Smooth muscles play an essential role in regulating involuntary functions throughout the body. In this comprehensive guide, we delve into the intricate details of smooth muscle anatomy, explore the underlying mechanisms that drive smooth muscle functions, and examine common conditions that can affect these tissues. You’ll also discover a range of treatment options—from conventional therapies to cutting‐edge interventions—and learn valuable healthy tips for maintaining optimal smooth muscle health. Whether you’re a healthcare professional or someone seeking to improve personal wellness, this article provides a wealth of detailed, evidence‐based information to help you better understand smooth muscle anatomy and functions.
Table of Contents
- Anatomical Overview
- Functional Dynamics and Mechanisms
- Prevalent Disorders and Conditions
- Diagnostic and Evaluation Approaches
- Management and Therapeutic Options
- Nutritional and Supplemental Interventions
- Lifestyle and Wellness Guidelines
- Credible Sources and Further Reading
- Frequently Asked Questions
- Disclaimer & Sharing
Anatomical Overview
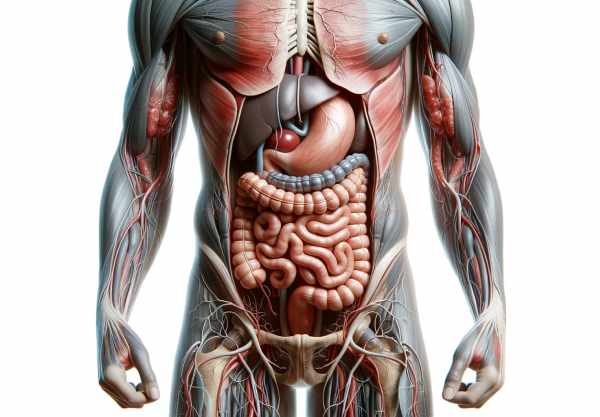
Smooth muscle tissue, unlike its striated counterparts, boasts a unique structure that enables the regulation of involuntary actions throughout various organ systems. This section delves into the detailed cellular and structural attributes of smooth muscles, exploring their microscopic architecture, organization, and widespread distribution within the body.
Cellular Architecture
Smooth muscle cells are specialized, spindle-shaped cells that play a pivotal role in the involuntary control of essential bodily functions. Their design is optimized for sustained contractions, vital for processes such as digestion and blood flow regulation. Here are key aspects of their cellular architecture:
- Shape and Dimensions:
Smooth muscle cells are elongated and tapered at both ends. Typically, their diameter ranges from 2 to 10 micrometers, while their length extends between 50 to 200 micrometers. This compact design facilitates precise, sustained contractions. - Nuclear Characteristics:
Each cell contains a single, centrally located nucleus that is elongated in shape, mirroring the cell’s overall design. The centrally placed nucleus supports cellular activities crucial for smooth muscle function. - Cytoplasmic Components:
The sarcoplasm, or cytoplasm, of smooth muscle cells houses typical organelles like mitochondria, the endoplasmic reticulum, and ribosomes. However, unlike skeletal muscle, smooth muscle cells lack an extensive sarcoplasmic reticulum network. This unique feature is integral to their regulation of contraction. - Contractile Proteins:
Actin and myosin filaments within smooth muscle cells are less organized than in striated muscles. Actin filaments attach to structures known as dense bodies, which serve a function similar to Z-lines in skeletal muscle, anchoring the contractile apparatus to the cell membrane via dense plaques. - Intermediate Filaments:
Proteins such as desmin and vimentin form intermediate filaments that provide structural support. These filaments connect dense bodies and plaques, ensuring the efficient transmission of contractile forces across the cell.
Structural Organization
Smooth muscle organization varies to meet the diverse functional demands of different organs. Two primary types are recognized:
- Single-Unit (Visceral) Smooth Muscle:
Also known as visceral smooth muscle, these cells are electrically connected by gap junctions. This connectivity allows the cells to contract in a synchronized fashion, a necessity in the coordinated activity required by hollow organs like the intestines, uterus, and bladder. - Multiunit Smooth Muscle:
In contrast, multiunit smooth muscle cells operate independently. They lack gap junctions, allowing for fine, individual control of contraction. This type is typically found in regions where precision is essential, such as in the iris of the eye, the arrector pili muscles in the skin, and certain large blood vessels.
Systemic Distribution
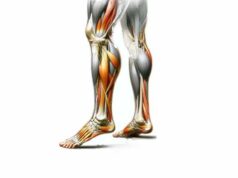
Smooth muscle tissue is found throughout the body, where it plays indispensable roles in various systems:
- Vascular System:
Smooth muscle cells are a major component of the tunica media in arteries and veins. Their contractile ability is critical for regulating blood vessel diameter, which in turn modulates blood pressure and flow dynamics. - Digestive System:
In the gastrointestinal tract, smooth muscles are arranged in two layers—the inner circular and outer longitudinal layers. Their coordinated contractions, known as peristalsis, propel food and waste through the digestive tract. - Respiratory System:
The bronchi and bronchioles contain smooth muscle cells that control airway diameter. This regulation is crucial in maintaining proper airflow during respiration and in response to allergens or environmental irritants. - Urinary System:
Smooth muscle fibers form the detrusor muscle of the bladder, facilitating the storage and expulsion of urine. Additionally, the ureters contain smooth muscle, which aids in the movement of urine from the kidneys to the bladder. - Reproductive System:
In females, the myometrium (uterine smooth muscle) plays a key role during childbirth, while in males, smooth muscle in the vas deferens assists in the transport of sperm. The proper functioning of these muscles is essential for reproductive health.
By understanding the intricate anatomical features and widespread distribution of smooth muscle tissue, we can appreciate its central role in maintaining the homeostasis of multiple body systems. This foundational knowledge is key for both clinical practice and everyday health awareness.
Functional Dynamics and Mechanisms
The functionality of smooth muscle tissue is characterized by its ability to contract and relax rhythmically, ensuring the seamless operation of numerous bodily systems. This section examines the physiological processes that underpin smooth muscle function, including the molecular mechanisms of contraction, the contributions of smooth muscles to various organ systems, and the ways in which these cells adapt to physiological changes.
Contraction and Relaxation Processes
Smooth muscle contraction is a finely tuned process that differs significantly from that of skeletal muscle. The sequence of events that leads to contraction involves multiple molecular players and regulatory pathways:
- Excitation–Contraction Coupling:
The contraction process is initiated by an increase in intracellular calcium (Ca²⁺). Calcium ions may enter the smooth muscle cell either from the extracellular space or be released from the sarcoplasmic reticulum. Once inside the cell, calcium binds to calmodulin, forming a Ca²⁺-calmodulin complex. - Activation of Contractile Machinery:
The Ca²⁺-calmodulin complex activates myosin light-chain kinase (MLCK), which in turn phosphorylates the myosin light chains. This phosphorylation enables the myosin heads to interact with actin filaments, leading to cross-bridge cycling and muscle contraction. - Relaxation Dynamics:
When intracellular calcium levels drop, the enzyme myosin light-chain phosphatase (MLCP) dephosphorylates the myosin light chains. This action interrupts the cross-bridge formation, allowing the muscle fibers to relax and return to their resting state.
These processes are vital for ensuring that smooth muscle tissues can contract and relax in response to varying physiological demands.
Organ System Contributions
Smooth muscles perform specialized roles in different organ systems, each tailored to the specific functional requirements of that system:
- Vascular Regulation:
In the circulatory system, smooth muscle contractions regulate blood vessel diameter. Through vasoconstriction and vasodilation, these muscles modulate blood pressure and ensure adequate tissue perfusion, which is crucial for overall cardiovascular health. - Gastrointestinal Motility:
The coordinated contractions of smooth muscle layers in the digestive tract facilitate peristalsis. This rhythmic motion is essential for moving food, digesting nutrients, and eventually eliminating waste, contributing to efficient digestive processes. - Respiratory Control:
Smooth muscles within the bronchi and bronchioles adjust airway diameter, thus controlling the flow of air into and out of the lungs. This dynamic regulation is particularly important in conditions like asthma, where airway constriction can impede breathing. - Urinary Function:
In the urinary system, smooth muscle contractions in the bladder allow for the controlled storage and expulsion of urine. The coordinated action of these muscles prevents incontinence and maintains proper urinary function. - Reproductive Processes:
The contraction of smooth muscle in the uterus (myometrium) is fundamental during childbirth, as it helps expel the fetus. In males, similar muscular contractions aid in the transport of sperm through the reproductive tract.
Autonomic and Endocrine Regulation
Smooth muscle activity is primarily regulated by the autonomic nervous system (ANS) and various hormones:
- Autonomic Control:
The sympathetic and parasympathetic branches of the ANS play distinct roles in modulating smooth muscle tone. Typically, sympathetic stimulation causes vasoconstriction and can inhibit gastrointestinal motility, while parasympathetic activation promotes vasodilation and enhances digestive processes. - Hormonal Influence:
A variety of hormones—such as adrenaline, angiotensin II, and oxytocin—bind to receptors on smooth muscle cells, triggering contraction or relaxation. These hormonal signals integrate with neural inputs to finely tune muscle activity in response to the body’s needs.
Adaptive Remodeling and Regeneration
Smooth muscle cells are remarkably adaptable, exhibiting a degree of plasticity that allows them to respond to various physiological and pathological stimuli:
- Hypertrophy and Hyperplasia:
In response to increased workload or injury, smooth muscle cells can undergo hypertrophy (an increase in cell size) or hyperplasia (an increase in cell number). This adaptability is essential for organs like the bladder, where muscle mass may increase to overcome obstructions. - Regenerative Capacity:
Unlike skeletal muscle cells, smooth muscle cells retain some regenerative ability. This regeneration is critical in repairing tissues that have been damaged by injury or disease, thereby maintaining organ integrity and function over time.
Understanding these functional dynamics offers valuable insight into how smooth muscles sustain vital bodily processes. Whether it’s regulating blood pressure, ensuring effective digestion, or adapting to chronic stressors, the mechanisms governing smooth muscle activity are central to maintaining overall health and homeostasis.
Prevalent Disorders and Conditions
While smooth muscles are essential for normal physiological functions, they can also be the site of various disorders that significantly affect quality of life. This section examines several common conditions associated with smooth muscle dysfunction, detailing their symptoms, underlying causes, and treatment approaches.
Irritable Bowel Syndrome (IBS)
Irritable Bowel Syndrome is a functional gastrointestinal disorder marked by chronic abdominal discomfort, bloating, and irregular bowel movements. The condition is believed to involve abnormal smooth muscle contractions in the intestines, which disrupt normal peristaltic movements.
- Causes:
IBS is multifactorial in origin, with potential contributors including gut-brain axis dysregulation, visceral hypersensitivity, altered gut motility, and changes in the gut microbiota. - Symptoms:
- Recurrent abdominal pain or cramping
- Bloating and excessive gas
- Alternating episodes of diarrhea and constipation
- Occasional presence of mucus in stools
- Treatment Strategies:
Management of IBS often involves dietary modifications (such as adopting a low FODMAP diet), the use of antispasmodic or antidiarrheal medications, and psychological therapies like cognitive behavioral therapy to manage stress and anxiety.
Asthma
Asthma is a chronic inflammatory disease of the airways characterized by episodes of wheezing, shortness of breath, and coughing. The condition is largely driven by hyperactivity of the smooth muscles surrounding the bronchi, leading to airway constriction.
- Causes:
Genetic predisposition, environmental allergens, respiratory infections, and physical exertion can all trigger asthma. Airway inflammation further exacerbates smooth muscle contraction. - Symptoms:
- Difficulty breathing, particularly during physical activity
- Wheezing and coughing, often worse at night
- Chest tightness, especially in the early morning hours
- Treatment Strategies:
Inhaled corticosteroids and bronchodilators form the cornerstone of asthma management, while long-term control medications and biologic therapies help reduce inflammation and prevent exacerbations.
Hypertension
Hypertension, commonly known as high blood pressure, is frequently linked to an increased tone of smooth muscle within the arterial walls. This elevated muscle tone reduces vessel diameter, resulting in increased resistance and persistently high blood pressure.
- Causes:
Hypertension is associated with a combination of genetic factors, high salt intake, obesity, sedentary lifestyle, and chronic stress. - Symptoms:
Often referred to as the “silent killer,” hypertension may remain asymptomatic for years. When symptoms do occur, they may include headaches, shortness of breath, nosebleeds, and visual disturbances in severe cases. - Treatment Strategies:
Effective management typically involves lifestyle modifications—such as a heart-healthy diet, regular physical activity, and weight loss—coupled with medications like ACE inhibitors, beta blockers, diuretics, and calcium channel blockers.
Dysmenorrhea
Dysmenorrhea refers to painful menstrual cramps resulting from abnormal or excessive contractions of uterine smooth muscle. This condition can severely impact quality of life, particularly during menstruation.
- Causes:
Primary dysmenorrhea is commonly linked to hormonal fluctuations during the menstrual cycle, whereas secondary dysmenorrhea may result from conditions such as endometriosis, fibroids, or pelvic inflammatory disease. - Symptoms:
- Intense lower abdominal pain that may radiate to the lower back and thighs
- Nausea, vomiting, and diarrhea in more severe cases
- Occasional headaches and fatigue
- Treatment Strategies:
Nonsteroidal anti-inflammatory drugs (NSAIDs) are typically used to alleviate pain, while hormonal treatments (such as oral contraceptives) and lifestyle changes, including exercise and heat therapy, offer additional relief.
Achalasia
Achalasia is a rare esophageal motility disorder in which the lower esophageal sphincter (LES) fails to relax properly, impeding the smooth passage of food from the esophagus to the stomach.
- Causes:
Although the precise cause remains unclear, nerve degeneration in the esophagus or an autoimmune response may contribute to the dysfunction of the LES. - Symptoms:
- Difficulty swallowing (dysphagia) for both solids and liquids
- Regurgitation of undigested food, leading to chest discomfort
- Unexplained weight loss and chest pain
- Treatment Strategies:
Treatment options include pneumatic dilation or surgical myotomy to relax the LES, along with medications such as nitrates and calcium channel blockers. Botox injections are also used to provide temporary relief by relaxing the esophageal muscles.
Raynaud’s Phenomenon
Raynaud’s phenomenon is characterized by episodic spasms of small arteries, primarily in the fingers and toes, which lead to reduced blood flow and noticeable color changes in the skin.
- Causes:
Primary Raynaud’s phenomenon is idiopathic, while secondary Raynaud’s is often associated with autoimmune conditions like scleroderma or lupus. - Symptoms:
- Color changes in the skin (white to blue to red) upon exposure to cold or stress
- Numbness, tingling, and pain in the affected extremities
- Occasional ulcers or sores in severe cases
- Treatment Strategies:
Management typically focuses on avoiding triggers such as cold exposure and stress, with medications like calcium channel blockers and vasodilators prescribed to improve blood flow. In extreme cases, surgical sympathectomy may be considered.
Uterine Fibroids
Uterine fibroids are benign tumors composed of smooth muscle cells that develop within the uterus. They are a common cause of abnormal bleeding and pelvic pain in women.
- Causes:
Hormonal imbalances—particularly involving estrogen and progesterone—combined with genetic predisposition contribute to the formation of fibroids. - Symptoms:
- Heavy menstrual bleeding and prolonged periods
- Pelvic pressure and pain
- Frequent urination and constipation due to pressure on surrounding organs
- Potential complications during pregnancy
- Treatment Strategies:
Options range from hormone-regulating medications (such as GnRH agonists and progestins) to minimally invasive procedures like uterine artery embolization and myomectomy. In severe or refractory cases, hysterectomy may be recommended.
The diverse spectrum of disorders affecting smooth muscles underscores the importance of early diagnosis and tailored treatment strategies to ensure optimal organ function and overall health.
Diagnostic and Evaluation Approaches
Accurate diagnosis is crucial for the effective management of smooth muscle disorders. A combination of clinical assessments, imaging modalities, functional tests, and laboratory investigations is used to evaluate the condition of smooth muscle tissue and guide appropriate treatment strategies.
Clinical Assessment
A comprehensive clinical evaluation is often the first step in diagnosing smooth muscle disorders:
- Medical History:
Detailed patient histories are obtained to identify symptoms, familial predispositions, and potential risk factors. Understanding the patient’s background is essential for forming a differential diagnosis. - Physical Examination:
Clinicians perform thorough physical examinations, assessing vital signs such as blood pressure, respiratory function, and abdominal tenderness, to detect any signs of smooth muscle dysfunction.
Imaging Modalities
Modern imaging technologies offer non-invasive methods to visualize internal structures and assess smooth muscle integrity:
- Ultrasound:
This technique employs high-frequency sound waves to generate images of internal organs. Ultrasound is particularly useful in examining abdominal organs, pelvic structures, and assessing uterine fibroids. - Computed Tomography (CT) Scan:
CT scans produce detailed cross-sectional images of the body, which are invaluable in evaluating vascular structures, gastrointestinal obstructions, and detecting potential tumors. - Magnetic Resonance Imaging (MRI):
MRI leverages magnetic fields and radio waves to provide high-resolution images of soft tissue structures. It is commonly used to assess the gastrointestinal tract, uterus, and blood vessels, offering precise detail without radiation exposure.
Endoscopic Examinations
Endoscopic procedures allow direct visualization of internal organ surfaces, aiding in the diagnosis of various smooth muscle disorders:
- Gastroscopy and Colonoscopy:
These procedures involve the insertion of flexible tubes equipped with cameras through the mouth or anus to inspect the gastrointestinal tract. They facilitate the diagnosis of conditions like IBS, Crohn’s disease, and even early-stage cancers. Additionally, tissue biopsies can be performed during these procedures. - Bronchoscopy:
In this procedure, a bronchoscope is introduced via the nose or mouth to visualize the airways. Bronchoscopy is particularly useful in diagnosing respiratory conditions associated with smooth muscle dysfunction, such as asthma and chronic bronchitis.
Functional Assessments
Functional tests provide quantitative data regarding the performance of smooth muscle tissues:
- Manometry:
This test measures pressure within the gastrointestinal tract or esophagus. It is essential in diagnosing motility disorders like achalasia, as it assesses the pressure dynamics of the smooth muscle layers. - Pulmonary Function Tests (PFTs):
PFTs evaluate lung capacity and airflow, helping to detect respiratory disorders such as asthma and COPD. They provide critical insights into the functional status of airway smooth muscle.
Laboratory Investigations
Laboratory tests further complement the diagnostic process:
- Blood Tests:
Routine blood panels, including complete blood counts (CBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) levels, help identify inflammatory markers and hormonal imbalances that may affect smooth muscle function. - Stool Analysis:
In gastrointestinal disorders, stool tests are performed to detect the presence of blood, pathogens, or inflammatory markers that could indicate underlying smooth muscle dysfunction.
Electrophysiological Evaluations
Electrophysiological tests offer insights into the electrical activity of muscle tissues:
- Electrocardiography (ECG):
While primarily used to assess cardiac function, ECG can also provide information about the electrical conduction in smooth muscle tissues of the heart. - Electromyography (EMG):
EMG is used less frequently for smooth muscle assessment but can yield valuable data regarding muscle electrical activity in certain diagnostic contexts.
Histopathological Analysis
Definitive diagnosis often requires microscopic examination of tissue samples:
- Tissue Biopsy:
A small sample of tissue is extracted from the affected organ. Biopsies are critical for diagnosing conditions such as gastrointestinal cancers, uterine fibroids, or autoimmune disorders affecting smooth muscle. - Histopathology:
Examining tissue samples under a microscope allows pathologists to detect cellular abnormalities, inflammatory changes, or malignancies. This step is pivotal for confirming a diagnosis and guiding subsequent treatment.
Through a combination of these diagnostic tools, healthcare professionals can accurately assess the condition of smooth muscle tissues and tailor interventions to each patient’s specific needs.
Management and Therapeutic Options
Treating smooth muscle disorders often requires a multifaceted approach that integrates lifestyle modifications, pharmacological treatments, and sometimes surgical interventions. In this section, we review several therapeutic strategies aimed at addressing common smooth muscle conditions, with an emphasis on both conventional treatments and emerging therapies.
Blood Pressure Management
Hypertension is a common manifestation of smooth muscle dysfunction within the vascular system. Effective management includes both lifestyle interventions and medication:
- Lifestyle Modifications:
- Dietary Adjustments: Adoption of a heart-healthy diet (such as the DASH diet) that emphasizes fruits, vegetables, whole grains, and lean proteins while limiting salt and saturated fats.
- Regular Exercise: Engaging in aerobic activities such as walking, cycling, or swimming helps reduce blood pressure and improve vascular health.
- Weight Control: Maintaining an optimal weight is crucial for lowering the workload on blood vessels.
- Pharmacological Interventions:
- Diuretics: Medications that promote the excretion of excess sodium and water, thereby reducing blood volume and pressure.
- ACE Inhibitors and Beta Blockers: These drugs help relax vascular smooth muscle, reducing arterial resistance.
- Calcium Channel Blockers: By preventing calcium influx into smooth muscle cells, these medications promote vasodilation and decrease blood pressure.
- Innovative Approaches:
Emerging treatments, such as renal denervation and baroreceptor activation therapy, offer promising alternatives for patients with resistant hypertension.
Asthma Control Strategies
Asthma management centers on reducing airway inflammation and controlling smooth muscle hyperactivity:
- Inhaled Medications:
- Corticosteroids: These reduce airway inflammation, limiting the frequency of asthma attacks.
- Bronchodilators: Short-acting agents provide rapid relief during an acute asthma attack, while long-acting formulations offer sustained control.
- Oral Medications and Biological Therapies:
- Leukotriene Modifiers and Theophylline: These help control inflammation and prevent bronchoconstriction.
- Monoclonal Antibodies: Targeted therapies such as omalizumab can reduce allergic responses, while others like mepolizumab diminish eosinophilic inflammation.
- Advanced Procedures:
- Bronchial Thermoplasty: This minimally invasive procedure uses controlled heat to reduce the mass of airway smooth muscle, thereby mitigating bronchoconstriction.
Uterine Fibroid Therapies
Uterine fibroids are managed through a range of treatments that aim to reduce symptoms while preserving uterine function when possible:
- Medical Management:
- Hormone-Modulating Drugs: GnRH agonists and progestins help reduce fibroid size and control heavy menstrual bleeding.
- Minimally Invasive Techniques:
- Uterine Artery Embolization (UAE): A procedure that cuts off the blood supply to fibroids, causing them to shrink.
- Myomectomy: Surgical removal of fibroids while conserving the uterus, often preferred by women seeking to maintain fertility.
- Surgical Interventions:
In severe cases, particularly when other treatments have failed, hysterectomy may be the most effective solution.
Interventions for Achalasia
Achalasia, characterized by impaired relaxation of the esophageal sphincter, is managed with both non-surgical and surgical approaches:
- Pharmacological Management:
Medications like nitrates and calcium channel blockers help relax the lower esophageal sphincter to improve swallowing. - Endoscopic Procedures:
- Pneumatic Dilation: Involves inflating a balloon within the esophagus to widen the sphincter.
- Botox Injections: Temporarily relax the LES by chemically denervating the muscle.
- Surgical Options:
- Heller Myotomy: A procedure that surgically cuts the LES muscles, facilitating easier passage of food.
- Peroral Endoscopic Myotomy (POEM): A less invasive endoscopic technique that achieves similar results.
Approaches for Raynaud’s Phenomenon
Raynaud’s phenomenon is primarily managed by alleviating symptoms and preventing episodes of vasospasm:
- Lifestyle Adjustments:
- Avoiding cold exposure and managing stress through relaxation techniques are crucial for symptom prevention.
- Medical Treatments:
- Calcium Channel Blockers and Vasodilators: These medications help dilate the blood vessels, reducing the frequency and severity of vasospastic episodes.
- Surgical Considerations:
In extreme cases, a sympathectomy may be considered to interrupt the nerve signals responsible for vasoconstriction.
By employing these targeted management strategies, healthcare providers can tailor treatments to individual patient needs, improving outcomes and enhancing the overall quality of life for those affected by smooth muscle disorders.
Nutritional and Supplemental Interventions
A balanced diet and the judicious use of nutritional supplements can play a crucial role in supporting smooth muscle health. The following supplements have been identified as beneficial for promoting muscle relaxation, reducing inflammation, and improving overall cellular function.
- Magnesium:
- Muscle Relaxation: Aids in reducing spasms and cramps by promoting muscle relaxation.
- Vasodilation: Supports the relaxation of vascular smooth muscles, thereby contributing to healthy blood pressure levels.
- Omega-3 Fatty Acids:
- Anti-Inflammatory Benefits: Reduces inflammation that can exacerbate smooth muscle disorders such as asthma and IBS.
- Cardiovascular Support: Enhances blood vessel function and helps in the regulation of blood pressure.
- Vitamin D:
- Immune Regulation: Helps modulate the immune response, reducing inflammatory processes in smooth muscle tissues.
- Muscle Function: Plays a vital role in maintaining normal muscle function and strength.
- Coenzyme Q10 (CoQ10):
- Antioxidant Properties: Protects smooth muscle cells from oxidative damage while supporting energy production.
- Cardiovascular Health: Enhances the function of blood vessels and contributes to overall heart health.
- Probiotics:
- Gut Health: Promote a balanced intestinal flora, which can help improve gastrointestinal smooth muscle function.
- Immune Enhancement: Support a robust immune system that is essential for maintaining gut integrity.
- L-Arginine:
- Vasodilation: Serves as a precursor to nitric oxide, a key molecule in relaxing blood vessels.
- Improved Endurance: Enhances muscle function by facilitating better blood flow and nutrient delivery.
- Turmeric (Curcumin):
- Anti-Inflammatory: Mitigates inflammatory responses, which is beneficial for conditions like IBS and dysmenorrhea.
- Antioxidant: Offers protective benefits against oxidative stress within smooth muscle cells.
- Ginger:
- Digestive Aid: Improves overall digestion and reduces nausea, contributing to smoother gastrointestinal function.
- Anti-Spasmodic Effects: Helps alleviate muscle spasms and discomfort.
- Peppermint Oil:
- Smooth Muscle Relaxation: Eases the contractions of gastrointestinal smooth muscles, offering relief from IBS symptoms.
- Pain Reduction: Acts as a natural remedy for abdominal pain and cramps.
- Aloe Vera:
- Soothing Properties: Calms the lining of the gastrointestinal tract, aiding in digestion and reducing inflammation.
- Overall Gut Support: Helps maintain the health of the gut mucosa, which is essential for proper smooth muscle function.
Integrating these supplements into a balanced nutritional plan can complement medical treatments and contribute significantly to the overall health of smooth muscle tissues.
Lifestyle and Wellness Guidelines
Beyond clinical treatments and nutritional supplements, adopting healthy lifestyle practices is paramount for maintaining smooth muscle function and overall well-being. The following guidelines provide actionable tips to support smooth muscle health across various systems in the body:
- Adopt a Balanced Diet:
Focus on a diet rich in fruits, vegetables, lean proteins, and whole grains. Such nutritional diversity ensures a steady supply of essential vitamins and minerals that bolster smooth muscle function. - Stay Hydrated:
Adequate water intake is crucial for maintaining muscle elasticity and preventing cramps. Aim to drink water consistently throughout the day. - Engage in Regular Physical Activity:
Consistent exercise—whether through walking, swimming, or cycling—supports cardiovascular health and improves the efficiency of smooth muscle contractions. Aim for at least 150 minutes of moderate-intensity activity weekly. - Manage Stress Effectively:
Techniques such as yoga, meditation, and deep-breathing exercises can alleviate stress, which in turn reduces the strain on smooth muscle tissues across the body. - Avoid Smoking:
Smoking impairs blood vessel function and can exacerbate smooth muscle dysfunction, particularly within the respiratory and cardiovascular systems. - Limit Alcohol Consumption:
Excessive alcohol intake may lead to muscle impairment and other health complications. Follow recommended guidelines to ensure moderation. - Prioritize Quality Sleep:
Aim for 7–9 hours of sleep per night to support cellular repair and muscle recovery. - Include Probiotic-Rich Foods:
Foods such as yogurt, kefir, and fermented vegetables help maintain a healthy gut microbiome, which is integral to the proper function of gastrointestinal smooth muscles. - Consume Magnesium-Rich Foods:
Incorporate leafy greens, nuts, seeds, and whole grains into your diet to provide natural sources of magnesium, which supports muscle relaxation and prevents cramping. - Schedule Regular Medical Check-Ups:
Routine visits to your healthcare provider can help monitor blood pressure and overall smooth muscle health, ensuring early detection and management of potential issues.
By embracing these lifestyle modifications, you can significantly enhance the function and resilience of smooth muscles, contributing to a healthier and more balanced life.
Credible Sources and Further Reading
For those seeking to deepen their understanding of smooth muscle health, a variety of credible resources are available. These books, academic journals, and mobile applications provide evidence-based insights and practical guidance on maintaining optimal smooth muscle function.
Books
- “The Magnesium Miracle” by Carolyn Dean:
Explores the essential role of magnesium in muscle function and overall health, offering practical advice on incorporating this nutrient into your diet. - “The Anti-Inflammatory Diet & Action Plans” by Dorothy Calimeris and Sondi Bruner:
Provides comprehensive meal plans and recipes aimed at reducing inflammation, benefiting both gastrointestinal and cardiovascular smooth muscle function. - “Asthma-Free Naturally” by Patrick McKeown:
Presents holistic approaches to managing asthma through dietary modifications, breathing techniques, and lifestyle changes, with a focus on improving airway smooth muscle function.
Academic Journals
- American Journal of Physiology – Cell Physiology:
Publishes high-quality research on cellular physiology, including studies on the mechanisms of smooth muscle contraction and regeneration. - Journal of Smooth Muscle Research:
Dedicated to the study of smooth muscle physiology and pathology, offering in-depth insights into the latest research findings and clinical applications.
Mobile Apps
- MyFitnessPal:
A comprehensive tool for tracking dietary intake and exercise routines, supporting overall health and indirectly benefiting smooth muscle function. - Calm:
Offers guided meditation and relaxation exercises to help manage stress levels, which is beneficial for maintaining proper smooth muscle tone. - Blood Pressure Monitor:
Enables regular tracking of blood pressure readings, aiding in the management of hypertension and the associated vascular smooth muscle conditions.
These resources serve as valuable guides for individuals looking to expand their knowledge and adopt practices that promote smooth muscle health.
Frequently Asked Questions
What is the primary role of smooth muscles in the body?
Smooth muscles regulate involuntary processes in the body, including blood vessel constriction, gastrointestinal motility, respiratory airway control, and uterine contractions. Their continuous, rhythmic contractions are essential for maintaining homeostasis and ensuring the proper function of vital organ systems.
How do smooth muscles contract and relax?
Smooth muscle contraction is triggered by increased intracellular calcium, which binds to calmodulin and activates myosin light-chain kinase (MLCK). This leads to phosphorylation of myosin and cross-bridge formation with actin. Relaxation occurs when calcium levels decrease, allowing myosin light-chain phosphatase (MLCP) to reverse phosphorylation, ending contraction.
What are common symptoms of smooth muscle disorders?
Symptoms vary by disorder but can include abdominal pain, irregular bowel movements in IBS, shortness of breath and wheezing in asthma, high blood pressure in vascular conditions, and painful menstrual cramps in dysmenorrhea. Early detection and diagnosis are key for effective treatment.
Which lifestyle changes benefit smooth muscle health?
Adopting a balanced diet, staying hydrated, exercising regularly, managing stress, avoiding smoking, and limiting alcohol intake all support smooth muscle function. Additionally, incorporating probiotic and magnesium-rich foods helps maintain overall health.
How are smooth muscle conditions diagnosed and treated?
Diagnosis typically involves a combination of clinical evaluations, imaging studies, functional tests, and laboratory investigations. Treatments range from lifestyle modifications and medications to minimally invasive procedures and surgical interventions, tailored to each specific condition.
Disclaimer & Sharing
The information provided in this article is for educational purposes only and should not be considered as a substitute for professional medical advice. Always consult with a qualified healthcare provider for personalized guidance and treatment options.
Feel free to share this article on Facebook, X (formerly Twitter), or your preferred platform to help spread awareness about smooth muscle health and promote informed wellness practices.