Hyphema is the accumulation of blood in the front (anterior) chamber of the eye, typically resulting from trauma, eye surgery, or, less commonly, underlying medical conditions. While often visible as a reddish pooling behind the cornea, hyphema can range from microscopic blood cells to a total filling of the chamber. The condition poses urgent risks to vision, including increased intraocular pressure and potential for long-term complications if not properly managed. This comprehensive guide explores everything you need to know—from established medical treatments to the latest surgical options and breakthrough innovations—empowering you to navigate hyphema care confidently and proactively.
Table of Contents
- Understanding Hyphema and Its Risk Factors
- Current Medical Therapies and Standard Management
- Surgical Intervention and Procedural Advancements
- Cutting-Edge Developments and Innovative Technologies
- Research Frontiers and Upcoming Clinical Trials
- Frequently Asked Questions
- Disclaimer
Understanding Hyphema and Its Risk Factors
Hyphema refers to the presence of blood in the anterior chamber of the eye, which lies between the cornea and the iris. While most cases result from blunt or penetrating trauma, spontaneous hyphemas can also occur, particularly in people with certain blood disorders or following eye surgery.
What Causes Hyphema?
- Trauma: Blunt injury (such as a sports impact or accident) is the leading cause, especially among children and young adults.
- Surgical Complications: Eye operations, including cataract or glaucoma surgery, can sometimes disrupt delicate blood vessels, leading to hyphema.
- Medical Conditions: Blood clotting disorders (e.g., hemophilia, sickle cell disease), tumors, or abnormal blood vessels may contribute.
- Medications: Blood thinners (anticoagulants) and some antiplatelet drugs can raise risk, especially when combined with trauma.
Types and Classifications
- Microhyphema: Only red blood cells, not visible to the naked eye.
- Grade I-IV Hyphema: Ranges from less than one-third to nearly total filling of the anterior chamber with blood.
Prevalence and Who Is at Risk
- Children, teenagers, and athletes are at highest risk, mainly due to accidental trauma.
- People with underlying clotting disorders or those taking blood-thinning medications face higher risk of spontaneous or severe hyphemas.
Complications and Why Prompt Care Matters
- Elevated Intraocular Pressure (IOP): Blood can block fluid drainage, leading to glaucoma and potential vision loss.
- Rebleeding: Can occur in the first few days, sometimes leading to worse outcomes.
- Corneal Blood Staining: Particularly dangerous in cases of large or prolonged hyphema.
- Synechiae and Permanent Vision Changes: Blood and inflammatory debris may cause adhesions or scarring within the eye.
Symptoms and Early Detection
- Visible blood pooling in the eye
- Blurred vision, light sensitivity, or eye pain
- Sometimes only detected by an eye exam, especially in microhyphema
Practical Prevention Tips
- Always wear protective eyewear during high-risk sports or work.
- Monitor for bleeding if you have a clotting disorder or are on anticoagulants.
- Keep regular follow-ups after any eye surgery.
Prompt diagnosis and risk assessment set the stage for effective management and vision preservation.
Current Medical Therapies and Standard Management
Managing hyphema centers on controlling intraocular pressure, minimizing the risk of rebleeding, and monitoring for complications. Non-surgical care is often effective for most cases, but strict adherence to therapy is essential.
Initial Assessment and Monitoring
- Bed Rest and Head Elevation: Patients are usually advised to rest with the head of the bed elevated 30–45 degrees to facilitate blood settling and clearance.
- Activity Restriction: Limit physical activity, avoid bending or lifting, and prevent situations that increase eye pressure.
- Eye Shield: Protective shields are used to prevent accidental trauma during recovery.
- Regular Eye Exams: Frequent monitoring for changes in vision, pressure, and rebleeding.
Medications for Hyphema
- Topical Steroids: Reduce inflammation and decrease risk of synechiae (scar tissue formation).
- Cycloplegic Drops: Paralyze the iris and ciliary muscle to ease pain and reduce risk of further bleeding.
- Antiglaucoma Medications: Beta-blockers, alpha agonists, or carbonic anhydrase inhibitors may be prescribed to keep intraocular pressure in a safe range.
- Antifibrinolytic Agents: In select cases, oral or topical agents like aminocaproic acid are used to stabilize blood clots and lower the chance of rebleeding.
Special Considerations
- Sickle Cell Patients: Special care is needed, as standard glaucoma medications like carbonic anhydrase inhibitors may worsen sickling. Close collaboration with hematology is essential.
- Children: Increased risk of complications, making close observation and tailored therapy critical.
Practical Self-Care Advice
- Never rub or touch the affected eye.
- Strictly follow all medication and follow-up instructions.
- Avoid aspirin, NSAIDs, or other medications that may thin blood (unless directed by your doctor).
Warning Signs Needing Immediate Attention
- Sudden increase in eye pain or vision loss
- Nausea and vomiting (may signal high eye pressure)
- New bleeding or blood level rising in the eye
Timely, consistent medical care and lifestyle adjustments play a key role in full recovery from hyphema.
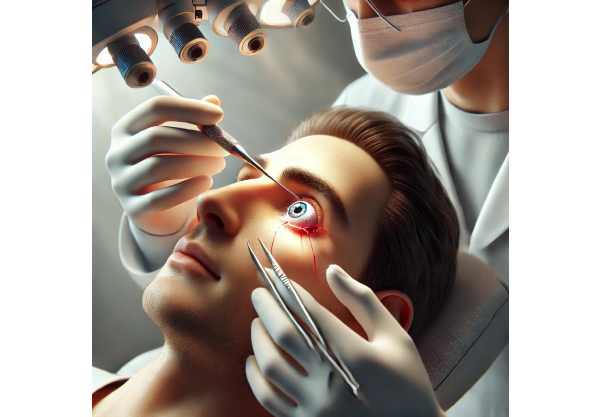
Surgical Intervention and Procedural Advancements
While most hyphemas resolve with conservative treatment, certain scenarios require surgical or minimally invasive intervention to protect vision and prevent permanent damage.
When Is Surgery Needed?
- Uncontrolled High Intraocular Pressure: If pressure remains high despite medications, especially in children or sickle cell patients.
- Large or Non-resolving Hyphema: Persistent blood (>50% of the chamber) for more than five days, or complete (eight-ball) hyphema.
- Corneal Blood Staining: When blood threatens to permanently stain the cornea.
- Rebleeding: Severe or recurrent bleeding with declining vision.
Surgical and Minimally Invasive Techniques
- Anterior Chamber Paracentesis:
A fine needle or cannula is used to drain blood directly from the anterior chamber. This can rapidly lower pressure and improve clarity. - Automated Anterior Chamber Washout:
Performed in the operating room using irrigation-aspiration systems, this technique clears blood and debris, reducing risk of complications. - Goniotomy and Trabeculotomy:
In some cases, these glaucoma surgeries may be combined to restore fluid outflow.
Post-Surgical Care
- Close Monitoring: Eye pressure, blood clearance, and corneal health are checked daily or every few days.
- Medication Adjustments: Continued steroids, cycloplegics, and IOP-lowering agents as needed.
- Infection Prevention: Strict aseptic technique during surgery and post-op antibiotic drops help prevent endophthalmitis (eye infection).
Recovery and Practical Post-Op Tips
- Use an eye shield at night and during naps.
- Attend all scheduled follow-up visits.
- Avoid strenuous activity or sports until cleared by your ophthalmologist.
- Watch for new pain, redness, or vision changes.
Prompt surgical intervention can be sight-saving for patients at risk of permanent hyphema complications.
Cutting-Edge Developments and Innovative Technologies
Ongoing advancements in the understanding and management of hyphema are improving both short-term safety and long-term visual outcomes.
Diagnostic and Imaging Innovations
- Anterior Segment Optical Coherence Tomography (OCT):
Non-invasive imaging for detailed assessment of blood location, volume, and resolution progress. - High-Resolution Ultrasound:
Allows visualization in eyes with dense blood obscuring internal details.
Novel Medical and Drug Therapies
- Sustained-Release Steroid Implants:
Under investigation for controlling inflammation with fewer daily drops. - Targeted Antifibrinolytic Therapy:
Improved formulations are being explored to reduce rebleed risk and speed recovery.
Minimally Invasive Surgical Devices
- Microcatheters and Precision Aspiration Tools:
Newer devices allow safer, less traumatic blood removal, reducing the risk of corneal injury and infection. - Biodegradable Implants:
Designed to temporarily maintain anterior chamber structure or slowly release medication during healing.
Digital Health and Remote Monitoring
- AI-Assisted Prognosis Tools:
Machine learning models can help predict which patients are at highest risk for complications, personalizing follow-up intensity. - Telemedicine Platforms:
Early triage and follow-up can now be managed via remote video consults in select cases.
Practical Innovation Tips
- Ask your eye doctor if digital imaging or AI risk assessment is available.
- Inquire about eligibility for new clinical trials if you have complex hyphema or are at high risk for complications.
By integrating these emerging approaches, eye care teams can deliver safer, more personalized care for hyphema patients.
Research Frontiers and Upcoming Clinical Trials
Exciting research is underway to further improve hyphema outcomes, speed healing, and reduce risks, especially for high-risk populations.
Current and Upcoming Studies
- Optimizing Antifibrinolytic Use:
Trials are comparing new topical, oral, and injectable agents for preventing rebleeds and enhancing safe recovery. - Genetic and Biomarker Research:
Studies seek to identify genetic or blood-based markers predicting which patients are most likely to have complications, enabling preventive interventions. - Regenerative Therapies:
Investigational treatments aim to support healing of damaged iris or corneal tissue after severe hyphema.
Focus on Special Populations
- Children and Athletes:
Research is refining guidelines for return to sports and school after hyphema. - Sickle Cell Disease:
New therapies aim to prevent vision loss and improve long-term prognosis.
The Future of Hyphema Care
- AI-powered triage systems in emergency departments.
- Universal access to point-of-care imaging for rapid hyphema grading.
- Integrated digital health platforms for personalized follow-up and medication reminders.
How to Stay Informed and Get Involved
- Subscribe to eye health research newsletters.
- Join patient advocacy groups for updates on clinical trials.
- Ask your eye doctor about participation in ongoing studies.
Research breakthroughs promise to make hyphema a more manageable—and less sight-threatening—diagnosis in the years ahead.
Frequently Asked Questions
What is hyphema and what causes it?
Hyphema is blood collecting in the front chamber of the eye, most often caused by trauma but also possible after surgery or due to blood disorders or medications affecting clotting.
What are the best treatments for hyphema?
Treatment involves resting with head elevation, eye shields, anti-inflammatory and pressure-lowering drops, and close monitoring. Surgery may be needed if blood doesn’t clear or eye pressure stays high.
Can hyphema cause permanent vision loss?
Yes, if not properly managed, hyphema can lead to glaucoma, corneal blood staining, or scarring, all of which can result in permanent vision problems.
How long does it take for hyphema to heal?
Most cases resolve within one to two weeks with proper care, but more severe or complicated hyphemas may take longer or require surgical treatment.
When is surgery needed for hyphema?
Surgery is considered when there’s high eye pressure unresponsive to medication, persistent large blood clots, or risk to the cornea or optic nerve.
How can I prevent hyphema or reduce my risk?
Wear protective eyewear during risky activities or sports, manage blood clotting conditions, and inform your doctor if you’re taking blood thinners.
What warning signs should prompt immediate medical attention?
Sudden vision loss, severe pain, increasing redness, or nausea with eye symptoms require prompt emergency evaluation.
Disclaimer
This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider regarding eye injuries, symptoms, or changes in vision.
If you found this guide helpful, please consider sharing it on Facebook, X (formerly Twitter), or your favorite social network. Your support helps us continue creating clear, practical eye health resources. Follow us for more tips and updates on vision care and safety!






