What is Acanthamoeba Keratitis?
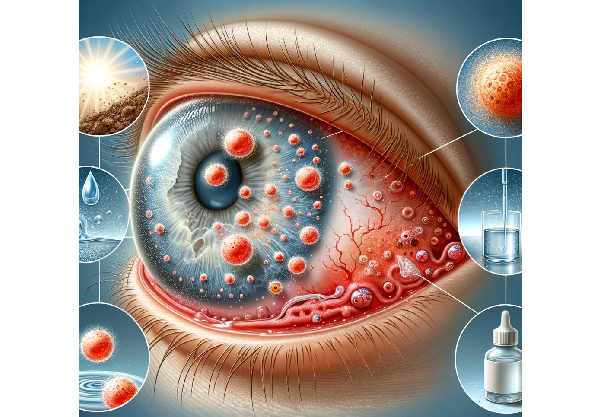
Acanthamoeba keratitis is a rare but serious eye infection caused by the free-living amoeba Acanthamoeba, which can be found in various water sources, soil, and air. This infection primarily affects the cornea, the clear, dome-shaped surface that protects the front of the eye. If not treated promptly, the condition can cause severe pain, vision loss, and, in extreme cases, blindness. Awareness of acanthamoeba keratitis is critical, especially for contact lens users who are more vulnerable due to potential exposure from contaminated water and poor lens hygiene. Early detection and treatment are critical for preventing complications and maintaining vision.
Understanding The Condition
Acanthamoeba keratitis is defined as a progressive infection of the cornea caused by Acanthamoeba species. This condition can cause significant visual impairment and is difficult to diagnose and treat due to the causative organism’s resilience and ability to exist in two forms: the trophozoite and the cyst.
Causes and Risk Factors
The main causes and risk factors of acanthamoeba keratitis are:
- Contact Lens Use: The majority of acanthamoeba keratitis cases are associated with contact lens wear. Poor hygiene practices, such as cleaning lenses with tap water, wearing lenses while swimming or showering, and failing to replace lens cases on a regular basis, can all introduce Acanthamoeba into the eye.
- Exposure to Contaminated Water: Activities that involve contact with potentially Acanthamoeba-contaminated water sources, such as swimming in pools, lakes, or hot tubs without proper eye protection, increase the risk of infection.
- Corneal Trauma: Minor corneal injuries, such as scratches or abrasions, can allow Acanthamoeba to enter the eye and cause infection.
- Immune System Compromise: People with weakened immune systems are more vulnerable to a variety of infections, including Acanthamoeba keratitis.
Pathophysiology
Acanthamoeba has two forms: active trophozoites and dormant cysts. Both forms can be found in infected tissues, helping the infection to persist and resist treatment.
- Adherence and Invasion: The infection begins when Acanthamoeba attaches to the corneal epithelium via mannose-binding proteins. Once attached, trophozoites produce enzymes such as proteases, which degrade the corneal epithelium and stroma, allowing for deeper penetration into the corneal layers.
- Cyst Formation: When exposed to harsh conditions, trophozoites can transform into cysts that are extremely resistant to environmental stress, disinfectants, and therapeutic agents. This cyst form enables the organism to survive in harsh environments, making treatment more challenging.
- Inflammation and Damage: The presence of Acanthamoeba in the cornea causes a significant inflammatory response. The immune system’s reaction causes the infiltration of immune cells like neutrophils, resulting in corneal ulcers and stromal inflammation. Inflammation and tissue damage cause severe pain, photophobia (light sensitivity), and visual impairment.
Symptoms
The symptoms of acanthamoeba keratitis can vary, but frequently include:
- Severe Eye Pain: Pain is frequently disproportionate to clinical findings and is a defining feature of the condition.
- Redness: The affected eye looks red and inflamed.
- Photophobia: A heightened sensitivity to light is common.
- Blurred Vision: As the infection progresses, vision may become more blurred.
- Tearing and Discharge: The affected eye usually produces excessive tearing and discharge.
- Ring Infiltrate: One of the hallmarks of advanced acanthamoeba keratitis is the presence of a ring-like infiltrate in the corneal stroma.
Diagnostics
The diagnosis of acanthamoeba keratitis can be difficult due to its rarity and symptoms’ similarity to other more common eye infections. Early and accurate diagnosis is critical for successful treatment and avoiding serious complications.
Prognosis
The prognosis for acanthamoeba keratitis varies according to the time of diagnosis and the efficacy of treatment. Early diagnosis and treatment are associated with better outcomes, whereas delayed treatment can lead to significant visual impairment or blindness.
Diagnostic methods
Acanthamoeba keratitis is diagnosed using a combination of clinical suspicion, laboratory testing, and advanced imaging techniques. The following are standard and innovative diagnostic methods for confirming the presence of Acanthamoeba in the cornea:
Clinical Evaluation
An ophthalmologist’s thorough clinical evaluation is the first step in diagnosing acanthamoeba keratitis. Severe eye pain, redness, photophobia, and visual disturbances are common clinical presentation features. The presence of a ring infiltrate in the cornea indicates advanced infection.
Microscopic Examination
- Corneal Scraping: Corneal scraping is the process of obtaining a sample of corneal tissue with a sterile instrument. The sample is then examined under a microscope to detect Acanthamoeba trophozoites and cysts. Special staining techniques, such as Giemsa or calcofluor white staining, can improve the visibility of organisms.
- Confocal Microscopy: Confocal microscopy is a non-invasive imaging technique that enables high-resolution visualization of corneal layers in real time. This method detects Acanthamoeba cysts and trophozoites in corneal tissue, allowing for early diagnosis of the infection.
Culture
Culturing corneal samples on non-nutrient agar plates seeded with E. coli can promote the growth of Acanthamoeba trophozoites, which can then be detected microscopically. While culture is a reliable diagnostic method, it is time-consuming and may not always produce positive results.
Molecular Techniques
- Polymerase Chain Reaction (PCR) is a highly sensitive and specific molecular technique for detecting Acanthamoeba DNA in corneal samples. This method can provide a quick and accurate diagnosis, even with small amounts of the organism.
Advanced Imaging
- Anterior Segment Optical Coherence Tomography (AS-OCT): AS-OCT produces high-resolution cross-sectional images of the cornea, allowing for detailed examination of its layers. This method can aid in identifying characteristic features of acanthamoeba keratitis and tracking treatment response.
- In Vivo Confocal Microscopy (IVCM): IVCM is an effective method for visualizing Acanthamoeba cysts and trophozoites in the cornea. It provides high magnification and resolution, allowing for early detection and assessment of the infection.
Using a combination of these diagnostic methods, healthcare professionals can accurately diagnose acanthamoeba keratitis and begin appropriate treatment to avoid serious complications and preserve vision.
Treatment
Acanthamoeba keratitis is difficult to treat because the organism can form cysts that are highly resistant to treatment. Successful treatment frequently necessitates a combination of medications and, in severe cases, surgical intervention.
Medications
- Topical Antimicrobials: The primary treatment for acanthamoeba keratitis is the use of topical antimicrobials. Commonly used medications include:
- Biguanides: Polyhexamethylene biguanide (PHMB) and chlorhexidine work against both trophozoites and cysts.
- Diamidines: Propamidine isethionate (Brolene) and hexamidine have been shown to effectively treat acanthamoeba infections.
- Aminoglycosides: Neomycin is occasionally used, but it is not as effective as biguanides and diamidines.
- Combination Therapy: Several of the agents listed above are frequently used in combination to improve efficacy. Treatment typically begins with high doses and gradually tapers as the infection responds.
- Oral Antifungals: When topical treatment is insufficient, oral antifungals such as itraconazole or voriconazole, which are particularly effective against cysts, may be added to the regimen.
Surgical Interventions
- Debridement: Corneal debridement is the removal of infected epithelial tissue with the goal of reducing microbial load and improving topical medication penetration. This procedure can alleviate symptoms while also increasing treatment efficacy.
- Keratoplasty: In severe or refractory cases, a corneal transplant (keratoplasty) may be indicated. This entails replacing infected corneal tissue with healthy donor tissue. Depending on the severity of the infection, either penetrating keratoplasty (full-thickness transplant) or lamellar keratoplasty (partial-thickness transplant) can be performed.
Innovative and Emerging Therapies
- Photodynamic Therapy: This novel treatment uses a photosensitizing agent activated by light to produce reactive oxygen species that kill the amoebae. Photodynamic therapy shows promise for treating both trophozoites and cysts.
- Nanoparticle-Based Treatments: Researchers are working to create nanoparticles that can deliver antimicrobial agents directly to the site of infection, potentially increasing treatment efficacy while reducing side effects.
- Gene Therapy: Although still in the experimental stage, gene therapy aims to boost the host’s immune response or disrupt Acanthamoeba’s genetic machinery, offering a novel approach to treatment.
- Advanced Drug Delivery Systems: Innovations such as sustained-release drug implants or contact lenses embedded with antimicrobial agents are being investigated to provide continuous drug delivery and improve patient compliance.
Essential Preventive Measures
- Proper Contact Lens Hygiene: Always wash your hands before handling contact lenses, and only use sterile solutions to clean and store them. Avoid using tap water or home-made saline solutions.
- Avoid Water Exposure with Lenses: Do not swim, shower, or soak in hot tubs while wearing contact lenses. If water contact is unavoidable, use watertight swim goggles.
- Regular Lens Case Replacement: Replace contact lens cases every three months and clean them regularly with sterile solution rather than tap water.
- Do Not Reuse or Top Off Solution: Always use a fresh cleaning solution when storing lenses, and do not top off the old solution.
- Do Not Sleep With Contact Lenses: Unless specifically designed for overnight use, remove contact lenses before going to bed to reduce the risk of infection.
- Routine Eye Examinations: Regular visits to an eye care professional can help detect early signs of infection and ensure proper lens hygiene practices are followed.
- Address Eye Discomfort: If you experience persistent eye pain, redness, or vision changes while wearing contact lenses, seek medical attention right away.
- Educate Yourself and Others: Knowing about acanthamoeba keratitis and its risk factors can help prevent infections. Share information with other contact lens users to encourage safe practices.
Trusted Resources
Books
- “Contact Lens Complications” by Nathan Efron
- “Keratitis: Diagnosis and Treatment” by Helena M. Tabery
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski and Brad Bowling






