Phacoanaphylactic endophthalmitis is a rare and severe type of intraocular inflammation that occurs when lens proteins are exposed to the immune system, usually as a result of trauma or surgical procedures like cataract extraction. When the lens capsule ruptures, lens proteins can leak into the eye, triggering a strong immune response. This response causes inflammation in the uveal tract, which includes the iris, ciliary body, and choroid, as well as damage to other ocular structures, potentially resulting in vision loss.
Phacoanaphylactic endophthalmitis causes symptoms such as pain, redness, blurred vision, photophobia, and floaters. The onset can range from days to weeks after the inciting event, and it is frequently accompanied by symptoms of severe intraocular inflammation such as hypopyon (pus in the anterior chamber), vitritis (inflammation of the vitreous body), and retinal detachment.
The diagnosis of phacoanaphylactic endophthalmitis is based on a thorough clinical examination that includes slit-lamp biomicroscopy, fundus examination, and imaging studies such as optical coherence tomography (OCT) and ultrasound. Laboratory tests, such as aqueous or vitreous sampling, can help identify inflammatory cells and rule out infectious causes of endophthalmitis. Early and accurate diagnosis is critical for initiating appropriate treatment and avoiding irreversible ocular damage.
Standard Treatments for Phacoanaphylactic Endophthalmitis
The management and treatment of phacoanaphylactic endophthalmitis focuses on reducing inflammation, preserving vision, and avoiding complications. Standard treatment methods usually include a combination of medical and surgical approaches tailored to the severity of the condition.
Corticosteroid Therapy: Because of their potent anti-inflammatory properties, corticosteroids are the most commonly used treatment for phacoanaphylactic endophthalmitis. They can be given topically, intraocularly, or systemically, depending on the severity of the inflammation. Prednisolone acetate, for example, is a common topical corticosteroid used to reduce anterior segment inflammation. In severe cases of inflammation, periocular or oral corticosteroids may be required to achieve adequate control.
Immunosuppressive Agents: Patients who do not respond well to corticosteroids or who require long-term treatment may benefit from immunosuppressive agents such as methotrexate, azathioprine, or cyclosporine. These medications help to regulate the immune response and reduce inflammation, lowering the risk of corticosteroid-related side effects.
Antibiotic Therapy: Although phacoanaphylactic endophthalmitis is primarily an inflammatory condition, secondary bacterial infection can develop. While waiting for culture results from aqueous or vitreous samples, empiric antibiotic therapy can be initiated. Broad-spectrum antibiotics, such as vancomycin and ceftazidime, are frequently used to treat a wide range of pathogens.
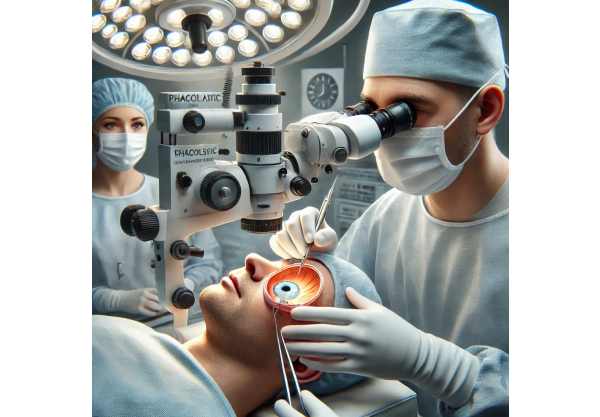
Surgical Intervention: Surgery is frequently required to treat complications of phacoanaphylactic endophthalmitis, such as persistent inflammation, secondary glaucoma, or retinal detachment. The most common surgical procedures are:
- Pars Plana Vitrectomy (PPV): PPV is the removal of vitreous gel and inflammatory debris from the eye. This procedure can help reduce intraocular inflammation, improve retinal visibility, and prevent future complications.
- Lens Extraction: If the lens is the primary cause of inflammation, lens extraction may be required. This procedure can be combined with vitrectomy to clear the visual axis and remove any remaining lens material.
- Glaucoma Surgery: Phacoanaphylactic endophthalmitis-related secondary glaucoma may necessitate surgical intervention to control intraocular pressure. Trabeculectomy and glaucoma drainage device implantation are two procedures that can help manage intraocular pressure while also protecting the optic nerve.
Postoperative Care: Following surgical intervention, meticulous postoperative care is required to ensure proper healing and avoid recurrent inflammation. This includes taking anti-inflammatory medications, closely monitoring intraocular pressure, and scheduling regular follow-up appointments to assess visual recovery and detect any signs of recurrence.
Phacoanaphylactic Endophthalmitis Treatment Innovations
Recent advances in medical research and technology have resulted in significant improvements to the treatment and management of phacoanaphylactic endophthalmitis. These cutting-edge approaches seek to improve therapeutic efficacy, shorten recovery times, and reduce the likelihood of complications. This article delves deeply into some of the most effective and groundbreaking treatments that have transformed the management of this condition.
Advanced Corticosteroid Delivery Systems
One of the most significant advances in the treatment of phacoanaphylactic endophthalmitis has been the development of advanced corticosteroid delivery systems. These innovations improve the efficacy of corticosteroid therapy while reducing systemic side effects.
Intravitreal Corticosteroid Implants: Intravitreal corticosteroid implants, such as the dexamethasone intravitreal implant (Ozurdex) and the fluocinolone acetonide implant (Retisert), deliver corticosteroids continuously into the vitreous cavity. These implants provide a long-lasting anti-inflammatory effect, reducing the need for repeated topical or systemic corticosteroid administration. They are especially useful for chronic or recurring inflammation.
Subconjunctival Corticosteroid Injections: Subconjunctival corticosteroid injections provide an alternative method of delivering high concentrations of medication directly to the site of inflammation. This method can produce rapid and long-lasting anti-inflammatory effects, improving outcomes in severe cases of phacoanaphylactic endophthalmitis.
Biological Therapies and Immunomodulators
Biologic therapies and immunomodulators are a promising frontier in the treatment of phacoanaphylactic endophthalmitis. These treatments target specific immune system components involved in the inflammatory response, providing more precise and effective control of inflammation.
TNF-α inhibitors: TNF-α inhibitors, including infliximab and adalimumab, have been effective in treating inflammatory ocular conditions. Biologic agents that inhibit TNF-α can reduce inflammation and improve outcomes in patients with phacoanaphylactic endophthalmitis. Clinical trials are underway to assess their safety and efficacy in this particular condition.
Interleukin inhibitors: Interleukin (IL) inhibitors, including tocilizumab (an IL-6 receptor antagonist) and anakinra (an IL-1 receptor antagonist), have been studied for their ability to modulate the immune response in inflammatory ocular diseases. These agents can aid in the reduction of pro-inflammatory cytokines, thereby controlling inflammation and preventing tissue damage in phacoanaphylactic endophthalmitis.
Calcineurin inhibitors: Calcineurin inhibitors, including cyclosporine and tacrolimus, are immunosuppressive agents that prevent T-cell activation. These medications can be used as an adjunctive therapy in patients with refractory inflammation, providing an additional mechanism to control the immune response and lowering the risk of corticosteroid dependency.
New Surgical Techniques and Technologies
Surgical techniques and technologies have advanced significantly, improving the outcomes of phacoanaphylactic endophthalmitis surgeries. These advancements increase precision, reduce surgical trauma, and shorten recovery times.
Microincision Vitrectomy Surgery (MIVS). MIVS involves the use of smaller gauge instruments (23-gauge, 25-gauge, or 27-gauge) during vitrectomy procedures. Smaller incisions reduce surgical trauma, promote faster healing, and lower the risk of complications. MIVS enables the precise removal of inflammatory debris and lens material, which improves the visual axis and reduces intraocular inflammation.
Femtosecond Laser-Assisted Surgery: Femtosecond laser technology offers precise and controlled tissue dissection, allowing surgeons to perform delicate maneuvers with high accuracy. Femtosecond lasers can be used in phacoanaphylactic endophthalmitis to perform anterior segment surgeries such as lens extraction or capsulotomy, improving surgical precision and lowering the risk of complications.
Endoscopic Vitrectomy: Endoscopic vitrectomy is a technique that uses an endoscope in conjunction with vitrectomy instruments to improve visualization and access to the posterior segment. This technique is especially useful when the anterior segment is opaque, limiting the view through traditional surgical microscopes. Endoscopic vitrectomy allows surgeons to perform precise dissection and removal of inflammatory material, resulting in better surgical outcomes for phacoanaphylactic endophthalmitis.
Gene Therapy and Molecular Treatments
Gene therapy and molecular treatments are emerging as promising options for treating phacoanaphylactic endophthalmitis. These novel approaches seek to address the underlying genetic and molecular mechanisms that drive the disease, with the potential for long-term and even curative results.
Gene Editing Technologies: Advances in gene editing technologies, such as CRISPR-Cas9, have created new opportunities for correcting genetic defects linked to phacoanaphylactic endophthalmitis. Gene editing, which precisely targets and modifies specific genes, has the potential to prevent abnormal immune responses and promote normal ocular function. While still in the experimental stage, gene editing shows great promise for future treatments.






