Lacrimal gland dislocation, though uncommon, can significantly impact ocular comfort and visual function. Characterized by the abnormal position or prolapse of the lacrimal gland, this condition may arise from trauma, aging, inflammation, or congenital factors. Patients often experience symptoms ranging from visible bulging in the upper eyelid to discomfort and excessive tearing. This guide explores the essential elements of diagnosis, provides an in-depth review of current and advanced treatment options, and offers practical insights for patients and clinicians navigating the evolving landscape of lacrimal gland dislocation management.
Table of Contents
- Condition Overview and Epidemiology
- Conventional and Pharmacological Therapies
- Surgical and Interventional Procedures
- Emerging Innovations and Advanced Technologies
- Clinical Trials and Future Directions
- Frequently Asked Questions
Condition Overview and Epidemiology
Lacrimal gland dislocation refers to the abnormal positioning of the lacrimal gland, most commonly presenting as gland prolapse or descent from its normal fossa in the upper outer eyelid. The lacrimal gland is responsible for producing the aqueous component of tears, essential for maintaining the health and function of the ocular surface.
Definition and Pathophysiology:
- The condition involves partial or complete displacement of the lacrimal gland from its bony fossa, often presenting as a palpable, sometimes visible, mass in the upper eyelid.
- Dislocation can disrupt tear flow and, in rare cases, compress adjacent orbital structures.
Causes and Risk Factors:
- Aging: Weakening of the orbital septum and supportive tissues is the most frequent underlying cause in older adults.
- Trauma: Blunt or penetrating injuries can disrupt normal gland positioning.
- Inflammation: Chronic inflammation (such as dacryoadenitis) may cause scarring or tissue laxity.
- Congenital: Rarely, gland malposition is present from birth.
- Surgical/iatrogenic: Previous eyelid or orbital surgery can weaken supportive tissues.
Prevalence:
- Precise epidemiological data are limited, but the condition is more prevalent in the elderly and those with prior eyelid trauma or surgery.
- No strong gender or ethnic predilection is documented.
Symptoms and Clinical Presentation:
- Bulge or fullness in the upper outer eyelid.
- Visible or palpable mass that may move with eyelid movement.
- Discomfort, aching, or mild pain, especially when looking upward.
- Excessive tearing (epiphora) or, less commonly, dry eye symptoms if tear flow is impaired.
- Rarely, diplopia (double vision) if the gland compresses ocular muscles.
Diagnosis:
- Clinical examination reveals an upper eyelid mass, often accentuated when the patient looks downward.
- Eversion of the eyelid may expose the gland tissue.
- Imaging (ultrasound, CT, or MRI) is valuable to rule out gland tumors or cysts, and to assess the extent of dislocation.
Practical Advice:
- Seek medical attention if you notice a new, painless swelling of the upper eyelid.
- Persistent discomfort, changes in vision, or rapid growth should prompt prompt evaluation.
Conventional and Pharmacological Therapies
Conservative management of lacrimal gland dislocation is often reserved for mild cases or individuals unfit for surgery. In selected scenarios, symptoms can be controlled without the need for operative intervention.
Non-Surgical Approaches:
- Observation: Asymptomatic or minimally symptomatic patients, especially older adults, may benefit from regular monitoring rather than immediate intervention.
- Lubricating eye drops: Prescribed to address mild irritation or dryness due to disrupted tear flow.
- Warm compresses: Can relieve mild discomfort if inflammation is present.
- Lifestyle adjustments: Advising gentle cleansing, avoidance of eye rubbing, and proper eyelid hygiene can prevent aggravation.
Pharmacological Treatment:
- Topical corticosteroids: Occasionally used for inflammatory swelling (dacryoadenitis) contributing to or exacerbating gland displacement.
- Oral anti-inflammatory medications: Prescribed when significant inflammation is identified.
- Antibiotics: If bacterial infection (e.g., secondary dacryoadenitis) is suspected, topical or systemic antibiotics may be indicated.
Treatment for Underlying Conditions:
- Systemic disease management: Autoimmune diseases such as sarcoidosis or Sjögren’s syndrome may contribute to gland inflammation and should be managed by a multidisciplinary team.
- Allergy management: Addressing allergic triggers may help reduce eyelid swelling and discomfort.
Limitations of Conservative Care:
- Non-surgical management does not reposition the gland; it is primarily for symptom control.
- Recurrence or worsening of prolapse is likely without surgical correction in moderate to severe cases.
Practical Tips:
- Keep a symptom diary to track changes and report new symptoms promptly.
- Use prescribed medications exactly as directed and consult your provider before discontinuing any treatment.
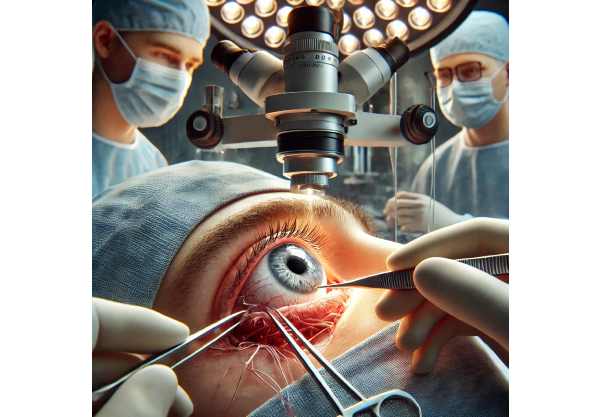
Surgical and Interventional Procedures
Surgery is the primary treatment for significant lacrimal gland dislocation, particularly when symptoms affect quality of life or when conservative management fails.
Lacrimal Gland Repositioning:
- The standard approach involves carefully dissecting and repositioning the gland into its normal anatomical fossa.
- The gland is anchored to the periosteum or orbital rim using non-absorbable sutures.
- Sometimes, supportive mesh or tissue grafts are used to reinforce the repair.
Orbital Septum Tightening (Blepharoplasty):
- For mild cases or those with coexistent eyelid laxity, tightening the orbital septum can help support the gland’s position.
- Blepharoplasty can also address cosmetic concerns.
Partial Gland Excision:
- In cases of severe prolapse or when gland tissue is nonviable (due to chronic inflammation or trauma), partial excision may be necessary.
- Care is taken to preserve as much gland tissue as possible to maintain tear function.
Management of Complications:
- Recurrence: Recurrent dislocation may require revision surgery, sometimes with alternative fixation techniques.
- Infection: Postoperative infections are rare but require prompt management with antibiotics.
- Scarring: Excessive scarring may impair eyelid mobility or gland function and occasionally necessitate further intervention.
Adjunctive Measures:
- Temporary tarsorrhaphy (partial eyelid closure) may be used to protect the gland and facilitate healing in select patients.
- Stent or tissue glue applications are under investigation for added support.
Postoperative Care:
- Cold compresses to minimize swelling and discomfort.
- Short-term topical or oral antibiotics and anti-inflammatory agents.
- Avoidance of strenuous activity, eye rubbing, or trauma to the area for several weeks post-surgery.
Practical Advice:
- Discuss anesthesia options, expected downtime, and postoperative appearance with your surgeon.
- Adhere closely to postoperative instructions for optimal outcomes.
- Keep all follow-up appointments to ensure proper healing and early recognition of complications.
Emerging Innovations and Advanced Technologies
The management of lacrimal gland dislocation is evolving, with modern techniques aiming to improve outcomes and minimize invasiveness.
Endoscopic and Minimally Invasive Surgery:
- New endoscopic approaches allow for gland repositioning with smaller incisions, less visible scarring, and faster recovery.
- High-resolution intraoperative imaging provides precise gland localization, reducing the risk of injury.
Absorbable Support Devices and Bioengineered Mesh:
- The use of bioabsorbable scaffolds or meshes for gland fixation is gaining popularity, offering support while gradually integrating into natural tissues.
Tissue Adhesives and Glues:
- Fibrin and synthetic tissue adhesives provide alternative or adjunctive fixation, minimizing the need for permanent sutures.
Computer-Assisted Surgical Planning:
- Preoperative 3D imaging enables tailored surgical plans, improving anatomical restoration and reducing operative time.
- AI algorithms can help predict risk of recurrence and recommend individualized management.
Robotic Surgery:
- Though still experimental, robotic platforms offer precision in delicate orbital procedures, with potential to enhance outcomes in complex cases.
Biologic Therapies and Regenerative Medicine:
- Early-stage research investigates stem cell therapy for gland repair in cases complicated by atrophy or loss of tissue function.
Patient-Centered Care Innovations:
- Mobile health apps and telemedicine enable remote monitoring, early detection of recurrence, and improved access to postoperative support.
- Patient-reported outcome tracking supports shared decision-making and long-term quality of life assessment.
Practical Tips:
- Ask about eligibility for less invasive surgical approaches or participation in clinical trials for innovative therapies.
- Consider digital tools for symptom monitoring and recovery tracking.
Clinical Trials and Future Directions
Ongoing research is advancing both surgical and non-surgical management options for lacrimal gland dislocation.
Current Research Focus:
- Prospective trials comparing endoscopic and traditional surgical outcomes.
- Evaluation of bioengineered and absorbable support materials for long-term efficacy and safety.
- Impact of regenerative medicine and biologic therapies on gland function recovery.
- Quality-of-life studies measuring functional, cosmetic, and psychosocial outcomes after various interventions.
Emerging Areas of Study:
- Predictive modeling using AI to personalize treatment plans and forecast recurrence risk.
- Development of advanced imaging modalities for earlier, more accurate diagnosis.
- Assessment of robotic-assisted orbital surgery for improved precision and safety.
- Innovations in postoperative monitoring, including wearable devices to detect gland displacement or eyelid changes.
Patient Participation and Advocacy:
- Patients with recurrent or complex dislocation may benefit from enrolling in clinical trials to access next-generation therapies.
- Collaboration with patient advocacy groups can offer support and up-to-date research news.
Future Directions:
- Focus on minimally invasive, scar-minimizing techniques and materials that promote natural tissue healing.
- Continued integration of digital health tools for remote follow-up and patient education.
Practical Advice:
- Stay informed about active clinical trials and emerging therapies.
- Discuss with your eye care provider whether novel approaches or research studies might benefit your individual condition.
- Engage with support communities to share experiences and gather resources for ongoing care.
Frequently Asked Questions
What is lacrimal gland dislocation and how is it identified?
Lacrimal gland dislocation is the abnormal displacement of the tear-producing gland in the upper eyelid, often seen as a visible or palpable mass. Diagnosis is made by clinical exam, eyelid eversion, and sometimes imaging.
What are the typical causes of lacrimal gland dislocation?
Common causes include age-related tissue weakening, trauma, previous eyelid or orbital surgery, and chronic inflammation or autoimmune disease.
Does lacrimal gland dislocation always need surgery?
Not always. Mild cases may only require observation and symptom management, but moderate to severe dislocation often benefits from surgical repositioning to restore function and comfort.
Is surgery for lacrimal gland dislocation safe?
Surgical repositioning is generally safe with a high success rate. Complications are rare and include infection, recurrence, and scarring, but can be minimized by experienced surgeons.
Are there less invasive options for correcting gland dislocation?
Yes. Endoscopic, minimally invasive, and absorbable fixation techniques are now available and often lead to less visible scarring and faster recovery than traditional surgery.
How long does recovery take after lacrimal gland surgery?
Most patients recover within two to four weeks, though swelling and mild discomfort may persist briefly. Strictly following postoperative instructions ensures the best outcome.
Disclaimer:
This guide is for educational purposes only and does not replace professional medical advice, diagnosis, or treatment. For concerns about lacrimal gland dislocation or related symptoms, please consult your eye care provider.
If you found this article useful, please share it on Facebook, X (formerly Twitter), or your favorite platform, and follow us on social media. Your support inspires us to keep delivering trusted, high-quality health content.






