The uterus is a dynamic, pear-shaped organ that plays a central role in the female reproductive system. It is essential for menstruation, pregnancy, and childbirth, while also influencing hormonal balance and overall health. Throughout a woman’s life, the uterus adapts dramatically—from cyclic changes during the menstrual cycle to significant transformations during gestation. This guide explores every aspect of uterine health, offering detailed insights into its complex anatomy, diverse functions, common disorders, state‐of‐the‐art diagnostic methods, and both traditional and innovative treatment options. Additionally, practical lifestyle tips and nutritional strategies are provided to support long-term uterine well-being.
Table of Contents
- Structural Overview
- Functional Roles and Regulation
- Common Uterine Disorders
- Diagnostic Approaches
- Treatment and Intervention Options
- Supplemental and Nutritional Support
- Lifestyle & Preventive Strategies
- Trusted Resources
- Frequently Asked Questions
Structural Overview
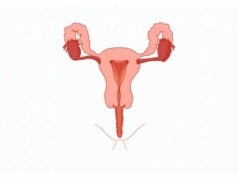
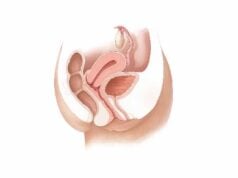
The uterus is a remarkable organ characterized by its layered structure and distinct regions, each of which plays a critical role in reproductive health. Anatomically, it is situated deep within the pelvic cavity, nestled between the bladder and rectum. The organ’s shape—resembling an inverted pear—allows for significant expansion during pregnancy and cyclical changes during menstruation.
Gross Anatomy and Regional Division
The uterus is typically divided into several key regions:
- Fundus: The rounded upper portion that sits above the openings of the fallopian tubes. This dome-shaped area is crucial during pregnancy as it accommodates the growing fetus.
- Corpus (Body): The largest central segment where the fertilized egg implants and where the endometrium proliferates. This region undergoes cyclical thickening and shedding during the menstrual cycle.
- Isthmus: A narrow passage connecting the corpus to the cervix. The isthmus forms the lower uterine segment, particularly evident during the later stages of pregnancy.
- Cervix: The lower cylindrical segment that projects into the vagina, acting as a gateway between the uterus and the vaginal canal. The cervix is vital for sperm transport, maintaining pregnancy, and dilating during labor.
Histological Layers
The uterine wall is composed of three distinct layers, each serving specialized functions:
- Endometrium: This innermost lining is highly dynamic, responding to hormonal fluctuations throughout the menstrual cycle. It is divided into:
- Stratum Functionalis: The superficial layer that thickens in preparation for potential embryo implantation and is shed during menstruation.
- Stratum Basalis: A deeper, permanent layer that regenerates the functionalis after each cycle.
- Myometrium: The thick, muscular middle layer made of smooth muscle fibers arranged in various directions. The myometrium is responsible for generating the powerful contractions necessary during menstruation and labor.
- Perimetrium: The outer serosal layer derived from the peritoneum, which covers and protects the uterus while allowing it to move smoothly against adjacent organs.
Vascular, Neural, and Lymphatic Supply
- Blood Supply:
The uterus is richly supplied with blood by the uterine arteries (branches of the internal iliac arteries) and the ovarian arteries, particularly nourishing the fundus and the lateral walls. Venous drainage is handled through the uterine venous plexus that empties into the internal iliac veins. - Nerve Supply:
Autonomic nerves (sympathetic from T12-L2 and parasympathetic from S2-S4) innervate the uterus, regulating muscle contractions and blood flow. Sensory nerves also transmit pain and stretch sensations, crucial during menstruation and labor. - Lymphatic Drainage:
Lymphatic vessels transport fluid from the uterus to the pelvic and para-aortic lymph nodes, playing an essential role in immune surveillance and the management of uterine malignancies.
Supporting Structures and Variations
- Ligaments:
The uterus is stabilized by several ligaments, including the broad ligament, round ligament, uterosacral ligament, and cardinal ligament. These structures secure the uterus within the pelvis while allowing a degree of movement. - Anatomical Variations:
Congenital anomalies such as bicornuate, septate, unicornuate, and didelphys uterus are variations that can affect reproductive outcomes. Recognizing these variations is important in clinical practice for managing infertility and obstetric complications.
Understanding the uterine structure lays the foundation for comprehending its myriad functions and the ways in which pathological conditions can alter its normal physiology.
Functional Roles and Regulation
The uterus is central to the reproductive system, undertaking roles that span from menstruation to childbirth. Its function is governed by a complex interplay of hormonal, neural, and mechanical factors that work in harmony to ensure reproductive success and overall female health.
Menstrual Cycle Dynamics
The menstrual cycle represents the cyclical process of endometrial regeneration, differentiation, and shedding:
- Proliferative Phase:
In response to rising estrogen levels after menstruation, the endometrium thickens, preparing a nutrient-rich environment for potential embryo implantation. - Secretory Phase:
Following ovulation, progesterone from the corpus luteum further matures the endometrium, increasing vascularity and glandular secretions to support an implanting embryo. - Menstrual Phase:
In the absence of fertilization, a drop in progesterone triggers the shedding of the stratum functionalis, resulting in menstrual bleeding.
Pregnancy and Fetal Support
The uterus is indispensable during pregnancy:
- Implantation and Decidualization:
After fertilization, the blastocyst implants in the endometrium, which then transforms into the decidua. This process establishes a nourishing interface between mother and embryo. - Uterine Expansion:
Throughout pregnancy, the myometrium undergoes hypertrophy and hyperplasia, allowing the uterus to expand significantly—from roughly 50 grams in its non-pregnant state to nearly 1,000 grams at term. - Placental Development:
The placenta forms within the uterine wall, facilitating the exchange of nutrients, gases, and waste products between the mother and the developing fetus. - Labor and Delivery:
Coordinated uterine contractions, regulated by oxytocin and other hormones, result in cervical dilation and the expulsion of the fetus during childbirth.
Hormonal and Neural Regulation
Hormones play a vital role in regulating uterine function:
- Estrogen and Progesterone:
These primary reproductive hormones control the cyclical changes of the endometrium, modulate myometrial contractility, and influence uterine blood flow. - Oxytocin and Prostaglandins:
During labor, these agents induce powerful uterine contractions. Oxytocin, in particular, is critical for initiating labor and facilitating postpartum uterine involution. - Neural Inputs:
Sensory and autonomic nerve fibers convey signals regarding uterine stretch and pain, aiding in the coordination of the menses and labor processes.
Protective Mechanisms
The uterus also serves protective functions:
- Immunological Barrier:
The endometrium contains immune cells that protect against infections. Additionally, the cyclical shedding of the endometrium helps clear potential pathogens. - Mechanical Support:
Structural ligaments and pelvic floor muscles provide essential support, maintaining proper uterine position and function during daily activities and pregnancy.
Together, these functional roles underscore the uterus’s critical importance in reproductive health and its responsiveness to internal and external signals.
Common Uterine Disorders
Various conditions can affect the uterus, impacting menstrual regularity, fertility, and overall well-being. Understanding these disorders is essential for prompt diagnosis and effective management.
Uterine Fibroids
Uterine fibroids, or leiomyomas, are benign tumors arising from the myometrium:
- Prevalence and Risk Factors:
Common among women of reproductive age, fibroids are influenced by hormonal levels, genetics, and growth factors. - Symptoms:
Fibroids may be asymptomatic, but symptomatic cases often involve heavy menstrual bleeding, pelvic pain, pressure, and reproductive challenges. - Management:
Treatment options include medication, minimally invasive procedures like uterine artery embolization, and surgical interventions such as myomectomy or hysterectomy, depending on severity and patient preferences.
Endometriosis
Endometriosis occurs when endometrial-like tissue grows outside the uterus, leading to inflammation and scarring:
- Clinical Manifestations:
This condition is characterized by severe menstrual cramps, chronic pelvic pain, dyspareunia (painful intercourse), and sometimes infertility. - Etiology:
Although its exact cause is unclear, theories include retrograde menstruation, genetic predisposition, and immune dysfunction. - Treatment Approaches:
Management includes pain relief through NSAIDs, hormonal therapies to suppress menstruation, and surgical excision of lesions for severe cases.
Adenomyosis
Adenomyosis is defined by the invasion of endometrial tissue into the myometrium, causing uterine enlargement and pain:
- Symptoms:
Patients typically report heavy menstrual bleeding, dysmenorrhea (painful menstruation), and chronic pelvic discomfort. - Management:
Treatment options range from hormonal therapies and NSAIDs to, in extreme cases, hysterectomy, especially when reproductive preservation is not a concern.
Uterine Prolapse
Uterine prolapse occurs when the uterus descends into the vaginal canal due to weakened pelvic floor muscles and supporting ligaments:
- Risk Factors and Presentation:
Commonly associated with childbirth, aging, and menopause, symptoms include a sensation of pelvic heaviness, urinary difficulties, and a visible bulge in the vagina. - Treatment:
Non-surgical approaches include pelvic floor rehabilitation and pessary use, while surgical repair may be necessary for advanced cases.
Uterine Cancer
Endometrial (uterine) cancer is the most common gynecologic cancer in developed countries:
- Risk Profile:
It is typically associated with postmenopausal bleeding, obesity, hormonal imbalances, and genetic factors. - Diagnosis and Management:
Diagnosis involves endometrial biopsy and imaging studies, while treatment options include surgery, radiation therapy, chemotherapy, and hormone therapy, tailored to the cancer stage and patient health.
Polycystic Ovary Syndrome (PCOS)
PCOS is a hormonal disorder that affects the ovaries and often has secondary effects on the uterus:
- Clinical Features:
Women with PCOS may experience irregular menstrual cycles, heavy bleeding, and infertility, along with metabolic issues such as insulin resistance. - Management:
Treatment focuses on lifestyle modification, weight management, and medications such as hormonal contraceptives and insulin-sensitizing agents.
Asherman’s Syndrome
Asherman’s syndrome is characterized by intrauterine adhesions that often follow surgical procedures like dilation and curettage:
- Impact on Reproduction:
It may cause decreased menstrual flow, recurrent miscarriages, and infertility. - Treatment:
Hysteroscopic adhesiolysis followed by hormonal therapy to promote endometrial regeneration is the primary treatment strategy.
Uterine Polyps
Uterine polyps are growths that project from the endometrial lining and can sometimes affect menstrual regularity and fertility:
- Clinical Signs:
Symptoms include irregular bleeding, heavy menstrual flow, and intermenstrual spotting. - Intervention:
Hysteroscopic removal is the preferred method for treating symptomatic polyps, with hormone therapy considered for smaller or recurring lesions.
Understanding these common conditions is crucial for timely intervention and effective management, ensuring optimal reproductive health and quality of life.
Diagnostic Approaches
Accurate diagnosis of uterine conditions is essential for effective treatment. A variety of diagnostic tools and procedures are employed to evaluate the uterus’s structure and function.
Clinical Examination and Patient History
- Detailed Medical History:
A comprehensive history covers menstrual patterns, pain, bleeding, and reproductive history, helping to pinpoint potential uterine abnormalities. - Pelvic Examination:
A thorough pelvic exam allows clinicians to assess uterine size, shape, and mobility, and to detect anomalies such as masses or prolapse.
Imaging Techniques
- Ultrasound:
Both transabdominal and transvaginal ultrasounds provide initial, non-invasive visualization of the uterus, revealing fibroids, polyps, adenomyosis, and congenital anomalies. - Magnetic Resonance Imaging (MRI):
MRI offers high-resolution images that detail uterine tissue characteristics and are particularly useful in complex cases such as adenomyosis, endometriosis, and cancer staging. - Computed Tomography (CT) Scans:
While less common for primary uterine evaluation, CT scans assist in assessing metastatic disease in cases of uterine cancer.
Endoscopic Evaluation
- Hysteroscopy:
This procedure involves inserting a hysteroscope through the vagina and cervix into the uterine cavity, allowing direct visualization and biopsy of the endometrium. It is invaluable for diagnosing intrauterine pathologies such as polyps, adhesions, and cancer. - Laparoscopy:
Laparoscopy permits a broader evaluation of the pelvic cavity, useful for diagnosing endometriosis and pelvic adhesions, and can be both diagnostic and therapeutic.
Laboratory and Histopathological Testing
- Blood Tests:
Hormonal profiles (estrogen, progesterone, LH, FSH), complete blood counts, and tumor markers (e.g., CA-125) provide essential clues about uterine function and potential malignancies. - Endometrial Biopsy:
Tissue samples obtained via biopsy are examined histologically to diagnose conditions such as endometrial hyperplasia, chronic endometritis, and uterine cancer. - Genetic Testing:
In cases with suspected hereditary factors, genetic screening and karyotyping can reveal chromosomal abnormalities that predispose individuals to uterine disorders.
Functional Assessments
- Hysterosalpingography (HSG):
This X-ray test involves injecting contrast dye into the uterus and fallopian tubes, evaluating the shape of the uterine cavity and tubal patency—particularly important in infertility workups. - Sonohysterography:
The infusion of saline during an ultrasound enhances the visualization of the endometrial cavity, aiding in the detection of polyps, fibroids, and adhesions.
Advanced Imaging Modalities
- Fluoroscopy and PET Scans:
Fluoroscopy provides real-time imaging during contrast studies, while PET scans are used in the evaluation of metabolic activity in uterine cancers, helping to assess the extent of disease.
These diagnostic strategies, when combined, offer a comprehensive evaluation of uterine health, ensuring that conditions are accurately identified and appropriately managed.
Treatment and Intervention Options
Treatment for uterine conditions is highly individualized, based on the specific disorder, its severity, and the patient’s reproductive goals. Options range from medical management and minimally invasive procedures to advanced surgical interventions.
Medical Management
- Hormonal Therapies:
Oral contraceptives, progestins, and GnRH agonists are commonly used to manage conditions such as fibroids, endometriosis, and adenomyosis by regulating the menstrual cycle and reducing bleeding. - Nonsteroidal Anti-Inflammatory Drugs (NSAIDs):
NSAIDs alleviate pain and reduce inflammation associated with menstrual cramps, endometriosis, and adenomyosis. - Antifibrinolytics:
Tranexamic acid is used to reduce heavy menstrual bleeding by promoting clot formation. - Pain Management:
Analgesics and other supportive medications provide relief for chronic pelvic pain and discomfort.
Minimally Invasive Procedures
- Uterine Artery Embolization (UAE):
UAE is a non-surgical option for fibroid management. By blocking the blood supply to fibroids, this procedure causes them to shrink and alleviate symptoms. - Endometrial Ablation:
This technique destroys the uterine lining to treat heavy menstrual bleeding. Various energy sources, including radiofrequency and microwave, are employed. - Hysteroscopic Myomectomy and Polypectomy:
Using a hysteroscope, surgeons can remove fibroids and polyps from the uterine cavity without external incisions. - Hysteroscopic Adhesiolysis:
In cases of intrauterine adhesions (Asherman’s syndrome), a hysteroscopic procedure is used to cut and remove scar tissue, restoring the normal uterine cavity.
Surgical Interventions
- Myomectomy:
Surgical removal of fibroids while preserving the uterus is an option for women who wish to maintain fertility. - Hysterectomy:
In severe cases—such as intractable fibroids, advanced adenomyosis, or uterine cancer—a hysterectomy may be necessary. Options include total, subtotal, or radical hysterectomy, sometimes combined with pelvic lymphadenectomy. - Laparoscopic and Robotic-Assisted Surgery:
These minimally invasive approaches offer reduced recovery times and less postoperative discomfort, making them ideal for procedures such as myomectomy and hysterectomy. - Reconstructive Surgery:
In conditions like uterine prolapse, reconstructive procedures (uterine suspension) or pessary placement may be employed to restore normal pelvic anatomy.
Advanced and Innovative Therapies
- MRI-Guided Focused Ultrasound Surgery (MRgFUS):
This non-invasive method uses high-intensity ultrasound waves, guided by MRI, to heat and destroy fibroid tissue. - Radiofrequency Ablation (RFA):
RFA utilizes radiofrequency energy to shrink fibroids and reduce symptoms. - Stem Cell Therapy and Tissue Engineering:
Emerging treatments that aim to regenerate healthy uterine tissue, particularly in cases of severe endometrial damage or Asherman’s syndrome. Although still experimental, these approaches offer promise for future treatments.
Behavioral and Lifestyle Interventions
- Bladder and Pelvic Floor Rehabilitation:
Pelvic floor exercises, including Kegels, help improve pelvic support and can reduce symptoms related to uterine prolapse and incontinence. - Cognitive Behavioral Therapy (CBT):
Stress management techniques, including CBT, may help alleviate chronic pelvic pain and improve overall quality of life. - Nutritional Counseling:
Dietary modifications can support hormonal balance and reduce inflammation, which is especially beneficial in conditions like PCOS and endometriosis.
Through a combination of these interventions, treatment is tailored to each patient’s unique situation, ensuring the best possible outcomes for uterine health.
Supplemental and Nutritional Support
Nutritional supplements can serve as valuable adjuncts to conventional therapies, promoting uterine health and overall reproductive well-being. When paired with a balanced diet, these supplements help modulate hormonal levels, reduce inflammation, and support tissue repair.
Key Supplements for Uterine Health
- Vitamin D:
This essential vitamin is anti-inflammatory and plays a role in cellular growth regulation. Adequate vitamin D levels are linked to a lower risk of fibroids and improved menstrual regularity. - Omega-3 Fatty Acids:
Found in fish oil, omega-3s help reduce inflammation and menstrual pain, and they may benefit conditions like endometriosis. - Vitamin E:
An antioxidant that helps combat oxidative stress, vitamin E can alleviate symptoms of PMS and may reduce the severity of endometriosis. - Magnesium:
Magnesium is known for its muscle-relaxing properties, which can help relieve menstrual cramps and support overall uterine muscle function. - Turmeric (Curcumin):
The active compound in turmeric, curcumin, is a potent anti-inflammatory agent that may help reduce pain and inflammation in conditions such as fibroids and endometriosis. - Zinc:
Zinc supports immune function and hormone regulation, which is important for maintaining a healthy endometrium and managing conditions like PCOS. - Vitex (Chasteberry):
Vitex is a herbal supplement that promotes hormonal balance and may alleviate menstrual irregularities, PMS symptoms, and aspects of PCOS. - Green Tea Extract:
Rich in antioxidants, green tea extract can help slow the growth of fibroids and support overall uterine health. - N-acetylcysteine (NAC):
As a powerful antioxidant, NAC reduces oxidative stress and may help alleviate symptoms of PCOS and endometriosis by promoting cellular repair.
Integrating Supplements into Your Regimen
Before beginning any supplement regimen, it is essential to consult with a healthcare provider to ensure compatibility with your overall health profile. When integrated with a nutrient-dense diet, these supplements can play a pivotal role in enhancing uterine health, reducing inflammation, and improving reproductive outcomes.
Lifestyle and Preventive Strategies
A proactive approach to uterine health involves adopting healthy lifestyle habits and preventive measures. These strategies can reduce the risk of developing uterine disorders and improve overall reproductive well-being.
Daily Health Practices
- Maintain a Healthy Weight:
A balanced diet and regular exercise help manage weight, reducing the risk of hormone-related conditions such as fibroids and PCOS. - Balanced Diet:
Focus on consuming plenty of fruits, vegetables, whole grains, and lean proteins. This nutritional approach supports hormonal balance and reduces inflammation. - Regular Exercise:
Physical activity improves blood circulation, supports metabolic health, and reduces stress, all of which contribute to better uterine function. - Stress Management:
Techniques such as yoga, meditation, and mindfulness can lower stress levels, which in turn may reduce the severity of uterine pain and menstrual irregularities. - Avoid Smoking and Limit Alcohol:
Smoking and excessive alcohol consumption can disrupt hormonal balance and increase the risk of uterine conditions. - Monitor Menstrual Cycles:
Keeping a menstrual diary can help detect irregularities early, allowing for prompt medical consultation if significant changes occur. - Practice Safe Sex:
Using protection and following safe sex practices can help prevent infections that may affect uterine health. - Regular Medical Check-Ups:
Routine gynecological exams are crucial for early detection of uterine abnormalities, enabling timely intervention. - Educate Yourself:
Staying informed about the latest research and treatment options empowers you to make better decisions regarding your reproductive health.
By incorporating these preventive measures into your daily routine, you can help safeguard uterine health and enhance your overall quality of life.
Trusted Resources
Staying updated with reliable information is key to managing uterine health effectively. Below are some authoritative resources for further reading and guidance.
Books
- “The Vagina Bible: The Vulva and the Vagina—Separating the Myth from the Medicine” by Dr. Jen Gunter
A comprehensive guide to female reproductive health that covers uterine anatomy and common conditions. - “Taking Charge of Your Fertility” by Toni Weschler
An essential resource for understanding the menstrual cycle, fertility, and overall reproductive health, with insights into uterine function. - “Our Bodies, Ourselves” by the Boston Women’s Health Book Collective
A classic resource that provides a wealth of information on women’s health, including detailed discussions on uterine conditions and care.
Academic Journals
- The Journal of Obstetrics and Gynaecology Research
This peer-reviewed journal publishes the latest research, reviews, and clinical studies related to uterine health and reproductive medicine. - Human Reproduction
A leading journal in reproductive biology that covers advanced research on uterine function, infertility, and gynecological disorders.
Mobile Apps and Online Tools
- Clue
A popular period and ovulation tracker that helps women monitor their menstrual cycles and identify any irregularities that may signal uterine issues. - Flo
An app designed to track menstrual cycles, ovulation, and related symptoms, offering personalized insights into reproductive health. - Ovia Health
A suite of apps that provides comprehensive support across various stages of reproductive health, including fertility and pregnancy management.
Frequently Asked Questions
What are the primary functions of the uterus?
The uterus primarily supports menstruation, pregnancy, and childbirth. It regenerates its lining each cycle, provides a nurturing environment for a fertilized egg, and contracts during labor to facilitate childbirth.
How is uterine fibroid diagnosed?
Fibroids are typically diagnosed via pelvic ultrasound, MRI, or hysteroscopy. These imaging techniques reveal the size, location, and number of fibroids, guiding treatment decisions.
What treatment options are available for endometriosis?
Treatment for endometriosis includes pain relief with NSAIDs, hormonal therapies to suppress the menstrual cycle, and surgical removal of endometrial implants in severe cases.
How can lifestyle changes improve uterine health?
Maintaining a healthy weight, following a balanced diet, exercising regularly, managing stress, and monitoring menstrual cycles can significantly reduce the risk of uterine disorders and improve overall reproductive health.
What supplements are beneficial for uterine health?
Supplements like vitamin D, omega-3 fatty acids, vitamin E, magnesium, turmeric, zinc, and chasteberry can help balance hormones, reduce inflammation, and support uterine function.
Disclaimer
The information provided in this article is intended for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a qualified healthcare provider for personalized guidance and treatment.
Please share this article on Facebook, X (formerly Twitter), or your preferred platform to help promote awareness of uterine health and encourage proactive reproductive care.