
Frequently Asked Questions on Sebaceous Glands
What is the primary function of sebaceous glands?
Sebaceous glands produce sebum, a lipid-rich substance that lubricates and moisturizes the skin and hair, provides a protective barrier against environmental aggressors, and possesses antimicrobial properties to help prevent infections.
How do sebaceous glands contribute to skin health?
By secreting sebum, sebaceous glands maintain skin hydration, protect against water loss, support the skin’s barrier function, and regulate the growth of skin microflora, all of which are essential for healthy, resilient skin.
What causes acne related to sebaceous gland dysfunction?
Acne often arises from excessive sebum production, abnormal shedding of skin cells, and bacterial overgrowth in hair follicles, leading to clogged pores, inflammation, and the formation of comedones, papules, and pustules.
How can I manage oily skin due to hyperactive sebaceous glands?
Managing oily skin involves using gentle cleansers, non-comedogenic skincare products, topical retinoids, and antioxidants, along with lifestyle modifications like a balanced diet, stress reduction, and adequate hydration.
Can supplements help improve sebaceous gland function?
Yes, supplements such as zinc, vitamin A, omega-3 fatty acids, and herbal extracts like saw palmetto and green tea extract can help regulate sebum production, reduce inflammation, and support overall skin health.
Disclaimer:
The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a healthcare provider for any concerns regarding your health.
Please share this article on Facebook, X (formerly Twitter), or your preferred social media platform to help spread awareness about salivary gland health and modern treatment strategies.