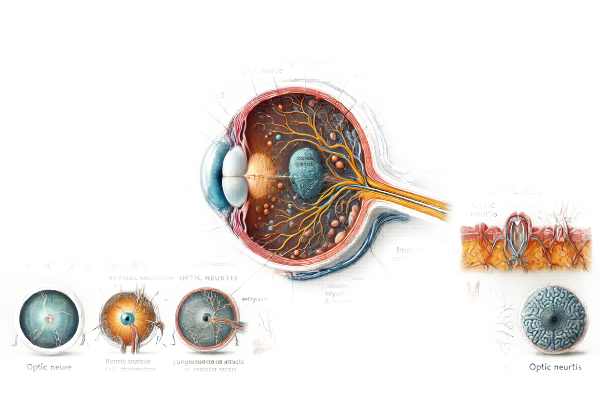
What is Optic Neuritis?
Optic neuritis is an inflammatory condition of the optic nerve, which transmits visual information from the eye to the brain. This inflammation can cause sudden vision loss, pain with eye movement, and other visual disturbances. Optic neuritis is frequently associated with multiple sclerosis (MS), but it can also occur as a result of other autoimmune disorders, infections, or as a single incident. Understanding optic neuritis is critical for early detection and treatment to avoid long-term visual impairment.
Detailed Investigation of Optic Neuritis
Anatomy and Pathophysiology
The optic nerve is a bundle of retinal ganglion cell axons and glial cells that connects the eye to the brain. It is critical for vision because it transmits visual information from the retina to the visual cortex. In optic neuritis, inflammation of the optic nerve interrupts this transmission, resulting in visual deficits.
The pathophysiology of optic neuritis includes an immune-mediated attack on the myelin sheath that surrounds the optic nerve fibers. This demyelination interferes with normal electrical conduction along the nerve, resulting in impaired vision. In some cases, inflammation can directly damage the nerve fibers.
Causes and Risk Factors
Multiple sclerosis is the most common associated condition for optic neuritis, but other factors can also cause it. Other causes are:
- Multiple Sclerosis (MS):
- Multiple sclerosis is an autoimmune disease in which the immune system attacks the central nervous system’s myelin sheath, which includes the optic nerve. Optic neuritis is frequently one of the initial symptoms of MS.
- **Neuromyelitis Optica (NMO)
- NMO, also known as Devic’s disease, is an autoimmune condition that primarily affects the optic nerves and spinal cord. It is similar to MS, but has distinct clinical and immunological characteristics.
- Infections:
Certain infections, such as herpes simplex virus and varicella-zoster virus, as well as bacterial infections like Lyme disease and syphilis, can cause optic neuritis. - Autoimmune disorders:
- Autoimmune diseases like lupus, sarcoidosis, and Behçet’s disease can cause optic neuritis as part of their systemic symptoms.
- Drug Reactions:
- Optical neuritis is a rare side effect of some medications and vaccines.
- Idiopathic:
- In many cases, no specific cause can be identified, so the condition is known as idiopathic optic neuritis.
Clinical Presentation
Symptoms of optic neuritis can vary, but typically include:
- Vision loss:
- Optic neuritis is characterized by sudden vision loss in one eye. The degree of vision loss can range from mild to severe, and it usually develops over hours to days. In some cases, vision in both eyes may be impaired, particularly in bilateral optic neuritis.
- Pain:
- Pain with eye movement is a common symptom that may precede vision loss. The pain is typically described as aching or discomfort behind the eyeball.
- Visual field defects:
- Patients may develop blind spots (scotomas), loss of color vision (dyschromatopsia), or peripheral vision loss.
- Afferent Pupillary Defect:
- A clinical examination may reveal an afferent pupillary defect (RAPD or Marcus Gunn pupil). This indicates a fault in the afferent visual pathway.
- The Uhthoff Phenomenon:
- The temporary worsening of symptoms caused by heat or exercise is known as Uhthoff’s phenomenon, and it can occur in patients with demyelinating diseases such as MS.
Pathophysiology
Immune cells that target the optic nerve’s myelin sheath primarily cause inflammation in optic neuritis. Demyelination disrupts the normal saltatory conduction of action potentials through nerve fibers, resulting in conduction block and impaired visual signal transmission.
In MS-related optic neuritis, the immune attack is part of a larger systemic process that affects other parts of the central nervous system. In NMO, the immune response focuses on aquaporin-4 water channels in the optic nerve and spinal cord.
Prognosis
The prognosis for optic neuritis varies according to the underlying cause. Many MS-related optic neuritis patients see significant improvement in their vision within a few weeks to months, though some permanent visual impairment may occur. Patients with specific risk factors, such as abnormal brain MRI findings, are more likely to develop MS following an initial episode of optic neuritis.
The prognosis in NMO can be more serious, with a higher risk of recurrent attacks and permanent disability. Early diagnosis and treatment are critical for managing these conditions and achieving better results.
Complications
- Chronic vision loss:
- While many patients regain most of their vision, some may suffer permanent vision loss due to irreversible damage to the optic nerve fibers.
- Recurring Episodes:
- Patients with MS or NMO may have recurrent episodes of optic neuritis, which causes cumulative damage and worsens visual outcomes.
- Associated neurological symptoms:
- Patients with systemic diseases like MS or NMO may develop additional neurological symptoms such as weakness, sensory disturbances, and coordination issues.
Differential Diagnosis
Several conditions can mimic optic neuritis, necessitating an accurate differential diagnosis:
- Anterior Ischemic Optic Neuropathy (AION):
- AION causes sudden vision loss due to a decrease in blood flow to the optic nerve. It usually affects older adults and is associated with cardiovascular risk factors.
- Leber’s Hereditary Optic Neuropathy (LHON):
- LHON is a genetic condition that results in progressive vision loss in young adults. It is distinguished by bilateral optic nerve atrophy and is diagnosed using genetic testing.
- Optical Nerve Compression:
- Tumors or other lesions compressing the optic nerve can result in vision loss and must be distinguished from optic neuritis using imaging studies.
- Toxic optic neuropathy:
- Certain toxins or medications can damage the optic nerve, causing vision loss. Identifying the offender is critical for management.
- Papilledema:
- Swelling of the optic disc caused by increased intracranial pressure can resemble optic neuritis, but it is distinguished by the presence of bilateral disc swelling and other signs of elevated intracranial pressure.
Methods to Diagnose Optic Neuritis
An accurate diagnosis of optic neuritis requires a combination of clinical evaluation, imaging studies, and laboratory tests to confirm the diagnosis and identify any underlying causes.
Clinical Evaluation
- Patient history:
- A detailed patient history is essential for determining the onset, duration, and progression of symptoms. Data on pain with eye movement, vision changes, and any systemic symptoms is gathered. A history of autoimmune diseases or recent infections can provide valuable diagnostic information.
- Ophthalmological Examination:
- Visual Acuity Testing: This determines the degree of visual impairment and is usually done with a Snellen chart or other standardized visual acuity tests.
- Fundoscopy: A direct examination of the optic disc with an ophthalmoscope can reveal swelling (papillitis) or atrophy. The optic disc may appear normal in retrobulbar optic neuritis, which occurs behind the globe.
- Pupil Reactions: Examining the pupil’s response to light can reveal an afferent pupillary defect (RAPD), which indicates severe optic nerve dysfunction.
Imaging Studies
- Magnetic Resonance Imaging(MRI):
- MRI is the preferred imaging modality for diagnosing optic neuritis and determining the risk of multiple sclerosis. It can produce detailed images of the optic nerves, brain, and spinal cord. Gadolinium-enhanced MRI can detect areas of active inflammation and demyelination.
- Brain MRI: Identifies white matter lesions suggestive of MS, which increases the likelihood of a subsequent MS diagnosis.
- Optical Coherence Tomography (OCT):
- OCT is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the retina and optic nerve head. It can measure the thickness of the retinal nerve fiber layer, which may be thinner in optic neuritis due to axonal loss.
Lab Tests
- Blood test:
- Blood tests can help detect underlying systemic conditions or infections that may cause optic neuritis. These tests may include a complete blood count (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and specific antibody tests for autoimmune diseases.
- Lumbral Puncture:
- Cerebrospinal fluid (CSF) analysis can detect oligoclonal bands, which are indicative of an inflammatory process within the central nervous system, as seen in MS. Elevated levels of specific antibodies can also indicate NMO.
- Visual Evoked Potentials (VEP):
- VEP testing assesses the electrical response of the visual cortex to visual stimulation. Delayed responses may indicate optic nerve demyelination, which supports the diagnosis of optic neuritis.
Effective Treatments for Optic Neuritis
Standard Treatment Options:
- Corticosteroids:
- Corticosteroids are the primary treatment for optic neuritis, particularly in cases associated with multiple sclerosis (MS). High-dose intravenous methylprednisolone is usually given for 3-5 days, followed by an oral corticosteroid taper. This regimen can speed up vision recovery, but it has no significant impact on long-term visual outcomes. Corticosteroids help to reduce inflammation and swelling in the optic nerve.
- Plasma Exchange Therapy:*
- If corticosteroids do not work for patients, plasma exchange (plasmapheresis) may be an option. This treatment entails removing and replacing plasma in the blood to eliminate antibodies and other inflammatory substances. It has been shown to be effective in severe cases of optic neuritis, particularly those involving neuromyelitis optica (NMO).
- Immunomodulatory Treatment:
- Patients with recurrent optic neuritis or MS may benefit from long-term immunomodulatory therapy to prevent future attacks. Disease-modifying therapies (DMTs) for MS, including interferon-beta, glatiramer acetate, and newer oral or infusion medications, can help reduce the frequency and severity of relapses.
Innovative and Emerging Therapies
- Anti-CD20 monoclonal antibodies:
- Rituximab and ocrelizumab are anti-CD20 monoclonal antibodies that deplete B-cells, which play a role in the inflammatory process of MS and NMO. These therapies have shown promise in reducing relapses and improving outcomes for patients suffering from these conditions.
- Interleukin-6 (IL-6) inhibitors:
- Tocilizumab, an IL-6 inhibitor, has demonstrated efficacy in treating NMO by targeting the disease’s inflammatory pathways. Clinical trials are currently underway to assess its efficacy in preventing relapses and improving vision in patients with optic neuritis associated with NMO.
- Neuroprotective Agents:*
- Researchers are working to identify neuroprotective agents that can shield optic nerve fibers from damage during inflammation. Citicoline and brimonidine are two drugs being investigated for their ability to improve neural survival and function.
- Stem Cell Treatment:
- Stem cell therapy is a developing field that has the potential to regenerate damaged optic nerve fibers and restore vision. Although still in the experimental stage, stem cell treatments show promise for the future treatment of optic neuritis and other neurodegenerative diseases.
- Remyelination Therapy:
- Researchers are working to develop therapies that promote remyelination, the process of repairing damaged myelin sheaths around nerve fibers. These treatments seek to restore normal nerve function and improve visual outcomes in patients suffering from demyelinating diseases such as MS.
Supportive Care
- Visual rehabilitation:
- Patients with severe vision loss may benefit from visual rehabilitation services, such as low vision aids, orientation and mobility training, and adaptive techniques, to improve their quality of life.
- Psychological support:
- Living with a chronic condition, such as optic neuritis, can be challenging. Psychological support and counseling can help with emotional and mental health issues, including stress management strategies and overall well-being.
Monitoring and Follow-up
Regular follow-up with an ophthalmologist and neurologist is required to monitor the condition, assess treatment efficacy, and manage any new complications. Periodic visual acuity tests, visual field assessments, and imaging studies are essential for monitoring changes and adjusting treatment plans as necessary.
Effective Ways to Improve and Prevent Optic Neuritis
- Regular Eye Examination:
- Schedule regular eye exams to check for vision changes and early signs of optic neuritis. Early detection enables timely intervention and improved management.
- Awareness of symptoms:
- Be aware of any changes in vision, such as blurring, pain with eye movement, or loss of color vision. Report these symptoms to an eye care professional right away.
- Managing Systemic Conditions:
- Manage systemic conditions like autoimmune diseases and infections that can cause optic neuritis. Proper management of these conditions can reduce the likelihood of developing optic neuritis.
- A Healthy Lifestyle:
- Eat a balanced diet high in antioxidants and nutrients that promote eye health. Regular exercise and avoiding smoking can also help with overall ocular health.
- Avoid Toxicants:
- Avoid toxins and medications that are known to cause optic neuropathy. Discuss any concerns with your healthcare provider, and make sure that any medications you’re taking are safe for your vision.
- Managing Stress:
- Chronic stress can worsen autoimmune conditions. Maintain your overall health by using stress management techniques like mindfulness, yoga, or meditation.
- Genetic counseling:
- For people who have a family history of autoimmune conditions or optic neuropathy, genetic counseling can help them understand their risk of developing optic neuritis and make better family planning decisions.
- Treatment Plans:
- Follow the treatment plans and follow-up schedules recommended by your healthcare provider. Consistent monitoring and adherence to treatment can halt the progression of complications.
- Engage in Support Networks:
- Join support groups or online communities for people who have optic neuritis or other similar conditions. Sharing experiences and strategies can offer both emotional support and practical advice.
Trusted Resources
Books
- “Clinical Neuro-Ophthalmology: A Practical Guide” by Ambar Chakravarty
- “Optic Neuritis and Multiple Sclerosis: An Evidence-Based Guide” by Andrew G. Lee and Michael J. Kupersmith
- “Neuro-Ophthalmology Illustrated” by Valérie Biousse and Nancy J. Newman






