The urethra is a narrow tube essential for both urinary excretion and, in males, reproductive functions. It not only facilitates the elimination of urine from the body but also plays a crucial role in protecting against infections and ensuring proper continence. In this guide, we delve into the intricate anatomy of the urethra, explore its dynamic functions, discuss common disorders that affect it, and review modern diagnostic techniques and treatment options. Additionally, we cover nutritional supplements and lifestyle practices designed to maintain optimal urethral health. Whether you are a healthcare professional or simply interested in understanding this vital structure, this comprehensive resource offers detailed insights and practical tips.
Table of Contents
- Urethral Structural Overview
- Urethral Functional Dynamics
- Urethral Disorders and Pathologies
- Diagnostic Techniques for Urethral Conditions
- Therapeutic Interventions and Management Strategies
- Nutritional Supplements for Urethral Wellness
- Lifestyle and Preventive Measures for Urethral Health
- Recommended References and Resources
- Frequently Asked Questions
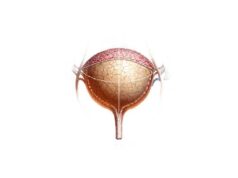
Urethral Structural Overview
The urethra’s structure is uniquely adapted to its dual functions in both the urinary and reproductive systems. Notably, its anatomical features differ between males and females, reflecting distinct roles and clinical considerations.
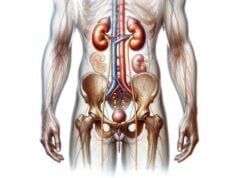
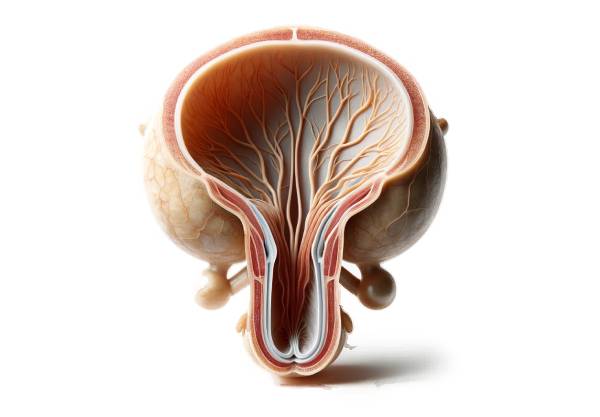
Male Urethral Anatomy
In males, the urethra measures roughly 20 centimeters and is divided into three main segments:
- Prostatic Urethra:
Approximately 3–4 centimeters long, this segment runs through the prostate gland. It serves as the passageway for both urine and seminal fluid. The urethral crest, a raised ridge along the posterior wall, and the prostatic sinuses, which collect secretions from the prostate, are characteristic features of this portion. - Membranous Urethra:
This short segment (about 1–2 centimeters) passes through the urogenital diaphragm. It is the narrowest and least distensible portion and is encircled by the external urethral sphincter—a voluntary muscle critical for continence. - Spongy (Penile) Urethra:
Extending about 15 centimeters along the length of the penis, this is the longest part of the male urethra. It is surrounded by the corpus spongiosum, an erectile tissue that cushions and protects the urethra during an erection. Along its length, glandular openings (including ducts from the bulbourethral glands) secrete mucus to aid lubrication.
Female Urethral Anatomy
In contrast, the female urethra is much shorter, measuring approximately 4 centimeters, and is dedicated solely to the urinary function:
- Proximal Urethra:
Originating at the bladder’s internal urethral orifice, this segment courses through the pelvic floor muscles and is guarded by an involuntary internal urethral sphincter composed of smooth muscle. - Distal Urethra:
Passing through the urogenital diaphragm, the distal urethra ends at the external urethral orifice, which is positioned anterior to the vaginal opening. The voluntary external urethral sphincter surrounds this segment, allowing for conscious control over urination.
Histological Composition
The urethral wall is characterized by a gradual transition in its epithelial lining:
- Epithelial Layer:
The lining begins as transitional epithelium near the bladder, shifts to stratified or pseudostratified columnar epithelium along most of its length, and finally becomes stratified squamous epithelium near the external orifice. This gradation protects the tissue from the irritative effects of urine and mechanical stress. - Lamina Propria:
Located beneath the epithelium, this connective tissue layer contains blood vessels, nerve fibers, and elastic fibers that provide structural support and flexibility. - Muscularis Layer:
Comprising an inner longitudinal and an outer circular layer of smooth muscle, the muscularis is essential for generating the peristaltic movements that propel urine. In males, the external sphincter adds a layer of skeletal muscle control.
Vascular and Neural Supply
The urethra receives a rich blood supply that varies according to its segments and gender:
- In Males:
- The prostatic urethra is supplied by branches of the inferior vesical artery.
- The membranous urethra derives blood from the bulbourethral artery.
- The spongy urethra is vascularized by the internal pudendal artery.
Venous drainage mirrors this pattern, connecting to the prostatic venous plexus and internal pudendal veins. - In Females:
The urethra is primarily supplied by branches of the internal pudendal and vaginal arteries, with venous return occurring via the corresponding venous networks.
Innervation includes both autonomic and somatic components. The autonomic nervous system—sympathetic fibers from the hypogastric plexus and parasympathetic fibers from the pelvic splanchnic nerves—regulates smooth muscle tone. Somatic innervation via the pudendal nerve controls the external urethral sphincter, facilitating voluntary urination.
Lymphatic Drainage and Variations
Lymphatic drainage follows the vascular patterns. In males, lymph from the prostatic and membranous urethra drains into the internal iliac nodes, while the spongy urethra drains into the superficial inguinal nodes. In females, drainage is directed to both the internal iliac and superficial inguinal lymph nodes.
Anatomical variations, such as congenital anomalies (e.g., hypospadias, where the urethral opening is abnormally positioned) and differences in urethral length or curvature, can significantly impact function and treatment approaches.
Urethral Functional Dynamics
The urethra’s functionality is central to both urinary excretion and, in males, reproductive performance. Its physiological mechanisms are designed to ensure efficient urine passage while maintaining protection and continence.
Urinary Excretion Process
The primary role of the urethra is the safe and effective transport of urine from the bladder to the exterior:
- Storage Phase:
During the storage phase, the internal urethral sphincter (involuntary) contracts, keeping urine securely in the bladder. Simultaneously, the external sphincter (voluntary) provides additional control, allowing the bladder to fill without leakage. - Voiding Phase:
Upon initiation of urination, the detrusor muscle contracts forcefully, while the internal sphincter relaxes. Voluntary relaxation of the external sphincter then permits urine to flow. Coordinated peristaltic waves in the muscularis help propel urine along the urethra with minimal resistance.
Male Reproductive Role
In males, the urethra serves a dual purpose by acting as a conduit for both urine and semen:
- Ejaculatory Mechanism:
During ejaculation, the internal sphincter contracts to prevent retrograde flow of semen into the bladder. The prostatic urethra receives secretions from the seminal vesicles and prostate, which combine with sperm to form semen. Subsequent contractions of the bulbospongiosus muscle propel the semen through the spongy urethra and out of the penile tip.
Protective and Continence Mechanisms
The urethra also incorporates several features to protect against infection and maintain continence:
- Mucosal Secretion:
Glands along the urethra, including the periurethral and bulbourethral glands in males, secrete mucus that lubricates the urethral lining. This lubrication reduces friction during urination and ejaculation, thereby minimizing tissue damage. - Antimicrobial Environment:
The mucus, along with the slightly acidic pH of urine, creates an environment that discourages bacterial adhesion and growth, thus lowering the risk of infections such as urethritis. - Sphincter Control:
The interplay between the involuntary internal sphincter and the voluntary external sphincter is vital for maintaining continence. This dual mechanism ensures that urine is retained during bladder filling and only released when appropriate.
Coordination with the Bladder
Effective urinary function relies on the seamless coordination between the bladder and the urethra. Neural signals trigger bladder contraction and sphincter relaxation in a precisely timed sequence, ensuring that urine is expelled efficiently while maintaining the integrity of the urinary system.
Urethral Disorders and Pathologies
Despite its small size, the urethra is prone to a variety of conditions that can significantly impact quality of life. Understanding these disorders is essential for timely diagnosis and effective treatment.
Urethritis
Urethritis refers to inflammation of the urethra, which can be caused by bacterial or viral infections.
- Etiology:
The most common causes include sexually transmitted infections such as Neisseria gonorrhoeae (gonococcal urethritis) and Chlamydia trachomatis (non-gonococcal urethritis). Other pathogens, including Mycoplasma genitalium, may also be involved. - Symptoms:
Typical symptoms include painful urination (dysuria), increased frequency and urgency, and a purulent or clear urethral discharge. In men, pain during ejaculation is common; in women, pelvic discomfort may be present. - Management:
Diagnosis is confirmed via urine tests, swab cultures, and PCR assays. Treatment generally involves a course of appropriate antibiotics or antivirals, with sexual abstinence advised until resolution.
Urethral Stricture
A urethral stricture is a narrowing of the urethral lumen resulting from scar tissue formation, often secondary to trauma, infection, or prior surgery.
- Clinical Presentation:
Patients may experience reduced urinary stream, difficulty initiating urination, and recurrent urinary tract infections. Severe strictures can lead to urinary retention and bladder dysfunction. - Diagnostic Methods:
Imaging studies such as retrograde urethrography and urethroscopy are used to assess the extent and location of the narrowing. - Treatment Options:
Management may include urethral dilation, internal urethrotomy (surgical incision of the stricture), and, in refractory cases, urethroplasty—surgical reconstruction of the affected segment.
Urinary Incontinence
Urinary incontinence is the involuntary leakage of urine, a condition that can result from a variety of underlying pathologies affecting the urethra and surrounding musculature.
- Types:
Common forms include stress incontinence (leakage during physical activity), urge incontinence (sudden, intense urge to urinate), overflow incontinence, and functional incontinence. - Diagnosis and Management:
A thorough evaluation, including urodynamic testing and bladder diaries, guides treatment. Options range from pelvic floor muscle training (Kegels) and behavioral therapies to pharmacologic treatments and surgical interventions such as sling procedures or the implantation of an artificial urinary sphincter.
Urethral Cancer
Although rare, urethral cancer is a serious condition involving the development of malignant tumors within the urethra.
- Risk Factors and Presentation:
Risk factors include chronic inflammation, HPV infection, and a history of recurrent infections. Symptoms typically include painless hematuria, difficulty urinating, and sometimes a palpable mass. - Diagnostic Approach:
Diagnosis is established through cystoscopy, biopsy, and advanced imaging (CT, MRI). Staging of the tumor guides subsequent management. - Treatment:
Treatment modalities vary based on the stage and location of the tumor and may include surgical resection, radiation therapy, and chemotherapy.
Urethral Diverticulum
A urethral diverticulum is a pouch-like protrusion of the urethral wall that can trap urine and predispose to infections.
- Symptoms:
Patients may experience recurrent urinary tract infections, pelvic pain, painful urination, and, in women, a palpable mass in the anterior vaginal wall. - Diagnosis and Treatment:
Diagnosis is typically made using MRI, ultrasound, or cystourethroscopy. Surgical excision of the diverticulum is the definitive treatment, with reconstruction of the urethral wall as needed.
Congenital Anomalies: Hypospadias and Epispadias
Hypospadias and epispadias are congenital malformations affecting the male urethra.
- Hypospadias:
The urethral opening is located on the underside of the penis. This condition can affect urinary stream direction and, in severe cases, sexual function. Surgical correction is typically recommended in early childhood. - Epispadias:
A less common condition where the urethral opening is on the upper surface of the penis. It may be associated with bladder exstrophy and also requires surgical intervention for functional and cosmetic restoration.
Urethral Prolapse
Urethral prolapse occurs when the mucosal lining of the urethra protrudes through the external orifice. This condition is most commonly seen in prepubescent girls and postmenopausal women.
- Clinical Features:
Visible protrusion at the urethral opening, pain, bleeding, and difficulties with urination are common signs. - Management:
Treatment may begin with topical estrogen therapy to reduce inflammation, with surgical correction reserved for refractory cases.
Diagnostic Techniques for Urethral Conditions
A precise diagnosis is essential for the successful treatment of urethral disorders. Various diagnostic methods, ranging from simple clinical assessments to advanced imaging, aid in identifying the nature and extent of the pathology.
Clinical Examination and History
- Detailed Patient History:
Gathering comprehensive information about symptoms—such as dysuria, urinary frequency, urgency, and any discharge—is the first step in the diagnostic process. - Physical Examination:
A thorough genital and pelvic examination, including palpation of the penis and prostate in males and a pelvic exam in females, can reveal visible abnormalities and areas of tenderness.
Laboratory Tests
- Urinalysis:
A basic yet essential test that examines the urine for signs of infection, blood, or crystalluria. It serves as an initial screening tool for conditions like urethritis and urinary tract infections. - Urine Culture:
This test identifies bacterial pathogens and determines antibiotic sensitivity, guiding appropriate treatment. - Polymerase Chain Reaction (PCR):
Highly sensitive molecular techniques detect specific pathogens responsible for urethritis, such as Chlamydia trachomatis and Neisseria gonorrhoeae. - Blood Tests:
Complete blood count (CBC) and markers such as C-reactive protein (CRP) may indicate systemic infection or inflammation.
Imaging Studies
- Ultrasound:
This non-invasive modality is effective in detecting structural abnormalities such as diverticula and assessing the bladder and kidneys without radiation exposure. - X-rays and Retrograde Urethrography:
In retrograde urethrography, contrast dye is injected into the urethra followed by X-rays, which help visualize strictures, diverticula, and other structural abnormalities. - Computed Tomography (CT) Scans:
CT scans, especially non-contrast studies, offer detailed cross-sectional images that help diagnose complex conditions like stones and tumors. - Magnetic Resonance Imaging (MRI):
MRI provides high-resolution, radiation-free images that are particularly useful for evaluating soft tissue structures and congenital anomalies.
Endoscopic Techniques
- Cystoscopy:
This procedure involves inserting a flexible scope through the urethra into the bladder, allowing direct visualization of the urethral and bladder mucosa. It is invaluable for diagnosing strictures, tumors, and other abnormalities, and permits tissue biopsy. - Urethroscopy:
Similar to cystoscopy, urethroscopy focuses on the urethra, facilitating the diagnosis and treatment of conditions such as strictures and foreign bodies.
Urodynamic Testing
- Uroflowmetry:
This test measures the rate and volume of urine flow, identifying potential obstructions or dysfunctions in the urethral passage. - Pressure-Flow Studies:
These studies assess the pressure within the bladder and urethra during voiding, offering insights into sphincter function and potential obstructions.
Histopathological Examination
- Biopsy:
In cases of suspected malignancy or chronic inflammation, a small tissue sample is obtained via endoscopy for microscopic examination. - Histopathology:
Detailed analysis of the tissue sample confirms the diagnosis and helps determine the appropriate treatment plan.
Advanced Imaging Modalities
- Fluoroscopy:
Real-time X-ray imaging, particularly useful during contrast studies such as retrograde urethrography. - Positron Emission Tomography (PET) Scans:
PET scans assess metabolic activity within tissues and can aid in detecting malignant urethral lesions and metastases.
Therapeutic Interventions and Management Strategies
Treatment for urethral disorders is tailored to the specific condition, its severity, and the patient’s overall health. A multidisciplinary approach often combines medical management, minimally invasive procedures, and surgical interventions.
Medical Management
- Antibiotics:
For bacterial infections like urethritis, antibiotics such as doxycycline, azithromycin, or ciprofloxacin are prescribed based on culture sensitivity. - Antiviral Medications:
In cases of viral urethral infections (e.g., herpes simplex virus), antivirals like acyclovir, famciclovir, or valacyclovir are used. - Alpha-blockers:
Medications such as tamsulosin can relax smooth muscle around the urethra, improving urine flow in conditions associated with obstruction, particularly in men with benign prostatic hyperplasia. - Topical Estrogens:
In postmenopausal women with urethral atrophy or prolapse, topical estrogen creams help restore tissue health and alleviate symptoms.
Endoscopic Procedures
- Urethral Dilation:
Gradual stretching of the urethra using dilators is a common approach to manage strictures. This procedure may need to be repeated periodically. - Internal Urethrotomy:
Also known as urethrotomy, this minimally invasive procedure involves using a urethroscope to make small incisions in the stricture to widen the urethral lumen. - Laser Therapy:
Laser techniques are used both to fragment urethral stones and to ablate small tumors or fibrotic tissue, offering a precise and minimally invasive treatment option.
Surgical Interventions
- Urethral Reconstruction (Urethroplasty):
For severe or recurrent strictures, urethroplasty involves excising the narrowed segment and reconstructing the urethra, either by primary anastomosis or by using tissue grafts. - Sling Procedures:
Particularly in women with stress urinary incontinence, sling procedures involve placing a supportive mesh or biological material around the urethra to improve closure and prevent leakage. - Artificial Urinary Sphincter:
In cases of severe incontinence, especially in men, the implantation of an artificial urinary sphincter provides a mechanical means to control urine flow. - Diverticulectomy:
Surgical removal of a urethral diverticulum is indicated when it causes recurrent infections or significant discomfort.
Advanced and Innovative Treatments
- Stem Cell Therapy:
Emerging research suggests that stem cell therapy may aid in regenerating damaged urethral tissues, particularly in cases of chronic strictures. - Tissue Engineering:
Experimental approaches using bioengineered scaffolds seeded with the patient’s own cells offer potential long-term solutions for complex urethral reconstruction. - Robotic-Assisted Surgery:
Robotic platforms enable precise surgical maneuvers for complex urethral repairs, reducing recovery time and minimizing postoperative pain.
Conservative Management
- Pelvic Floor Rehabilitation:
Pelvic floor muscle exercises (Kegels) strengthen the muscles surrounding the urethra, which is particularly beneficial for managing urinary incontinence. - Behavioral Therapies:
Bladder training, timed voiding, and lifestyle modifications can help improve urinary control and reduce symptoms associated with overactive bladder. - Lifestyle Adjustments:
Simple measures, such as reducing irritant intake (caffeine, alcohol) and ensuring regular voiding schedules, can prevent exacerbation of urethral symptoms.
Nutritional Supplements for Urethral Wellness
In addition to conventional therapies, certain nutritional supplements have been shown to support urethral and overall urinary health by preventing infections, reducing inflammation, and optimizing tissue function.
Key Supplement Options
- Cranberry Extract:
Rich in proanthocyanidins, cranberry extract helps prevent bacterial adhesion, particularly of E. coli, thereby reducing the incidence of urinary tract infections. - D-Mannose:
This naturally occurring sugar binds to bacterial adhesion sites in the urinary tract, preventing the colonization of pathogens and reducing recurrent infections. - Probiotics:
Strains such as Lactobacillus and Bifidobacterium help maintain a balanced microbiome in the gut and urinary tract, lowering the risk of infections. - Vitamin C:
As an antioxidant, vitamin C acidifies urine and boosts the immune response, creating an environment less favorable for bacterial growth. - Magnesium:
Magnesium supports muscle and nerve function, including the proper operation of urethral sphincters, and may reduce spasms that contribute to urinary discomfort. - Horsetail Extract:
With natural diuretic properties, horsetail extract helps increase urine flow, which aids in flushing out potential pathogens and debris. - Saw Palmetto:
Commonly used for prostate health, saw palmetto can also help reduce inflammation in the urethra and improve urinary flow in men. - Pumpkin Seed Extract:
Known for its benefits in managing benign prostatic hyperplasia, this extract may improve urinary function and alleviate symptoms related to urethral obstruction. - N-acetylcysteine (NAC):
A potent antioxidant, NAC reduces oxidative stress and inflammation, supporting the overall health of the urethral lining.
Integrating Supplements into Daily Routine
It is important to adopt an individualized approach when incorporating supplements. Consultation with a healthcare provider ensures that any supplement regimen complements dietary habits and addresses specific health needs. When combined with a balanced diet rich in fruits, vegetables, lean proteins, and whole grains, these supplements can provide a robust defense against common urethral issues.
Lifestyle and Preventive Measures for Urethral Health
A holistic approach to maintaining urethral health involves lifestyle modifications and preventive practices that reduce the risk of disorders and promote overall urinary tract wellness.
Daily Health Practices
- Stay Hydrated:
Drinking plenty of water throughout the day ensures continuous urine flow, which flushes out toxins and bacteria. - Maintain Proper Hygiene:
Good genital hygiene, including gentle cleansing without harsh chemicals, minimizes the risk of infections. - Regular Voiding Habits:
Avoiding prolonged urine retention by emptying the bladder frequently can prevent urinary tract infections and reduce pressure on the urethra. - Wear Breathable Clothing:
Loose-fitting, natural-fiber clothing helps maintain a cool and dry environment, reducing irritation. - Avoid Irritants:
Limit exposure to harsh soaps, douches, and scented products that may disrupt the natural flora and irritate the urethral lining.
Health and Wellness Strategies
- Pelvic Floor Exercises:
Regular Kegel exercises strengthen the muscles supporting the urethra and bladder, enhancing continence. - Dietary Modifications:
A diet low in sodium, caffeine, and alcohol, combined with a high intake of fiber and antioxidants, supports overall urinary health. - Manage Chronic Conditions:
Effective management of conditions like diabetes and hypertension reduces the risk of urinary tract complications. - Stress Management:
Techniques such as mindfulness, regular physical activity, and sufficient sleep help manage stress, which can indirectly affect urinary function. - Regular Medical Check-Ups:
Routine consultations with healthcare professionals ensure early detection and management of potential urethral issues.
Recommended References and Resources for Urethral Health
Staying informed with reliable, up-to-date information is essential for both healthcare providers and patients. The following resources offer comprehensive insights into urethral anatomy, disorders, diagnostic methods, and treatment options.
Books
- “Smith’s General Urology” by Emil A. Tanagho and Jack W. McAninch:
A foundational text covering all aspects of urology, with detailed chapters on urethral conditions and their management. - “Campbell-Walsh-Wein Urology” by Alan J. Wein, Louis R. Kavoussi, and Andrew C. Novick:
Recognized as a definitive guide in urology, this comprehensive textbook addresses the anatomy, physiology, and pathology of the urinary system. - “The Urology Textbook” by Hohenfellner, Michael, and Simon Horenblas:
Offering a thorough overview of urological diseases, this book provides detailed information on diagnostic techniques and treatment modalities for urethral disorders.
Academic Journals
- The Journal of Urology:
Published by the American Urological Association, this journal features original research, reviews, and clinical studies covering a wide range of urological topics, including urethral health. - Urology:
A peer-reviewed journal that presents cutting-edge research on diagnostic and therapeutic advances in the field of urology, including studies on urethral conditions.
Mobile Apps and Online Tools
- Urology Times:
An app that provides the latest news, research updates, and clinical guidelines in urology, ideal for healthcare professionals seeking current information. - My Urology App:
A patient-centered resource offering educational materials, symptom tracking, and practical tips for managing urinary health. - Medscape and UpToDate:
Both platforms offer comprehensive, evidence-based information on urological conditions, including detailed sections on urethral disorders.
Frequently Asked Questions
What are the primary functions of the urethra?
The urethra primarily transports urine from the bladder to the outside of the body. In males, it also serves as the conduit for semen during ejaculation. It plays a crucial role in maintaining continence through the coordinated action of internal and external sphincters.
How is urethritis typically diagnosed?
Urethritis is diagnosed using a combination of patient history, physical examination, urine analysis, cultures, and PCR tests to identify the responsible pathogen. Cystoscopy may be used for further evaluation if necessary.
What treatment options exist for urethral strictures?
Urethral strictures are managed with techniques such as urethral dilation, internal urethrotomy, and surgical reconstruction (urethroplasty) for severe cases. The chosen treatment depends on the stricture’s length, location, and severity.
How can lifestyle changes prevent urethral disorders?
Maintaining adequate hydration, practicing good hygiene, voiding regularly, and adopting a balanced diet can help prevent infections and reduce the risk of conditions such as urethritis and incontinence. Regular exercise and stress management also support urinary tract health.
What supplements support urethral and urinary health?
Supplements such as cranberry extract, D-mannose, probiotics, vitamin C, and magnesium help prevent infections and support proper muscle function in the urethra. These supplements improve the urinary tract’s environment, reducing the risk of bacterial adhesion and inflammation.
Disclaimer
The information provided in this article is intended for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a qualified healthcare provider for personalized guidance and treatment.
Please share this article on Facebook, X (formerly Twitter), or your preferred social platform to help spread awareness about urethral health and promote better urinary care.