The vagina is a central component of the female reproductive system, playing a vital role in sexual intercourse, menstruation, and childbirth. This resilient, flexible muscular canal is designed to protect internal reproductive organs, facilitate reproductive processes, and maintain overall gynecologic health. Throughout a woman’s life, its structure and function adapt to hormonal fluctuations, sexual activity, and reproductive changes. In this comprehensive guide, we explore every aspect of vaginal health—from detailed anatomy and physiological roles to common disorders and the latest treatment options. We also provide practical lifestyle tips and nutritional strategies to help you maintain optimal vaginal health.
Table of Contents
- Anatomical Structure
- Functional Roles & Regulation
- Common Vaginal Disorders
- Diagnostic Methods
- Treatment & Intervention Options
- Supplemental & Nutritional Strategies
- Lifestyle & Preventive Measures
- Trusted Resources
- Frequently Asked Questions
Anatomical Structure
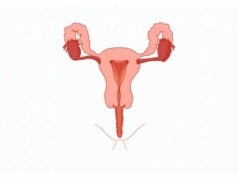
The vagina is a complex, multi-layered muscular canal that extends from the vulvar vestibule to the cervix, forming an integral part of the female reproductive system. Its anatomy is meticulously designed to perform a range of functions including sexual intercourse, passage of menstrual blood, and serving as a birth canal during labor.
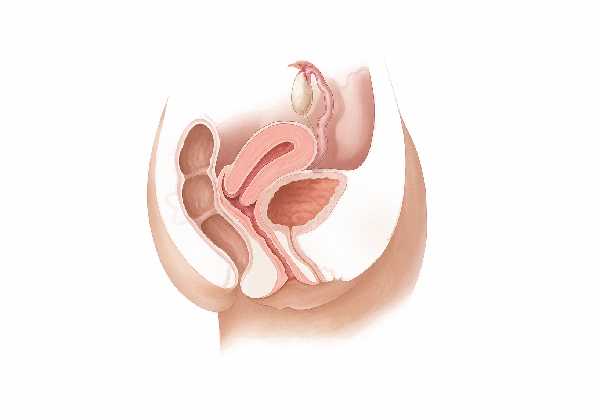
Location and Gross Anatomy
Positioned deep within the pelvic cavity, the vagina lies posterior to the urethral opening and anterior to the anus. It forms the central passage of the vulva, which is the external part of the female genitalia. When unstimulated, the vagina typically measures about 7 to 10 centimeters in length; however, its walls are remarkably elastic, allowing significant expansion during sexual arousal and childbirth.
Key external features include:
- Vaginal Introitus: The external opening is framed by the labia minora and labia majora, which not only provide protection but also contribute to the aesthetic and functional aspects of the vulva.
- Hymen: Often considered a remnant of embryonic development, the hymen is a thin membrane that partially covers the vaginal opening in some women. Its appearance and integrity can vary widely depending on genetic, cultural, and physical factors.
Internal Composition and Layers
The vaginal wall is composed of multiple layers that work together to ensure durability, flexibility, and protection:
- Mucosal Layer (Vaginal Epithelium):
- The innermost lining is made of non-keratinized stratified squamous epithelium, which provides robust protection against friction and microbial invasion.
- This layer is rich in glycogen, which helps maintain an acidic pH when metabolized by resident Lactobacillus species, thus creating a natural defense against pathogens.
- Numerous rugae (folds) in the mucosa allow for expansion during intercourse and childbirth.
- Lamina Propria:
- Located just beneath the epithelial lining, this connective tissue layer contains a dense network of blood vessels, lymphatics, and nerve fibers.
- It provides structural support and nourishment to the mucosa and plays a role in immune defense.
- Muscular Layer (Muscularis):
- Comprising inner circular and outer longitudinal layers of smooth muscle, the muscularis is responsible for the vagina’s ability to contract and expand.
- These muscular fibers contribute to sexual function by enhancing sensation and are critical during childbirth as they facilitate the dilation and contraction of the birth canal.
- Adventitia:
- The outermost layer consists of loose connective tissue that anchors the vagina to surrounding pelvic structures.
- It blends with the connective tissues of the pelvic floor, providing additional support and flexibility.
Vascular and Neural Supply
A healthy vaginal function depends on a rich supply of blood and an intricate network of nerves:
- Arterial Supply:
- The vagina is primarily supplied by the vaginal arteries, which are branches of the internal iliac arteries. Additional contributions come from the uterine and internal pudendal arteries.
- Venous Drainage:
- Venous blood is collected via the vaginal venous plexus and drains into the internal iliac veins.
- Nerve Supply:
- Sensory and autonomic innervation is provided by branches of the pudendal nerve and the uterovaginal plexus, a branch of the inferior hypogastric plexus.
- This neural network is crucial for sexual arousal, lubrication, and maintaining overall vaginal sensitivity.
Lymphatic Drainage
The lymphatic system plays a significant role in immune surveillance and fluid balance:
- Upper Vagina:
- Lymph drains primarily into the internal iliac lymph nodes.
- Lower Vagina:
- Lymphatic drainage from the lower portion is directed to the superficial inguinal lymph nodes.
- This efficient lymphatic drainage helps prevent the spread of infections and is an important consideration in the management of vaginal and cervical cancers.
Supportive Structures
The vagina is supported by various ligaments and muscles that maintain its position and function:
- Pelvic Floor Muscles:
- Muscles such as the levator ani and coccygeus provide a muscular diaphragm that supports the vagina, contributing to continence and sexual function.
- Urogenital Diaphragm:
- This structure offers additional support, helping to maintain the integrity of the vaginal canal.
- Connective Tissue and Ligaments:
- Structures such as the cardinal and uterosacral ligaments anchor the vagina and uterus, ensuring they remain properly aligned within the pelvis.
Microbiota
A healthy vaginal ecosystem is maintained by its unique microbiota:
- Lactobacillus Dominance:
- The vaginal flora is predominantly composed of Lactobacillus species, which ferment glycogen to produce lactic acid, maintaining an acidic pH (3.8–4.5) that is inhospitable to many pathogens.
- Balanced Ecosystem:
- A balanced microbial environment is crucial for preventing infections and sustaining overall vaginal health. Disruptions in this balance can lead to conditions such as bacterial vaginosis or yeast infections.
Anatomical Variations and Clinical Relevance
The vaginal anatomy can vary among individuals due to factors such as age, hormonal status, childbirth, and congenital differences:
- Congenital Anomalies:
- Conditions like a septate vagina (a partition within the vaginal canal) or vaginal agenesis (absence of the vagina) require specialized management and can impact fertility.
- Age-Related Changes:
- Postmenopausal women may experience thinning of the vaginal walls, decreased lubrication, and increased susceptibility to infections due to lower estrogen levels.
Understanding the detailed anatomy of the vagina is essential for diagnosing gynecologic conditions, planning surgical interventions, and promoting overall sexual and reproductive health.
Functional Roles & Regulation
The vagina is a multifunctional organ integral to sexual health, reproduction, and overall well-being. Its functions extend beyond serving as a passage for menstrual flow and childbirth; it also plays a pivotal role in sexual pleasure and acts as a first line of defense against infections.
Sexual Function and Intercourse
- Receptivity and Lubrication:
- During sexual arousal, increased blood flow and hormonal signals stimulate the vaginal walls to secrete natural lubricants.
- This lubrication reduces friction and enhances comfort during intercourse.
- Elasticity and Expansion:
- The presence of rugae and flexible muscle fibers allows the vagina to expand significantly to accommodate the penis during intercourse.
- The muscular contractions also contribute to sexual pleasure by enhancing sensation.
Menstrual Flow and Reproductive Cycle
- Menstrual Passage:
- The vagina serves as the exit route for menstrual blood and tissue, which is shed from the endometrium during menstruation.
- The efficient passage of menstrual fluid is essential for clearing the uterine cavity and preparing for the next cycle.
- Cyclic Changes:
- Hormones such as estrogen and progesterone regulate changes in the vaginal epithelium throughout the menstrual cycle, ensuring an optimal environment for both sexual activity and protection against pathogens.
Role in Childbirth
- Birth Canal Function:
- During labor, the vagina stretches considerably to allow the passage of the baby.
- The coordinated contraction of the pelvic floor muscles, along with the elasticity of the vaginal walls, is critical during delivery.
- Postpartum Recovery:
- After childbirth, the vagina gradually returns to its pre-pregnancy state. Factors such as episiotomy or tearing may influence the recovery process and necessitate rehabilitative measures.
Defense and Immune Mechanisms
- Acidic Environment:
- The production of lactic acid by Lactobacillus species creates an acidic pH that inhibits the growth of harmful bacteria and yeast.
- Mucosal Barrier:
- The stratified squamous epithelium forms a protective barrier against pathogens, while secretions from vaginal glands help trap and flush out invaders.
- Immune Surveillance:
- Immune cells within the vaginal mucosa detect and respond to pathogens, playing a key role in maintaining a healthy vaginal environment.
Hormonal and Neural Regulation
- Hormonal Influences:
- Estrogen and progesterone profoundly influence vaginal tissue, regulating lubrication, elasticity, and immune function.
- Fluctuations in these hormones during the menstrual cycle and menopause significantly impact vaginal health.
- Neural Input:
- A dense network of sensory and autonomic nerves innervates the vagina, contributing to sexual pleasure and modulating physiological responses during arousal and intercourse.
Sensory and Psychological Factors
- Enhanced Sensitivity:
- Numerous nerve endings in the vaginal walls transmit pleasurable sensations during sexual activity.
- These sensory inputs not only enhance sexual pleasure but also contribute to emotional intimacy and overall quality of life.
- Psychological Well-being:
- Positive sexual experiences and a healthy vaginal environment are closely linked to overall mental and emotional health, emphasizing the importance of maintaining vaginal wellness.
The coordinated interplay of these functions underscores the vagina’s essential role in reproductive health and sexual function, highlighting why maintaining its health is paramount.
Common Vaginal Disorders
A variety of conditions can affect the vagina, disrupting its normal function and impacting a woman’s quality of life. Early diagnosis and appropriate treatment are essential to managing these disorders effectively.
Vaginitis
Vaginitis refers to inflammation of the vaginal walls and can be caused by infectious agents or non-infectious irritants.
- Bacterial Vaginosis (BV):
- Caused by an imbalance in the vaginal microbiota, leading to a reduction in Lactobacillus and overgrowth of anaerobic bacteria.
- Symptoms include a thin, grayish-white discharge with a strong fishy odor, along with itching or burning.
- Yeast Infections (Candidiasis):
- Overgrowth of Candida species, particularly Candida albicans, results in thick, white, cottage cheese-like discharge, intense itching, and irritation.
- Trichomoniasis:
- A sexually transmitted infection caused by the protozoan Trichomonas vaginalis, characterized by a frothy, yellow-green discharge, itching, and discomfort.
Vaginal Atrophy (Atrophic Vaginitis)
Vaginal atrophy typically occurs in postmenopausal women due to decreased estrogen levels.
- Symptoms:
- Thinning and drying of the vaginal walls, itching, burning, and painful intercourse (dyspareunia).
- Increased susceptibility to infections and urinary symptoms.
- Management:
- Local estrogen therapy and lubricants can help restore vaginal tissue integrity and alleviate discomfort.
Vulvodynia
Vulvodynia is a chronic pain syndrome affecting the vulva and sometimes the vagina, without an identifiable cause.
- Presentation:
- Persistent burning, stinging, or irritation around the vaginal opening, which may occur continuously or intermittently.
- The pain can significantly impact sexual function and quality of life.
- Treatment:
- Management typically involves a multidisciplinary approach including medications (topical anesthetics, antidepressants), physical therapy, and counseling.
Vaginal Prolapse
Vaginal prolapse occurs when weakened pelvic support structures cause the vaginal walls to sag or protrude into the vaginal canal.
- Risk Factors:
- Childbirth, aging, menopause, obesity, and chronic straining can all contribute to prolapse.
- Symptoms:
- A sensation of pelvic pressure, discomfort during intercourse, urinary difficulties, and visible bulging.
- Treatment:
- Options include pelvic floor exercises, pessary devices, and surgical repair in more severe cases.
Lichen Sclerosus
Lichen sclerosus is a chronic inflammatory skin condition that can affect the vulva and sometimes the vagina.
- Symptoms:
- White, patchy, thin skin that is often itchy, painful, and prone to tearing.
- It can cause significant discomfort and affect sexual activity.
- Management:
- Topical corticosteroids are the mainstay of treatment, with additional supportive measures to maintain skin health.
Vaginal Cancer
Although rare, vaginal cancer can occur, usually in older women.
- Presentation:
- Symptoms may include abnormal vaginal bleeding, a mass or lump in the vagina, pain during intercourse, and persistent pelvic pain.
- Diagnosis and Treatment:
- Diagnosis is made via biopsy, imaging, and endoscopic evaluation, with treatment options including surgery, radiation, and chemotherapy.
Sexually Transmitted Infections (STIs)
Several STIs can affect the vagina, disrupting its normal flora and causing inflammation.
- HPV (Human Papillomavirus):
- Certain strains of HPV can cause genital warts and are associated with a risk of cervical and vaginal cancer.
- Chlamydia and Gonorrhea:
- These bacterial infections may cause abnormal discharge, pain during urination, and pelvic pain if left untreated.
- Herpes Simplex Virus (HSV):
- Causes recurrent painful lesions and can lead to systemic symptoms during outbreaks.
Bartholin’s Cyst
Bartholin’s cysts occur when the ducts of the Bartholin glands (located on either side of the vaginal opening) become blocked.
- Symptoms:
- A painful, swollen lump near the vaginal opening that may become infected, forming an abscess.
- Management:
- Treatment options include warm compresses, drainage, and, if recurrent, surgical excision.
Dyspareunia
Dyspareunia, or painful intercourse, can result from a variety of causes, ranging from infections to anatomical abnormalities.
- Causes:
- Vaginal dryness, infections, structural issues, or psychological factors.
- Management:
- Treatment depends on the underlying cause and may involve lubricants, hormone therapy, pain management, or counseling.
Understanding these disorders is essential for timely intervention, enabling effective treatment and improved quality of life.
Diagnostic Methods
A thorough diagnosis of vaginal disorders relies on a combination of clinical evaluation, laboratory testing, imaging studies, and endoscopic procedures. These tools allow healthcare providers to determine the underlying cause and severity of the condition.
Clinical Examination and History
- Patient History:
- Collecting detailed information about menstrual cycles, sexual activity, pain, discharge, and previous infections helps form a comprehensive picture of the patient’s vaginal health.
- Physical Examination:
- A pelvic exam is crucial for assessing the external and internal structures of the vagina, detecting signs of inflammation, lesions, prolapse, or anatomical abnormalities.
Laboratory Investigations
- Vaginal Swabs:
- Swab tests are used to collect samples of vaginal secretions for microscopic examination and culture, aiding in the diagnosis of infections such as bacterial vaginosis, yeast infections, and trichomoniasis.
- pH Testing:
- Vaginal pH is measured using pH strips. Normal pH ranges between 3.8 and 4.5; deviations can indicate infections or imbalances in the vaginal microbiota.
- Nucleic Acid Amplification Tests (NAATs):
- These highly sensitive tests detect the genetic material of pathogens responsible for STIs, providing accurate identification of infections like chlamydia and gonorrhea.
Imaging Studies
- Ultrasound:
- Transabdominal and transvaginal ultrasound are effective in visualizing the vagina and surrounding pelvic structures, helping to diagnose conditions such as prolapse, cysts, or masses.
- Magnetic Resonance Imaging (MRI):
- MRI offers high-resolution images that are particularly useful in evaluating complex conditions like deep infiltrating endometriosis and vaginal cancer.
- Computed Tomography (CT) Scans:
- Although less common for primary vaginal evaluation, CT scans can provide detailed cross-sectional images when needed for complex cases.
Endoscopic Techniques
- Colposcopy:
- A colposcope is used to magnify and examine the vaginal and cervical epithelium, especially useful in cases of abnormal Pap smears or suspected precancerous changes.
- Cystoscopy:
- When bladder involvement is suspected, a cystoscopy may be performed to evaluate the urethra and bladder from the vaginal perspective.
Biopsy and Histopathology
- Tissue Biopsy:
- When suspicious lesions are found, a small tissue sample is removed for histological analysis. This is critical for diagnosing conditions such as lichen sclerosus, vaginal intraepithelial neoplasia, and vaginal cancer.
- Histopathological Examination:
- Microscopic examination of biopsy specimens confirms the diagnosis and guides treatment planning.
Functional Assessments
- Urodynamic Testing:
- Although primarily used for urinary disorders, urodynamic tests can help evaluate the impact of vaginal prolapse on bladder function.
- Pap Smear:
- This screening tool, while focused on cervical cytology, can also provide information about the vaginal epithelium and detect signs of infection or dysplasia.
Advanced and Emerging Technologies
- Optical Coherence Tomography (OCT):
- OCT is an emerging imaging modality that provides high-resolution cross-sectional images of vaginal tissues, potentially identifying early changes in tissue structure.
- Fluorescence Spectroscopy:
- This technique detects biochemical changes in vaginal tissues, aiding in the early detection of precancerous and cancerous lesions.
These comprehensive diagnostic methods enable clinicians to accurately assess vaginal health and tailor treatment plans to each patient’s unique condition.
Treatment & Intervention Options
The treatment of vaginal disorders is multifaceted, ranging from conservative medical management to advanced surgical interventions. Treatment is tailored to the individual, based on the underlying cause, symptom severity, and reproductive goals.
Medical Management
- Antibiotic and Antifungal Therapy:
- Bacterial Vaginosis: Treated with metronidazole or clindamycin.
- Yeast Infections: Managed with antifungal agents such as fluconazole or topical miconazole.
- Trichomoniasis: Oral metronidazole or tinidazole is used for treatment.
- Hormonal Therapies:
- Vaginal Atrophy: Local estrogen creams, rings, or tablets can restore vaginal lubrication and thickness.
- Menstrual Disorders: Hormonal contraceptives may be prescribed to regulate cycles and alleviate symptoms.
- Pain Relief:
- NSAIDs and topical analgesics (such as lidocaine) help manage pain associated with conditions like vulvodynia and endometriosis.
- Antifibrinolytics:
- In cases of heavy menstrual bleeding, tranexamic acid can reduce blood loss by promoting clot stability.
Minimally Invasive Procedures
- Laser Therapy:
- CO2 and fractional lasers are used to treat vaginal atrophy and tighten the vaginal canal by stimulating collagen production.
- Radiofrequency Treatments:
- Radiofrequency energy treatments, such as ThermiVa, improve vaginal tone, elasticity, and lubrication, benefiting women with vaginal laxity or atrophy.
- Endoscopic Procedures:
- Hysteroscopic Resection: Removal of intrauterine polyps or adhesions via a hysteroscope.
- Colposcopic Excision: For precancerous lesions or localized areas of dysplasia.
Surgical Interventions
- Labiaplasty:
- Surgical modification of the labia minora or majora can be performed to correct congenital anomalies, relieve discomfort, or enhance aesthetic appearance.
- Vaginal Prolapse Repair:
- Procedures such as anterior or posterior colporrhaphy, sacrocolpopexy, or vaginal mesh repair restore pelvic organ support in cases of prolapse.
- Excisional Surgery for Neoplasms:
- Surgical removal of malignant or precancerous lesions is necessary in cases of vaginal cancer or severe dysplasia.
- Bartholin’s Gland Surgery:
- Drainage or excision of Bartholin’s cysts and abscesses alleviates pain and prevents recurrence.
Advanced and Innovative Treatments
- Platelet-Rich Plasma (PRP) Therapy:
- PRP injections, derived from the patient’s own blood, are used for vaginal rejuvenation, promoting tissue repair, improved lubrication, and enhanced sexual function.
- Stem Cell and Tissue Engineering Approaches:
- Emerging therapies aim to regenerate vaginal tissue in cases of severe atrophy or congenital defects. Although still experimental, these approaches hold promise for future restorative treatments.
- Bioidentical Hormone Replacement Therapy (BHRT):
- BHRT uses hormones that are chemically identical to those produced by the body, providing a more natural option for managing menopausal symptoms and maintaining vaginal health.
Behavioral and Lifestyle Interventions
- Pelvic Floor Rehabilitation:
- Kegel exercises and physical therapy help strengthen the pelvic floor muscles, improving support for the vagina and reducing symptoms of prolapse and incontinence.
- Cognitive Behavioral Therapy (CBT):
- CBT can assist in managing chronic pain conditions such as vulvodynia by addressing the psychological components of pain.
- Dietary and Lifestyle Modifications:
- Adjustments in diet, such as reducing sugar and processed foods, can help manage inflammation. Adequate hydration and stress management further support vaginal health.
These varied treatment options ensure that therapy is individualized to each patient’s needs, promoting optimal outcomes and improved quality of life.
Supplemental & Nutritional Strategies
Nutritional and supplemental interventions can serve as valuable adjuncts to traditional therapies, helping to maintain vaginal health by reducing inflammation, balancing hormones, and supporting the immune system.
Key Nutritional Supplements
- Probiotics:
- Particularly Lactobacillus strains are critical for maintaining a healthy vaginal microbiota. Probiotics help sustain the acidic pH essential for preventing infections such as bacterial vaginosis and yeast infections.
- Vitamin D:
- With its anti-inflammatory properties, vitamin D supports immune function and is associated with a lower risk of vaginal infections and inflammatory conditions like lichen sclerosus.
- Omega-3 Fatty Acids:
- Found in fish oil, these essential fatty acids reduce inflammation and may alleviate discomfort associated with vaginal atrophy and chronic pelvic pain.
- Vitamin E:
- An antioxidant that promotes healthy tissue repair and improves vaginal lubrication and elasticity.
- Magnesium:
- Magnesium aids in muscle relaxation, which can reduce menstrual cramps and enhance overall vaginal comfort.
- Turmeric (Curcumin):
- Curcumin’s powerful anti-inflammatory and antioxidant effects may help reduce pain and inflammation in conditions such as endometriosis and fibroids.
- Zinc:
- Zinc supports hormone regulation and immune function, both of which are vital for maintaining a healthy vaginal environment.
- Chasteberry (Vitex):
- A herbal supplement that helps balance hormones and may alleviate symptoms of premenstrual syndrome (PMS) and irregular cycles.
- Cranberry Extract:
- Widely used for its role in preventing urinary tract infections by inhibiting bacterial adhesion, cranberry extract indirectly benefits vaginal health.
Integrating Supplements into Daily Life
Before starting any supplement regimen, it is important to consult with a healthcare provider. When used alongside a balanced diet rich in fruits, vegetables, whole grains, and lean proteins, these supplements can enhance the natural defense mechanisms of the vagina, support hormonal balance, and contribute to overall reproductive health.
Lifestyle & Preventive Measures
Preventing vaginal disorders and maintaining optimal health involves adopting proactive lifestyle habits. These measures help sustain the delicate balance of the vaginal environment and protect against infections and other conditions.
Daily Practices
- Maintain Excellent Hygiene:
- Use mild, unscented cleansers and water for washing the external genitalia. Avoid douching, which can disrupt the natural microbiota.
- Wear Breathable Clothing:
- Opt for cotton underwear and loose-fitting clothing to reduce moisture buildup and friction, which can predispose to irritation and infections.
- Stay Hydrated:
- Drinking ample water supports overall health and aids in maintaining adequate vaginal lubrication.
- Practice Safe Sexual Habits:
- Use condoms and engage in safe sexual practices to reduce the risk of sexually transmitted infections (STIs) that can affect vaginal health.
- Monitor Your Menstrual Cycle:
- Keeping a menstrual diary can help you detect irregularities or changes that might signal an underlying condition.
- Regular Gynecological Exams:
- Routine check-ups with your healthcare provider allow for early detection and treatment of vaginal and reproductive issues.
Pelvic and Lifestyle Wellness
- Pelvic Floor Exercises:
- Regular Kegel exercises help strengthen pelvic floor muscles, improving support for the vagina and reducing the risk of prolapse and incontinence.
- Balanced Diet and Weight Management:
- A nutrient-rich diet and regular physical activity contribute to hormonal balance and reduce inflammation, lowering the risk of conditions such as fibroids and PCOS.
- Stress Reduction:
- Techniques such as yoga, meditation, and mindfulness not only improve mental health but also positively impact hormonal balance and reduce symptoms associated with chronic pelvic pain.
- Avoid Irritants:
- Refrain from using scented hygiene products, tampons, or douches that can disrupt the vaginal flora and irritate the sensitive mucosal surfaces.
- Educate Yourself:
- Staying informed about reproductive health and the latest research empowers you to make proactive decisions regarding your well-being.
Adopting these lifestyle and preventive strategies can greatly enhance vaginal health and overall quality of life.
Trusted Resources
Reliable information is essential for making informed decisions about vaginal health. The following resources provide comprehensive, evidence-based guidance for both patients and healthcare professionals.
Books
- “The Vagina Bible: The Vulva and the Vagina—Separating the Myth from the Medicine” by Dr. Jen Gunter
- This guide dispels common myths and provides accurate, in-depth information on vaginal anatomy, health, and common disorders.
- “Taking Charge of Your Fertility” by Toni Weschler
- This book offers insights into menstrual and reproductive health, including detailed discussions on vaginal function and fertility.
- “Our Bodies, Ourselves” by the Boston Women’s Health Book Collective
- A classic resource covering a wide range of topics related to women’s health, including comprehensive information on the vagina.
Academic Journals
- The Journal of Obstetrics and Gynaecology Research
- A peer-reviewed journal that publishes cutting-edge research and clinical studies on vaginal health and gynecological disorders.
- Human Reproduction
- This leading journal covers advanced research in reproductive biology, including studies on vaginal physiology and pathology.
Mobile Apps and Online Tools
- Clue:
- A period and ovulation tracker that helps women monitor their reproductive health and detect any irregularities.
- Flo:
- An app designed for menstrual cycle tracking, offering personalized insights and reminders to support overall reproductive well-being.
- Ovia Health:
- A suite of apps providing information and support throughout different stages of reproductive health, including fertility and pregnancy.
Frequently Asked Questions
What are the primary functions of the vagina?
The vagina serves as a canal for sexual intercourse, allows for the passage of menstrual flow, and functions as the birth canal during childbirth. It also plays a protective role by maintaining an acidic environment to prevent infections.
How is vaginitis diagnosed?
Vaginitis is diagnosed through a combination of patient history, physical examination, vaginal swabs for microscopy and culture, pH testing, and nucleic acid amplification tests (NAATs) to detect specific pathogens.
What treatment options exist for vaginal atrophy?
Vaginal atrophy is commonly treated with local estrogen therapy (creams, rings, tablets) and lubricants. In some cases, lifestyle changes and systemic hormone replacement therapy may also be recommended.
How can lifestyle changes improve vaginal health?
Maintaining good hygiene, wearing breathable clothing, staying hydrated, practicing safe sex, and engaging in pelvic floor exercises all contribute to a healthy vaginal environment and reduce the risk of infections and irritation.
What supplements support vaginal health?
Supplements such as probiotics (especially Lactobacillus strains), vitamin D, omega-3 fatty acids, vitamin E, magnesium, turmeric, and cranberry extract help maintain a balanced vaginal microbiome, reduce inflammation, and support overall reproductive health.
Disclaimer
The information provided in this article is intended for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a qualified healthcare provider for personalized guidance and treatment.
Please share this article on Facebook, X (formerly Twitter), or your preferred platform to help promote awareness of vaginal health and encourage proactive reproductive care.