Introduction to Macular Pucker
A macular pucker, also known as epiretinal membrane (ERM), is an ocular condition in which a thin layer of fibrous tissue forms on the macula’s surface. The macula is the central part of the retina that provides the sharp, detailed vision required for activities such as reading and facial recognition. When this fibrous tissue contracts, it causes the macula to wrinkle or pucker, resulting in visual distortions.
Symptoms of a macular pucker include blurred vision, distorted central vision (where straight lines appear wavy or bent), and difficulty reading small print or performing tasks requiring fine visual detail. Although macular pucker can occur in one or both eyes, it is most common in people over the age of 50 and can be associated with diabetic retinopathy, retinal detachment, or inflammation inside the eye.
The exact cause of macular pucker is unknown, but it is thought to be due to changes in the vitreous gel that fills the eye. As we get older, the vitreous can shrink and pull away from the retina, potentially causing small tears or inflammation that leads to the formation of fibrous tissue on the macula. Understanding the nature of macular pucker is critical for appreciating progress in its treatment and management.
Standard Treatments for Macular Pucker
Traditional treatment for macular pucker focuses primarily on symptom management and, in severe cases, surgical removal of the epiretinal membrane to improve vision. The standard surgical procedure for macular pucker is vitrectomy.
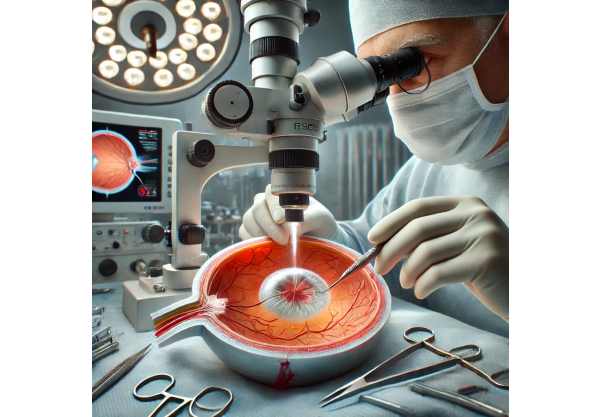
Vitrectomy
Vitrectomy is the primary surgical procedure for macular puckering. This procedure removes the vitreous gel from the eye, as well as the epiretinal membrane that causes the puckering. The surgery, which takes place under local or general anesthesia, involves making small incisions in the sclera (white part of the eye) in order to insert tiny instruments. These instruments include a light source, a cutting tool, and a suction device for removing vitreous and fibrous tissue.
Post-Surgical Results
While vitrectomy is generally effective at reducing or eliminating visual distortions and improving visual acuity, it does have some risks. Infection, retinal detachment, cataract formation, and changes in intraocular pressure are all possible complications. Recovery from vitrectomy can take weeks or months, and the final visual outcome depends on the severity of the macular pucker and the presence of other ocular conditions.
Observation and Nonsurgical Management
In cases where the macular pucker causes minor symptoms that do not interfere with daily activities, ophthalmologists may advise a watchful waiting approach. Regular monitoring, such as comprehensive eye exams, can help track any changes in the condition over time. Patients should report any worsening of symptoms, such as increased visual distortion or additional blurring of vision.
Low-Vision Aids
Low vision aids can help people with mild to moderate vision impairment due to macular pucker. Magnifying glasses, specialized reading lights, and electronic devices that improve visual contrast and magnification are examples of such aids. While these aids do not treat the underlying condition, they can improve quality of life by allowing people to perform daily tasks more efficiently.
Breakthrough Innovations in Macular Pucker Treatment
Medical technology advancements and a better understanding of ocular diseases have resulted in significant improvements in the treatment and management of macular puckers. These cutting-edge developments aim to improve treatment precision, safety, and efficacy, giving people with this condition new hope.
Advanced Vitrectomy Techniques
Modern advances in vitrectomy techniques have significantly improved the results of this surgical procedure. The introduction of micro-incision vitrectomy surgery (MIVS) transformed the field. MIVS uses smaller gauge instruments (23-, 25-, or 27-gauge) than traditional 20-gauge instruments. These smaller instruments enable minimally invasive procedures, resulting in less eye trauma, faster recovery times, and a lower risk of complications like infection and retinal detachment.
Enhanced Imaging Technologies
Advanced imaging technologies, such as optical coherence tomography (OCT), have significantly improved the diagnosis and treatment of macular pucker. OCT generates high-resolution cross-sectional images of the retina, allowing ophthalmologists to see the macular anatomy in detail. This technology allows for precise measurement of the thickness of the epiretinal membrane and its impact on the macula, which aids in surgical planning and post-operative monitoring.
Therapeutic Interventions
Emerging pharmacologic therapies may provide non-surgical options for macular pucker treatment. Researchers are investigating the use of anti-fibrotic agents to inhibit the formation and contraction of the epiretinal membrane. These agents target the fibrosis-related cellular mechanisms, with the goal of preventing or slowing the progression of macular pucker.
One promising pharmacologic approach is the use of enzyme-based treatments like ocriplasmin. Ocriplasmin is a recombinant enzyme that can dissolve proteins found in the vitreous gel and epiretinal membrane. Clinical trials have demonstrated that intravitreal injections of ocriplasmin can cause the vitreous to separate from the retina, potentially reducing the need for surgical intervention in some patients.
Genetic Therapy
Gene therapy represents an exciting new frontier in the treatment of a variety of ocular conditions, including macular pucker. This novel approach involves delivering specific genes into the retina to address the underlying causes of fibrosis and inflammation. Researchers hope to halt or reverse the progression of macular pucker by modifying gene expression at the molecular level.
Although gene therapy for macular pucker is still in its early stages, preliminary studies have yielded promising results. Researchers are investigating the ability of adeno-associated viral (AAV) vectors to deliver therapeutic genes to retinal cells. These vectors have proven safe and effective in preclinical models, paving the way for future clinical trials.
Stem Cell Therapy
Stem cell therapy has enormous potential for regenerating damaged retinal tissue and restoring vision in people with macular pucker. Stem cells possess the unique ability to differentiate into a variety of cell types, including retinal cells. Researchers are investigating the transplantation of stem cells into the retina in order to replace damaged or degenerated cells and promote tissue regeneration.
Recent advances in stem cell research have resulted in the creation of retinal organoids—miniature, three-dimensional retinal structures grown from stem cells. These organoids can mimic the organization and functionality of the human retina, making them a useful model for studying macular pucker and testing potential treatments. While stem cell therapy for macular pucker is still in its early stages, ongoing research shows promise for future clinical applications.
Artificial Intelligence, Machine Learning
The incorporation of artificial intelligence (AI) and machine learning (ML) into ophthalmology has provided new opportunities for diagnosing and treating macular pucker. AI algorithms can analyze large amounts of imaging data, such as OCT scans, to detect subtle changes in the retina that may indicate the beginning stages of macular pucker. This early detection can lead to timely intervention and better treatment outcomes.
Furthermore, artificial intelligence-powered tools can help ophthalmologists plan treatments and monitor patients after surgery. These tools, which analyze patient data and surgical outcomes, can provide personalized recommendations for optimizing surgical techniques and predicting visual recovery. The application of AI and ML in macular pucker management is a significant step toward precision medicine in ophthalmology.
Personalized Medicine
Personalized medicine seeks to tailor treatments to individual patients based on their distinct genetic, molecular, and clinical characteristics. In the case of macular pucker, personalized approaches can improve treatment efficacy while minimizing side effects. Ophthalmologists can identify patients who will benefit more from specific interventions by analyzing genetic markers and biomarkers associated with the condition.
For example, genetic testing can reveal variations in genes involved in fibrosis and inflammation, guiding the choice of targeted therapies. Furthermore, molecular profiling of the epiretinal membrane can provide insights into the cellular mechanisms causing macular pucker, allowing for the development of novel therapeutics that target the underlying pathology.
Minimally Invasive Surgical Instruments
The development of new surgical devices has advanced the field of macular pucker treatment. Innovations such as intraoperative OCT-guided surgery enable real-time retinal visualization during vitrectomy. This technology allows surgeons to precisely identify and remove the epiretinal membrane, lowering the risk of damaging the surrounding retinal tissue.
Furthermore, the use of robotic-assisted surgical systems has improved the accuracy and dexterity of vitrectomy procedures. These systems use surgeon-controlled robotic arms to provide enhanced stability and fine motor control. Robotic surgery can reduce the risk of human error while also improving surgical outcomes in macular pucker treatment.
Combination Therapies
Combination therapies, which employ multiple treatment modalities, are emerging as a promising strategy for managing macular pucker. For example, combining pharmacologic agents and advanced surgical techniques can improve treatment outcomes. Antifibrotic medications given before or after vitrectomy may lower the risk of recurrence and improve visual recovery.
Furthermore, integrating imaging technologies into surgical interventions enables more precise and targeted treatments. Combining OCT-guided surgery with enzyme-based therapies can improve epiretinal membrane removal while minimizing retinal trauma. The synergistic effects of combination therapies have a high potential for improving the efficacy and safety of macular pucker treatment.