A Fresh Perspective on Corneal Remodeling: A Comprehensive Overview of CAIRS
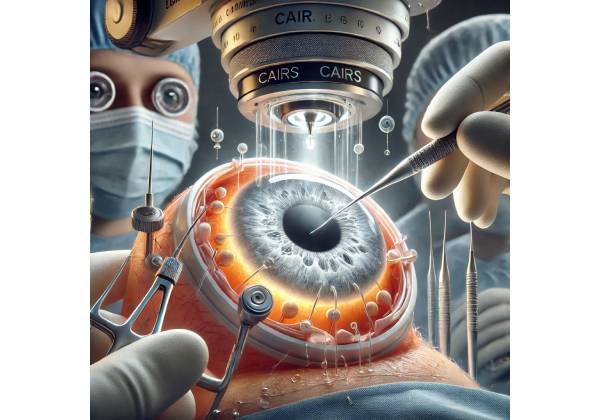
Keratoconus, a progressive thinning and bulging of the cornea, has long been a challenge to patients and eye care providers due to its impact on vision and quality of life. For many, conventional treatments—like rigid contact lenses, corneal cross-linking (CXL), or intrastromal corneal ring segments (ICRS) made from synthetic materials—can yield positive results. However, not all patients respond optimally, and some experience discomfort or suboptimal reshaping. Against this backdrop, Allogenic Intrastromal Ring Segments (CAIRS) stand out as an innovative solution that harnesses biological tissue—donor corneal rings—to support and stabilize the keratoconic cornea.
CAIRS merges the benefits of ring-segment implantation with the advantages of biologically compatible grafts. Donor corneal segments, shaped appropriately, fit into channels in the patient’s cornea to reinforce and restore a more normal contour. Early reports highlight improved corneal topography, enhanced visual acuity, and reduced higher-order aberrations (HOAs). This article explores how CAIRS works, what sets it apart from existing therapies, and why it may be a breakthrough for managing moderate-to-advanced keratoconus in patients not fully served by traditional options.
The concept of using donor tissue in ring-segment form for keratoconus correction is relatively new in the global ophthalmology arena. Yet the consistent improvement in corneal stability and the decreased foreign-body reaction have attracted keen interest. If validated by further research, CAIRS might redefine how eye care professionals approach keratoconus—offering an option that’s less invasive than a transplant but potentially more biologically integrated and comfortable than synthetic rings alone.
The Underpinnings of Keratoconus: Grasping the Condition’s Progression and Impact
To appreciate the significance of CAIRS, one must first understand the nature of keratoconus (KC) itself. The cornea, normally a dome-shaped transparent tissue, becomes progressively thinner and protrudes in a cone-like shape in keratoconus. This distortion leads to myopia, irregular astigmatism, and often significant visual aberrations that can’t be fully corrected with soft lenses or glasses.
Key Features of Keratoconus
- Onset and Risk Factors: Keratoconus usually emerges in the teenage or early adult years. While the exact cause remains multifactorial, genetic predispositions, environmental triggers (like eye rubbing), and certain conditions (e.g., Down syndrome) can increase susceptibility.
- Progressive Changes in Topography: Early KC may show subtle changes on corneal topography—like inferior steepening. As the disease advances, the cone shape becomes more pronounced, severely compromising vision.
- Symptoms and Functional Limitations: Patients often struggle with glare, halos, double vision (monocular diplopia), and poor night vision. Keratoconus can cause emotional distress, hamper performance at work or school, and lead to dependence on specialized contact lenses.
- Stages of Severity: Ophthalmologists grade KC severity (mild, moderate, advanced) based on keratometry values, corneal thickness, and scarring presence. Late-stage disease might require a corneal transplant if scarring or extreme thinning precludes other measures.
Typical management includes rigid gas-permeable or scleral lenses for better optics, collagen cross-linking to stiffen corneal tissue, and in some cases, synthetic ICRS to flatten or regularize the cone. Although many patients benefit, some require repeated interventions or eventually corneal transplantation. CAIRS emerges in this landscape as a potential game-changer, offering an allogenic ring-segment approach that merges optical correction, mechanical support, and biological integration.
Why Conventional Options May Fall Short
- Contact Lens Limitations: While specialized lenses can restore acceptable vision, they do not slow or reverse corneal deformation. Moreover, lens wear can be uncomfortable for severe cones, or might fail altogether if corneal shape changes significantly.
- Cross-Linking (CXL) Plateaus: Though highly effective at halting progression, CXL has limitations for extremely thin corneas and may not produce immediate topographic normalization. Some advanced keratoconic eyes see only partial flattening.
- Synthetic ICRS Challenges: Made from PMMA or similar materials, synthetic ring segments can reduce the cone but might cause local irritation, partial extrusion, or limited improvement in HOAs. Non-biological materials also carry a risk of vascularization or scarring in certain patients.
The impetus behind CAIRS is to deliver ring-segment benefits while leveraging human-derived tissue for better integration, potentially fewer complications, and improved corneal biomechanics.
How CAIRS Works: Dissecting the Mechanism Behind Allogenic Corneal Ring Segments
CAIRS’s premise is straightforward yet profound: harness donor corneal material to create intrastromal ring segments that mimic the function of synthetic rings, but with enhanced compatibility. This synergy of shape correction and biological integration sets CAIRS apart.
Allogenic Donor Tissue as the Foundation
Donor corneas, often surplus tissue from an eye bank unsuited for full-thickness transplant or advanced lamellar keratoplasty, are processed into arcs or ring segments. Surgeons carefully size and shape these arcs to fit corneal thickness and curvature data from the keratoconic patient. Because the segments are made from corneal collagen, they’re more likely to integrate seamlessly into the recipient’s stroma over time, reducing the risk of foreign body reactions that can occur with synthetic implants.
Re-establishing Structural Support
When placed in intracorneal channels (created via femtosecond laser or manual dissection), the segments exert a mild flattening effect on the steepest corneal areas. Much like synthetic ring segments, CAIRS can alter corneal curvature, regularizing the optical surface. The result: improved topography, potentially leading to better uncorrected or spectacle-corrected visual acuity. But unlike synthetic materials, the biologic ring fosters a continuum of corneal tissue, effectively acting as an internal buttress that might hamper further progression.
Biomechanical and Healing Advantages
- Tissue Incorporation: Over time, the host stroma can bond with or partially encapsulate the donor segment, forming a stable interface. Minimal micro-movements or friction can reduce the risk of migration or extrusion.
- Reduced Immunogenic Profile: Because corneal tissue is avascular, the immunogenic threat is relatively low. Thorough decellularization or partial processing of the donor tissue further lowers rejection risk, akin to processes used in lamellar grafts.
- Potential for Future Adjustments: If adjustments are required—like removing or repositioning segments—CAIRS can be manipulated similarly to synthetic ICRS, though with added caution due to its biological nature.
Ultimately, CAIRS attempts to rectify the underlying geometry of the keratoconic cornea. By smoothing irregularities, the treatment alleviates the cornea’s dependence on special lenses, complements cross-linking if needed, and possibly stalls keratoconus progression. Patients can expect greater optical quality, though the magnitude of improvement varies with disease stage, surgical precision, and healing patterns.
Surgical Implementation: Protocols and Best Practices for CAIRS
Adopting CAIRS in routine practice demands refined surgical skills, thorough preoperative planning, and familiarity with keratoconus staging. The following outlines the typical steps and considerations:
Patient Evaluation and Preoperative Measures
- Corneal Mapping and Pachymetry: High-resolution corneal tomography and OCT imaging are essential to identify the cone’s location, measure corneal thickness, and determine ring-segment arc length. Surgeons also look for scarring or other pathologies that might hamper ring placement.
- Keratoconus Severity Assessment: Mild to moderate keratoconus with enough thickness to accommodate ring channels often yields optimal outcomes. Extremely advanced cones or near-rupture corneas might require more definitive measures like a corneal transplant.
- Donor Tissue Preparation: Eye bank corneas that do not meet standards for full-thickness transplantation can be used. Tissue is shaped into arcs that match the diameter and thickness needed. Some centers use specialized femtosecond laser–based corneal segment creation. Standard decellularization or partial dehydration steps reduce antigenicity.
Surgical Steps
- Channel Creation: Using a femtosecond laser or a mechanical ring-segment dissector, the surgeon creates intrastromal tunnels at the desired corneal depth—generally around 70–80% of the corneal thickness. Precision is crucial to avoid perforation or asymmetrical channel depth.
- Donor Segment Insertion: The allogenic segment is inserted through the channel opening using specialized forceps or an injector. Surgeons gently slide the arc into position, ensuring it adheres to the planned orientation (often determined by topographic markers). Some protocols use one continuous ring, while others opt for two separate segments spaced around the cone.
- Final Verification: Intraoperative optical coherence tomography or topography can confirm correct placement. The surgeon checks for tension, any microfolds, or distortion. A small suture or corneal glue might close the entry site if needed.
- Postoperative Regimen: Typically includes topical antibiotics and steroids to curtail inflammation and reduce the risk of infection or immunological reaction. Patients follow up closely in the first weeks, with repeated imaging to track ring integration.
Combined or Sequential Cross-Linking
For younger patients or those with documented progression, some surgeons couple CAIRS with corneal cross-linking to enhance the stability of the cornea. Either done sequentially (e.g., ring insertion first, cross-linking weeks later) or simultaneously (though more technically complex), this synergy might yield a more robust outcome—mechanical support from CAIRS plus biochemical stiffening from CXL.
Gauging Efficacy and Mitigating Risks: The Performance and Safety of CAIRS
Though still emerging, CAIRS demonstrates promising outcomes in flattening the cone, improving visual acuity, and maintaining corneal integrity. However, as with any surgical procedure, complications must be acknowledged and monitored.
Measurable Visual and Topographic Gains
Patients frequently exhibit enhanced corneal regularity post-CAIRS, which translates into:
- Reduced Topographic Astigmatism: Notable flattening in the steep meridians, lowering diopters of irregular astigmatism.
- Improved Best-Corrected Visual Acuity (BCVA): Some individuals can shift from complicated lens requirements to simpler corrective options. In certain cases, BCVA improvements range from 1–2 lines, with outliers achieving more dramatic gains.
- Lower High-Order Aberrations (HOAs): Haloes, glare, and double images—commonly associated with the distorted shape of keratoconus—can lessen as the corneal surface normalizes.
Potential Complications to Monitor
- Infection: Although allogenic tissue is typically decellularized or rigorously tested, any foreign material raises a small infection risk. Surgeons adopt stringent sterile protocols and prophylactic antibiotics.
- Segment Dislocation or Rotation: If channels are too shallow or if the arc is incorrectly sized, the ring might shift. This is generally less frequent with proper technique and planning.
- Immunologic Reactions: Rare but possible. Mild interface haze or local inflammation can happen if the host recognizes the graft as foreign. Thorough decellularization and partial cross-linking of the segment can diminish this risk.
- Corneal Thinning or Perforation: In advanced cones with extremely thin corneas, the risk of inadvertent perforation or stress on the tissue is higher.
Fortunately, serious complications remain uncommon when CAIRS is performed by seasoned refractive surgeons adhering to meticulous protocols. Short-term results are promising, and mid-term follow-ups show stable ring segments and no major signs of rejection in most published case series. Still, extended longitudinal studies will clarify long-term survivability and maintain a track record of safety.
Clinical Research Insights: Evidence Backing CAIRS as a Keratoconus Solution
Although the concept of using donor corneal ring segments is relatively new, multiple studies worldwide have begun documenting outcomes, offering a growing body of data to inform both patients and ophthalmologists.
Key Published Studies
- Small Prospective Trials: Early prospective trials, each enrolling 20–30 keratoconus patients, indicated a mean decrease in Kmax (the steepest keratometric reading) by 2–4 diopters and an improvement in corrected distance visual acuity (CDVA) by 1–2 lines. No cases reported frank ring extrusion or severe inflammatory responses over 6–12 months of follow-up.
- Comparative Observational Reports: A handful of retrospective reviews compare CAIRS to standard synthetic ICRS in matched groups of keratoconus eyes. CAIRS cohorts showed slightly less corneal microfolds, suggesting a more harmonious integration. Subjective comfort and post-op dryness scores were similar or slightly better with CAIRS.
- Cross-Linking Combo Protocols: One pilot study investigating concurrent or staged cross-linking with CAIRS found that combining treatments might yield a more stable flattening effect, though a larger sample is required to confirm synergy. Preliminary results pointed to fewer re-treatments versus cross-linking alone.
International Adoption and Ongoing Trials
Countries like India, where corneal donation programs are robust, have seen earlier large-scale usage of CAIRS. Leading corneal centers in Europe and parts of Latin America are also trialing the approach. Meanwhile, multiple major academic institutions are set to launch longer-term, randomized investigations. Researchers plan to track not just visual changes but also rate of disease progression, ring stability, and potential immunological events over 2–5 years.
Patients often attest to stable vision improvements and fewer limitations in everyday tasks, reinforcing the concept that CAIRS can deliver functional gains. The evidence base, albeit still evolving, consistently underscores CAIRS’s potential as an effective, safe, and possibly more natural alternative to synthetic ring segments.
Cost and Accessibility: Navigating CAIRS in the Global Landscape
As with any procedure reliant on donor tissue and specialized surgical techniques, CAIRS can pose questions around cost, coverage, and availability. The expense typically includes the price of the ring segments (often proportionate to donor tissue processing fees), surgical fees, and facility charges for advanced equipment like femtosecond lasers.
Typical Pricing Structures
- Ring Segment Procurement Costs: Eye banks or corneal tissue processors may charge anywhere from a few hundred to over a thousand US dollars for prepared ring segments, depending on the region and the complexity of sizing/sterilization.
- Surgical Facility Fees: Clinics invest in femtosecond laser technology and specialized surgical instruments. Per-procedure overhead can add another substantial sum.
- Professional Fees: The surgeon’s expertise in performing intrastromal ring segment implantation plus patient follow-up visits factors into total expense.
Collectively, the final cost for CAIRS may range from \$2,000 to \$4,000 (or the equivalent) per eye in many locales, though wide variations exist. This figure can be higher if combined with cross-linking or if additional complexities arise.
Insurance and Reimbursement
In certain countries or under certain policies, partial coverage may be possible, especially if keratoconus severely impairs vision and other treatments have failed. However, CAIRS remains novel, so universal coverage is not guaranteed. Patients often need to secure prior authorization or pay out-of-pocket if deemed an “emerging” technology. Over time, as more clinical data emerges, some national health systems or private insurers may reconsider their coverage stance.
Eye Bank and Donor Tissue Availability
A robust eye bank infrastructure is critical. Regions with fewer donors or underdeveloped corneal donation systems may see limited CAIRS availability. Nonetheless, global eye banks frequently discard surplus corneal tissue deemed unsuitable for full-thickness keratoplasty but perfectly viable for ring-segment preparation. This synergy could help reduce waste and bolster the supply of ring segments. Partnerships between cornea specialists and eye banks are essential to sustain this therapy, ensure consistent quality, and keep costs within reach.
For keratoconus patients, exploring CAIRS requires candid discussions about the logistical and financial aspects. If coverage is minimal, clinics may offer payment plans or philanthropic channels to offset costs for low-income individuals. As acceptance grows and more donors contribute corneal tissue, increased supply may gradually lower the final expense, broadening access to this promising solution.
Disclaimer: This article is for educational purposes only and not a substitute for professional medical advice. Always consult a qualified healthcare provider regarding any medical condition or treatment.










