The testes are essential male reproductive organs that serve dual roles in producing sperm (spermatogenesis) and synthesizing testosterone, the primary male sex hormone. Encased in the scrotum, they maintain a temperature slightly below core body temperature, which is crucial for proper sperm production. Beyond reproduction, the testes also influence secondary sexual characteristics, metabolism, and overall male health. This in-depth guide explores testicular anatomy, physiological functions, common disorders, diagnostic techniques, treatment options, and lifestyle strategies to promote optimal testicular health.
Table of Contents
- Structural Features
- Coverings and Lobular Organization
- Seminiferous Tubules & Cellular Components
- Interstitial Tissue & Leydig Cells
- Rete Testis, Efferent Ductules & Epididymis
- Vascular Supply, Lymphatic Drainage & Innervation
- Temperature Regulation & Testicular Descent
- Testicular Physiology and Functions
- Common Testicular Conditions
- Diagnostic Methods
- Treatment Options
- Supplements for Testicular Health
- Lifestyle Practices and Healthy Tips
- Trusted Resources
- Frequently Asked Questions
- Disclaimer & Sharing
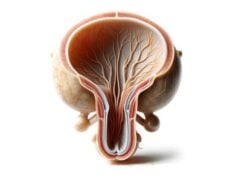
Structural Features of the Testes
The testes are paired organs located within the scrotum and are vital for male reproductive and endocrine functions. Each testis is approximately the size of a small egg and has a smooth, oval shape. Their primary roles are to produce sperm and synthesize testosterone, the hormone responsible for developing male secondary sexual characteristics. Structurally, the testes are encapsulated by several layers that protect their delicate tissues and support their complex functions.
Key structural features include:
- Size & Shape: Typically, each testis weighs about 15–25 grams and is oval or almond-shaped.
- Color & Texture: They appear smooth and slightly lobulated with a homogenous texture due to their high collagen content and organized cellular structure.
- Encapsulation: Multiple layers of tissue surround the testes, each serving distinct protective and supportive roles.
Coverings and Lobular Organization
The testes are protected by several distinct coverings and are internally divided into smaller functional units.
Coverings
- Tunica Vaginalis:
This double-layered serous membrane originates from the peritoneum. The outer (parietal) layer lines the scrotal cavity, while the inner (visceral) layer adheres directly to the testicular surface. The space between these layers contains a small amount of serous fluid that facilitates frictionless movement within the scrotum. - Tunica Albuginea:
Beneath the tunica vaginalis lies the tunica albuginea, a dense, fibrous capsule that encases each testis. It provides structural support and protection and sends septa inward to divide the testis into lobules. - Tunica Vasculosa:
The innermost vascular layer of the tunica albuginea, rich in blood vessels, ensures that the testicular tissue receives essential nutrients and oxygen.
Lobular Organization
The tunica albuginea divides each testis into approximately 250-300 lobules. Within these lobules, coiled seminiferous tubules—where spermatogenesis occurs—are densely packed. This lobular organization optimizes the space within the testis for efficient sperm production and hormone synthesis.
Seminiferous Tubules & Cellular Components
The seminiferous tubules are the site of spermatogenesis, where sperm are produced through a highly organized and regulated process.
Structure
- Length and Coiling:
When uncoiled, the seminiferous tubules can extend up to 70 centimeters, yet they are compactly arranged within each lobule of the testis. - Epithelial Lining:
They are lined by a stratified epithelium composed of two main types of cells: - Sertoli Cells:
These supportive cells nourish developing sperm cells, form the blood-testis barrier, and secrete androgen-binding protein. Their role is crucial in creating a protected microenvironment for spermatogenesis. - Germ Cells:
These cells undergo a series of divisions—first mitosis, then meiosis—to ultimately form mature spermatozoa. The process includes the transformation of spermatogonia into spermatocytes, then spermatids, and finally into fully functional sperm.
Blood-Testis Barrier
Formed by tight junctions between Sertoli cells, the blood-testis barrier protects developing germ cells from harmful substances and immune reactions, ensuring an optimal environment for sperm production.
Interstitial Tissue & Leydig Cells
The interstitial tissue, found between the seminiferous tubules, plays a vital role in hormone production and overall testicular function.
Components
- Leydig Cells:
Scattered throughout the interstitial tissue, Leydig cells are responsible for synthesizing testosterone in response to luteinizing hormone (LH) from the anterior pituitary. Testosterone is essential for spermatogenesis, development of male secondary sexual characteristics, and overall metabolic regulation. - Connective Tissue:
The interstitial tissue also contains blood vessels, lymphatics, and a supportive matrix that ensures proper nutrient and oxygen delivery to testicular cells.
Rete Testis, Efferent Ductules & Epididymis
Once sperm are produced in the seminiferous tubules, they must be transported to the epididymis for maturation and storage.
Rete Testis
- Structure and Function:
The rete testis is a network of tubules located in the mediastinum of the testis. It collects sperm from the seminiferous tubules and channels them into the efferent ductules.
Efferent Ductules
- Role:
These small ducts connect the rete testis to the head of the epididymis, facilitating the transport and concentration of sperm.
Epididymis
- Anatomical Segments:
The epididymis is divided into three parts: - Head: Receives sperm from the efferent ductules and initiates the maturation process.
- Body: Where sperm undergo further maturation and acquire motility.
- Tail: Acts as a storage site until ejaculation.
- Function:
The epididymis provides an environment for sperm to mature, gain motility, and be stored until they are needed for reproduction.
Blood Supply, Lymph Drainage & Innervation
Efficient blood flow, lymphatic drainage, and nerve supply are critical for testicular function and overall reproductive health.
Blood Supply
- Testicular Arteries:
The testes are supplied by the testicular arteries, which originate directly from the abdominal aorta. These arteries branch into smaller arterioles that provide oxygen and nutrients to the testicular tissue. - Pampiniform Plexus:
The venous drainage system, known as the pampiniform plexus, plays a dual role by draining deoxygenated blood and functioning as a counter-current heat exchanger, helping to maintain the optimal temperature for spermatogenesis.
Lymphatic Drainage
- Pathway:
Lymph from the testes drains into the para-aortic lymph nodes located near the kidneys. This drainage pathway is particularly important in the context of testicular cancer, as it is the primary route for metastasis.
Innervation
- Autonomic Innervation:
The testes receive autonomic innervation from both sympathetic and parasympathetic fibers, which regulate blood flow and support endocrine functions. - Sensory Innervation:
The genital branch of the genitofemoral nerve carries sensory information from the testes, contributing to reflexes and pain perception.
Temperature Regulation & Testicular Descent
The testes require an environment that is a few degrees cooler than core body temperature for optimal spermatogenesis. This precise temperature regulation is achieved through several mechanisms.
Scrotal Regulation
- Cremaster Muscle:
This muscle elevates the testes towards the body in cold conditions and relaxes them to cool down when warm. - Dartos Muscle:
The contraction of this smooth muscle in the scrotal skin creates wrinkles, reducing surface area and aiding in heat retention or dissipation. - Pampiniform Plexus:
This network of veins cools arterial blood before it reaches the testes, ensuring the proper temperature is maintained.
Testicular Descent
During fetal development, the testes form near the kidneys and descend into the scrotum via the inguinal canal. This descent is essential for establishing the lower temperature necessary for sperm production. Failure of the testes to descend (cryptorchidism) can lead to infertility and an increased risk of testicular cancer if not corrected.
Testicular Physiology and Functions
The primary functions of the testes are twofold: to produce sperm (spermatogenesis) and to synthesize testosterone, the hormone responsible for male secondary sexual characteristics and various metabolic processes.
Spermatogenesis
Spermatogenesis is a highly regulated process that occurs within the seminiferous tubules. It involves:
- Mitosis:
Spermatogonia (stem cells) divide to form primary spermatocytes. - Meiosis:
Primary spermatocytes undergo two rounds of cell division to produce haploid spermatids. - Spermiogenesis:
Spermatids transform into mature spermatozoa with a streamlined structure optimized for motility.
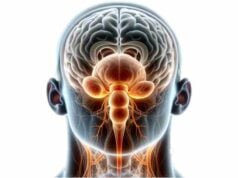
Hormonal Regulation
The hypothalamic-pituitary-gonadal (HPG) axis is key to regulating testicular function.
- Gonadotropin-Releasing Hormone (GnRH):
Secreted by the hypothalamus, GnRH stimulates the anterior pituitary to release LH and FSH. - Luteinizing Hormone (LH):
LH acts on Leydig cells to stimulate testosterone production. - Follicle-Stimulating Hormone (FSH):
FSH supports spermatogenesis by acting on Sertoli cells, which nurture developing sperm and produce androgen-binding protein.
Testosterone Production
Testosterone is vital for:
- Male Secondary Sexual Characteristics:
Development of facial and body hair, deepening of the voice, and increased muscle mass. - Reproductive Function:
Regulation of spermatogenesis and libido. - Systemic Effects:
Impact on mood, bone density, and overall metabolic processes.
Additional Functions
Beyond reproduction, the testes influence overall endocrine balance and contribute to general health by regulating processes such as red blood cell production, fat distribution, and even aspects of cognitive function.
Common Testicular Disorders
The testes are susceptible to a variety of disorders, many of which can affect fertility, hormone production, and overall health. Early detection and treatment are essential for managing these conditions effectively.
Cryptorchidism
- Definition:
Cryptorchidism is the failure of one or both testes to descend into the scrotum. It is one of the most common congenital abnormalities in males. - Complications:
Increased risk of infertility and testicular cancer. - Treatment:
Hormone therapy or surgical correction (orchiopexy) is usually recommended.
Testicular Torsion
- Definition:
Testicular torsion occurs when the spermatic cord twists, cutting off blood supply to the testis. - Symptoms:
Severe pain, swelling, and sudden onset of scrotal pain. - Treatment:
Surgical detorsion is a medical emergency; if blood flow is not restored promptly, orchiectomy may be necessary.
Epididymitis and Orchitis
- Definition:
Inflammation of the epididymis (epididymitis) or the testis (orchitis) often due to bacterial infections or sexually transmitted infections. - Symptoms:
Scrotal pain, swelling, redness, fever, and urinary symptoms. - Treatment:
Antibiotics and supportive care (rest, scrotal elevation) are typically effective.
Testicular Cancer
- Definition:
Testicular cancer is a malignancy arising primarily from germ cells and is most common in men aged 15 to 35. - Symptoms:
Painless lump or swelling in the testis, discomfort, or pain. - Treatment:
Early detection through self-examination is critical; treatment options include orchiectomy, chemotherapy, and radiation therapy, depending on the cancer stage.
Varicocele
- Definition:
Varicocele is the abnormal enlargement of veins in the scrotum, often affecting sperm quality and causing discomfort. - Symptoms:
A feeling of heaviness or aching in the scrotum. - Treatment:
Varicocelectomy (surgical ligation) or embolization can improve symptoms and fertility.
Hydrocele
- Definition:
A hydrocele is a fluid-filled sac surrounding the testis that causes swelling. - Symptoms:
Painless swelling, discomfort, and sometimes a visible bulge in the scrotum. - Treatment:
Hydroceles in infants may resolve spontaneously, whereas persistent cases in adults may require surgical drainage.
Hypogonadism
- Definition:
Hypogonadism occurs when the testes fail to produce sufficient testosterone, affecting fertility and secondary sexual characteristics. - Causes:
Genetic disorders, injury, infections, or chronic illnesses. - Treatment:
Testosterone replacement therapy is the mainstay of treatment.
Orchiectomy and Trauma
- Definition:
Orchiectomy refers to the surgical removal of one or both testes, which may be necessary due to cancer, severe trauma, or as part of gender-affirming surgery. - Considerations:
Post-surgical hormonal replacement and psychological support are critical for recovery and overall health.
Infectious and Inflammatory Conditions
- Examples:
Conditions such as mumps orchitis, tuberculosis, and autoimmune orchitis. - Symptoms:
Testicular pain, swelling, fever, and sometimes systemic symptoms. - Treatment:
Appropriate antibiotics, antiviral agents, or immunosuppressive therapies are used based on the underlying cause.
Testicular Atrophy
- Definition:
Testicular atrophy involves the shrinkage of the testes due to various causes including hormonal imbalances, chronic infections, trauma, and systemic diseases. - Symptoms:
Reduced testicular size, decreased fertility, and low testosterone levels. - Treatment:
Treatment is focused on the underlying cause, which may include hormone therapy or lifestyle changes.
Diagnostic Techniques for Testicular Disorders
Accurate diagnosis is paramount to effectively manage testicular disorders. A comprehensive evaluation typically combines clinical assessments with various imaging, laboratory, and specialized tests.
Clinical Examination
- Physical Examination:
The initial evaluation involves palpating the testes and scrotum to detect abnormalities such as lumps, swelling, or tenderness. The examination may also include assessing the size, consistency, and position of the testes. - Patient History:
A thorough medical history is essential to understand symptoms, previous conditions, family history, and any history of trauma or infections. Self-examination is also encouraged for early detection of abnormalities.
Imaging Studies
- Ultrasound:
Scrotal ultrasound is the first-line imaging modality for evaluating testicular conditions. It is highly effective in detecting masses, cysts, varicoceles, and other structural abnormalities. - Doppler Ultrasound:
This technique assesses blood flow within the testes and is particularly useful for diagnosing testicular torsion and evaluating varicocele severity. - Magnetic Resonance Imaging (MRI):
MRI provides detailed soft tissue imaging and is used when ultrasound findings are inconclusive or when further characterization of testicular masses is needed. - Computed Tomography (CT) Scan:
CT scans can be used to assess the extent of testicular cancer and detect metastatic spread, particularly to retroperitoneal lymph nodes.
Laboratory Tests
- Hormone Panel:
Blood tests measuring testosterone, LH, and FSH help diagnose hypogonadism and other endocrine disorders affecting the testes. - Tumor Markers:
Blood tests for AFP, hCG, and LDH are critical in diagnosing and monitoring testicular cancer. - Infection Screening:
Urine and swab tests for sexually transmitted infections (STIs) are used to diagnose epididymitis and orchitis.
Biopsy and Histopathology
- Testicular Biopsy:
In cases of unexplained infertility or suspected cancer, a biopsy can provide definitive histopathological diagnosis. - Histopathological Examination:
Microscopic analysis of biopsy samples helps detect neoplastic changes, inflammation, or fibrosis.
Genetic Testing
- Karyotyping and Genetic Panels:
Genetic tests, including karyotyping, are used to diagnose congenital disorders such as Klinefelter syndrome, which can affect testicular function.
Functional Tests
- Semen Analysis:
Evaluates sperm count, motility, and morphology to assess reproductive function. - Scrotal Transillumination:
Used to differentiate between solid and cystic masses, particularly in the case of hydroceles.
Treatment Options for Testicular Disorders
Treatment strategies for testicular disorders depend on the specific condition, its severity, and the overall health of the patient. A combination of medical management, surgical interventions, and supportive therapies is often required.
Medical Management
Antibiotic Therapy
- Indications:
Used to treat epididymitis and orchitis, especially when caused by bacterial infections or STIs. - Common Medications:
Doxycycline, ceftriaxone, or fluoroquinolones are often prescribed based on the causative organism.
Hormone Replacement Therapy (HRT)
- Purpose:
For hypogonadism, testosterone replacement therapy (TRT) helps restore normal hormone levels. - Delivery Methods:
Options include injections, transdermal patches, gels, or implants.
Pain and Inflammation Management
- NSAIDs:
Nonsteroidal anti-inflammatory drugs such as ibuprofen are used to manage pain and reduce inflammation in conditions like testicular torsion and epididymitis. - Supportive Measures:
Rest, scrotal elevation, and cold compresses are recommended to alleviate discomfort.
Surgical Interventions
Orchiopexy
- Indication:
Treats cryptorchidism by surgically relocating undescended testes into the scrotum. - Benefits:
Early orchiopexy reduces the risk of infertility and testicular cancer.
Orchiectomy
- Indication:
The removal of one or both testes, primarily performed for testicular cancer or severe trauma. - Postoperative Care:
May involve chemotherapy or radiation therapy in cases of cancer, along with hormone replacement if necessary.
Varicocelectomy
- Purpose:
Surgical correction of varicoceles, which can improve sperm quality and alleviate pain. - Techniques:
Options include open surgery, laparoscopic surgery, or percutaneous embolization.
Hydrocelectomy
- Indication:
For symptomatic hydroceles causing discomfort or complications. - Procedure:
Involves draining the fluid and removing the sac if necessary.
Detorsion Surgery
- Indication:
An emergency procedure for testicular torsion, where timely surgical intervention is crucial to restore blood flow and save the testis.
Advanced and Experimental Treatments
Microdissection Testicular Sperm Extraction (micro-TESE)
- Purpose:
Used in cases of non-obstructive azoospermia, micro-TESE extracts sperm directly from testicular tissue under microscopic guidance. - Application:
This technique enhances the chances of retrieving viable sperm for assisted reproductive technologies.
Testicular Tissue Cryopreservation
- Purpose:
An experimental method to preserve fertility in prepubertal boys undergoing treatments that may compromise testicular function. - Procedure:
Involves freezing a small sample of testicular tissue for future use.
Stem Cell Therapy
- Potential:
Research into stem cell therapy aims to regenerate damaged testicular tissue and improve fertility outcomes in men with testicular failure.
Radiation and Chemotherapy
Testicular Cancer Management
- Surgical Removal:
Orchiectomy is the primary treatment for testicular cancer, followed by adjuvant therapies if needed. - Chemotherapy and Radiation:
Depending on the type and stage of cancer, additional treatments such as chemotherapy (cisplatin-based regimens) and radiation therapy may be used.
Psychological Support
Testicular disorders, especially those affecting fertility or involving cancer, can have significant psychological impacts. Counseling and psychological support are critical components of comprehensive care, helping patients manage stress, anxiety, and depression related to their condition.
Effective Supplements for Testicular Health
A range of supplements can support testicular function, improve sperm quality, and enhance overall reproductive health. These supplements provide essential nutrients, antioxidants, and hormones that are critical for maintaining healthy testicular tissue.
Key Supplements
- Zinc:
Vital for testosterone production and sperm quality. Studies suggest that zinc supplementation can improve sperm count, motility, and morphology, especially in zinc-deficient individuals. - Vitamin D:
Plays a crucial role in hormone synthesis and immune function. Adequate levels of vitamin D are associated with higher testosterone levels. - Omega-3 Fatty Acids:
Found in fish oil, these fatty acids help reduce inflammation and improve sperm membrane integrity. - Coenzyme Q10 (CoQ10):
An antioxidant that supports cellular energy production and improves sperm motility and concentration. - L-Carnitine:
Enhances energy metabolism in sperm cells, which can lead to improved sperm motility. - Selenium:
This antioxidant mineral protects sperm from oxidative damage and improves motility. - Folic Acid:
Essential for DNA synthesis and repair, folic acid works synergistically with zinc to improve sperm quality. - Ashwagandha:
An adaptogenic herb that reduces stress and improves testosterone levels and sperm quality. - Maca Root:
Traditionally used to boost fertility, maca root can enhance sperm concentration, motility, and sexual function. - Vitamin E:
An antioxidant that protects sperm membranes from oxidative stress and improves overall sperm function.
Lifestyle and Maintenance Tips for Testicular Health
Adopting a healthy lifestyle is crucial for maintaining optimal testicular function and overall reproductive health. Here are some practical recommendations:
Regular Self-Examination
- Monthly Checks:
Perform self-examinations to detect any lumps, swelling, or changes in the size and shape of the testes. Early detection of abnormalities is vital for prompt treatment.
Diet and Nutrition
- Balanced Diet:
Consume a nutrient-rich diet high in fruits, vegetables, lean proteins, and whole grains to support hormone production and overall reproductive health. - Hydration:
Drink plenty of water daily to ensure proper bodily functions, including efficient nutrient delivery and toxin removal. - Antioxidant-Rich Foods:
Incorporate foods high in antioxidants, such as berries, leafy greens, and nuts, to reduce oxidative stress on testicular tissue.
Exercise and Physical Activity
- Regular Exercise:
Engage in moderate physical activity to boost circulation, support hormone balance, and maintain a healthy weight. - Avoid Overheating:
Avoid prolonged exposure to high temperatures (hot tubs, saunas) as excessive heat can impair sperm production.
Stress Management
- Mindfulness Practices:
Incorporate stress-reduction techniques such as meditation, yoga, or deep breathing exercises to maintain hormonal balance. - Adequate Sleep:
Aim for 7–9 hours of quality sleep each night to allow the body to recover and regulate hormone levels.
Avoid Harmful Substances
- Limit Alcohol:
Excessive alcohol consumption can negatively impact testosterone levels and sperm quality. - Quit Smoking:
Smoking is linked to lower sperm quality and increased risk of testicular cancer. - Minimize Exposure to Toxins:
Reduce exposure to environmental toxins and endocrine disruptors by choosing organic foods and using natural personal care products when possible.
Regular Medical Check-Ups
- Health Screenings:
Regular visits to a healthcare provider can help detect and manage testicular disorders early. - Vaccinations and STI Testing:
Stay up-to-date with vaccinations and regularly test for sexually transmitted infections, which can affect testicular health.
Trusted Resources for Testicular Health
For further information on testicular health, consider these trusted resources that provide evidence-based research and comprehensive guidance.
Books
- “The Testicular Cancer Resource Guide” by Scott Williams
A thorough resource covering testicular cancer, including diagnostic strategies, treatment options, and patient support. - “Male Infertility: Contemporary Clinical Approaches, Andrology, ART & Antioxidants” by Sijo J. Parekattil and Ashok Agarwal
Offers insights into male infertility, including testicular function, modern treatments, and lifestyle interventions. - “Endocrinology of the Testis and Male Reproduction” edited by Manuela Simoni and Ilpo T. Huhtaniemi
Provides an in-depth exploration of hormonal regulation and reproductive functions of the testes.
Academic Journals
- The Journal of Urology
Publishes high-quality research on testicular health, male reproductive disorders, and innovative treatment approaches. - Human Reproduction
Focuses on studies related to testicular function, fertility, and assisted reproductive technologies.
Mobile Apps
- MyCancerCoach
Provides personalized information and resources for testicular cancer patients, including treatment options and side-effect management. - Testicular Cancer Society
Offers educational materials, self-examination guides, and support for men affected by testicular cancer. - Male Fertility
A comprehensive app that helps track diet, exercise, and lifestyle factors that affect fertility and overall testicular health.
Frequently Asked Questions
What are the primary functions of the testes?
The testes produce sperm (spermatogenesis) and synthesize testosterone, the main male sex hormone. These functions are critical for male fertility, the development of secondary sexual characteristics, and overall hormonal balance.
How is spermatogenesis regulated?
Spermatogenesis is regulated by the hypothalamic-pituitary-gonadal axis. GnRH from the hypothalamus stimulates the release of LH and FSH from the pituitary, which in turn stimulate Leydig and Sertoli cells to produce testosterone and support sperm maturation.
What causes testicular disorders like cryptorchidism?
Cryptorchidism, or undescended testes, is a congenital condition where one or both testes fail to descend into the scrotum. It can lead to infertility and an increased risk of testicular cancer if not corrected early.
How is testicular cancer diagnosed?
Testicular cancer is typically diagnosed through self-examination, followed by clinical evaluation, ultrasound imaging, and blood tests for tumor markers such as AFP, hCG, and LDH.
What lifestyle changes can improve testicular health?
Maintaining a balanced diet, regular exercise, avoiding excessive heat exposure, managing stress, quitting smoking, and having regular medical check-ups are key strategies to support testicular health and overall reproductive function.
Disclaimer & Sharing
The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a qualified healthcare provider for diagnosis and treatment tailored to your needs.
If you found this guide helpful, please share it on Facebook, X (formerly Twitter), or your preferred social platform to help spread awareness and promote testicular health.