The alveoli are the microscopic, balloon-like air sacs within the lungs that serve as the critical interface for gas exchange. They are essential for breathing, supplying oxygen to the bloodstream and removing carbon dioxide from the body. Their specialized structure, including delicate walls and an extensive capillary network, enables efficient diffusion of gases, while surfactant production ensures they remain open during respiration. Understanding alveolar anatomy, physiology, and pathology is vital for diagnosing and managing a wide range of respiratory conditions. This guide offers an in-depth exploration of alveolar structure, function, disorders, diagnostic methods, treatment options, and practical tips for maintaining optimal lung health.
Table of Contents
- In-Depth Alveolar Architecture
- Essential Alveolar Roles
- Alveolar Health Challenges
- Comprehensive Diagnostic Methods
- Advanced Treatment Modalities
- Nutritional & Supplementary Interventions
- Strategies for Optimal Alveolar Function
- Reputable Resources for Respiratory Health
- Frequently Asked Questions
In-Depth Alveolar Architecture
The alveoli form the fundamental units of the lung’s gas exchange system. Their intricate design is a marvel of biological engineering, optimized to maximize oxygen uptake and carbon dioxide elimination. In this section, we delve into the microscopic structure and organization of alveoli, exploring every detail that contributes to their critical function.
Unique Morphology and Dimensional Characteristics
Alveoli are minuscule, balloon-like sacs typically measuring between 200 and 300 micrometers in diameter. They are organized in clusters that resemble bunches of grapes, forming a vast network within the lung tissue. This expansive surface area is crucial for efficient gas exchange, as it allows for close contact between inhaled air and the blood. The variation in their size and the dense packing of alveoli ensure that even a slight alteration in lung volume can have a significant impact on oxygenation.
- Balloon-Like Structures:
The spherical shape of alveoli minimizes the distance that gases must diffuse, thereby speeding up the exchange process. - Surface Area Optimization:
The aggregated, grape-like configuration maximizes the available surface area for oxygen and carbon dioxide diffusion, which is critical during both rest and strenuous activities.
Alveolar Walls and Cellular Composition
At the core of alveolar functionality is the remarkably thin barrier formed by alveolar walls. These walls are composed primarily of a single layer of epithelial cells known as type I alveolar cells or pneumocytes. Their extreme thinness—typically less than one micrometer—facilitates rapid diffusion of gases across the membrane.
- Type I Pneumocytes:
These cells cover approximately 95% of the alveolar surface and are pivotal in gas exchange due to their minimal thickness. - Type II Pneumocytes:
Scattered among the type I cells, type II pneumocytes are responsible for the synthesis and secretion of surfactant—a lipid-protein complex essential for reducing surface tension within the alveoli. Their role is not only supportive in nature but also regenerative, as they can differentiate into type I cells in response to injury.
Interalveolar Septa and Structural Support
The alveoli are separated by thin walls called interalveolar septa. These septa contain elastic fibers and a minimal amount of connective tissue that confers both stability and elasticity. This balance is critical for maintaining the shape and integrity of the alveoli during the cyclic process of inhalation and exhalation.
- Elastic Fibers:
The presence of elastic fibers in the septa is fundamental to lung recoil, aiding in the expulsion of air during exhalation. - Capillary Integration:
Embedded within these septa is an extensive network of pulmonary capillaries. The close juxtaposition of the capillary endothelium with the alveolar epithelium forms the respiratory membrane, the thin barrier across which gas exchange occurs.
The Alveolar Capillary Network
Each alveolus is enveloped by a dense web of capillaries. These capillaries are vital for transporting oxygen to body tissues and carrying carbon dioxide back to the lungs for exhalation. The capillary network is characterized by its low-pressure, high-flow system, which is optimized for efficient gas exchange.
- Respiratory Membrane:
This is the interface where oxygen and carbon dioxide diffuse between the alveolar air and the bloodstream. It is composed of the alveolar epithelium, the fused basement membranes of the alveolar and capillary walls, and the capillary endothelium. - Blood Flow Dynamics:
The pulmonary circulation is uniquely adapted to maintain a constant, low-pressure flow that minimizes damage to the delicate alveolar structures while ensuring that oxygenated blood is efficiently delivered to the heart.
Summary of Structural Insights
Understanding the detailed architecture of the alveoli is critical for appreciating how these microscopic structures support overall respiratory efficiency. Their unique design—from the delicate, single-layered epithelial cells to the robust capillary network and supportive interalveolar septa—ensures that gas exchange occurs with minimal resistance and maximal efficiency. This intricate structural arrangement is a testament to the evolutionary optimization of the respiratory system.
Essential Alveolar Roles
The alveoli are not only structural units; they are the epicenters of pulmonary function. In this section, we explore the multifaceted roles that the alveoli play in respiration and overall metabolic regulation. Their contributions extend far beyond simple gas exchange, influencing systemic physiology in profound ways.
The Dynamics of Gas Exchange
At the heart of alveolar function lies the process of gas exchange. During inhalation, fresh air rich in oxygen fills the alveoli. Due to the minimal diffusion distance across the thin alveolar walls, oxygen rapidly diffuses into the capillary blood, where it binds to hemoglobin in red blood cells. Conversely, carbon dioxide, a metabolic waste product, diffuses from the blood into the alveoli to be exhaled.
- Oxygen Diffusion:
The high concentration gradient between alveolar air and deoxygenated blood drives the diffusion of oxygen, ensuring that each breath replenishes the body’s oxygen supply. - Carbon Dioxide Elimination:
The removal of carbon dioxide is equally critical. By maintaining a low concentration of this gas in the alveoli, the body prevents the buildup of carbonic acid, which can lead to respiratory acidosis.
Surfactant Production and Its Impact
Surfactant, produced by type II alveolar cells, plays a vital role in maintaining alveolar stability. This complex mixture of lipids and proteins reduces surface tension, preventing the collapse of alveoli during exhalation and ensuring that they reopen easily during inhalation.
- Reduction of Surface Tension:
By lowering the adhesive forces between water molecules, surfactant allows alveoli to remain inflated even at low lung volumes. - Uniform Ventilation:
Surfactant helps stabilize alveoli of varying sizes, promoting even distribution of air throughout the lungs and optimizing gas exchange across the entire respiratory surface.
The Blood-Air Barrier: A Delicate Interface
The respiratory membrane, also known as the blood-air barrier, is where the magic of gas exchange happens. This barrier is remarkably thin—often only 0.5 micrometers thick—allowing for rapid diffusion of gases while also serving as a protective shield against harmful particles and pathogens.
- Selective Permeability:
Despite its thinness, the blood-air barrier is highly selective, permitting the passage of gases while preventing the entry of larger molecules and infectious agents. - Structural Integrity:
The close apposition of the alveolar epithelium and capillary endothelium, reinforced by fused basement membranes, ensures that the barrier is both efficient and resilient.
Ventilation-Perfusion Coupling
Efficient gas exchange in the lungs depends on the precise matching of ventilation (airflow) and perfusion (blood flow) in the alveoli. This balance is achieved through dynamic adjustments in the pulmonary circulation, ensuring that each alveolus receives adequate blood flow relative to the amount of air it receives.
- Hypoxic Vasoconstriction:
In regions of the lung where oxygen levels are low, blood vessels constrict, redirecting blood flow to better-ventilated areas. This mechanism is crucial for optimizing oxygen uptake and preventing ventilation-perfusion mismatch. - Adaptive Regulation:
The lungs continuously adjust the distribution of blood flow and ventilation to respond to changes in body position, activity level, and environmental conditions.
Alveolar Defense Mechanisms
The alveoli are constantly exposed to airborne particles, pathogens, and pollutants. To protect these delicate structures, the lungs employ a range of defense mechanisms:
- Alveolar Macrophages:
These immune cells patrol the alveolar spaces, engulfing and digesting foreign particles and microorganisms. Their activity is essential for maintaining a sterile environment within the lungs. - Mucociliary Escalator:
Although primarily active in the upper airways, the mucociliary clearance system traps inhaled particles and transports them out of the respiratory tract, reducing the burden on the alveoli. - Immune Surveillance:
The alveoli are supported by an array of immune cells that monitor for signs of infection and inflammation, triggering appropriate responses to neutralize potential threats.
Contribution to Acid-Base Homeostasis
By regulating the levels of carbon dioxide—a key component in the body’s acid-base balance—the alveoli play an integral role in maintaining pH homeostasis. Efficient removal of carbon dioxide helps prevent acidosis, ensuring that cellular functions remain within their optimal pH range.
- Buffer System:
The carbon dioxide-bicarbonate buffer system is central to pH regulation, with alveolar gas exchange serving as a critical component of this system. - Metabolic Equilibrium:
By adjusting the rate of ventilation, the body can fine-tune carbon dioxide elimination, maintaining a stable internal environment even under stress.
Recap of Functional Significance
The alveoli are indispensable to respiratory health, serving as the primary sites for oxygen uptake and carbon dioxide elimination. Their roles in surfactant production, ventilation-perfusion matching, immune defense, and acid-base balance underscore their importance in sustaining life. Together, these functions illustrate how the alveoli contribute to both immediate respiratory needs and long-term systemic homeostasis.
Alveolar Health Challenges
While the alveoli are designed for optimal function, various diseases and environmental factors can compromise their structure and efficiency. In this section, we explore the common disorders and conditions that affect alveolar health, detailing their causes, clinical manifestations, and potential complications.
Infectious Processes: Pneumonia
Pneumonia is one of the most frequent and serious infections affecting the alveoli. It is characterized by inflammation and fluid accumulation within the air sacs, which impairs gas exchange and can lead to life-threatening complications.
- Etiology:
Pneumonia can be caused by a range of pathogens, including bacteria (such as Streptococcus pneumoniae), viruses (such as influenza), and, less commonly, fungi. - Clinical Presentation:
Patients typically present with symptoms such as fever, cough, chest pain, and difficulty breathing. In severe cases, the infection can lead to hypoxemia and respiratory failure. - Pathophysiology:
Inflammatory exudates fill the alveoli, reducing the surface area available for gas exchange and causing consolidation of lung tissue.
Chronic Obstructive Pulmonary Disease (COPD)
COPD is a progressive lung disease that encompasses conditions such as emphysema and chronic bronchitis. It is primarily linked to long-term exposure to irritants, with cigarette smoke being the most common culprit.
- Emphysema:
Emphysema involves the destruction of alveolar walls, leading to enlarged air spaces and reduced surface area for gas exchange. This loss of alveolar integrity is irreversible and contributes to chronic respiratory insufficiency. - Chronic Bronchitis:
Characterized by persistent inflammation of the bronchial tubes, chronic bronchitis can also affect alveolar function indirectly by causing mucus hypersecretion and airway obstruction. - Clinical Impact:
Patients often experience progressive shortness of breath, chronic cough, and diminished exercise tolerance, which can severely impact quality of life.
Pulmonary Fibrosis
Pulmonary fibrosis is marked by the excessive formation of scar tissue within the lungs, leading to thickened and stiffened alveolar walls. This process significantly impairs lung compliance and gas exchange.
- Causes:
The condition may be idiopathic or secondary to environmental exposures, medications, or autoimmune disorders. - Symptoms:
Common symptoms include chronic dry cough, progressive breathlessness, and fatigue. The scarring process limits the lung’s ability to expand, resulting in reduced oxygenation. - Long-Term Consequences:
As fibrosis progresses, patients are at increased risk for respiratory failure and may require supplemental oxygen or lung transplantation.
Acute Respiratory Distress Syndrome (ARDS)
ARDS is a severe, often rapidly progressing condition that results from widespread inflammation and fluid accumulation in the alveoli. It is most commonly triggered by severe infections, trauma, or inhalation injuries.
- Pathogenesis:
In ARDS, the alveoli become flooded with inflammatory exudate, leading to marked hypoxemia and reduced lung compliance. - Clinical Course:
The condition requires immediate medical intervention, often including mechanical ventilation, to support respiratory function while the underlying cause is addressed. - Prognosis:
ARDS carries a high mortality rate and can lead to long-term pulmonary complications in survivors.
Alveolar Proteinosis
Alveolar proteinosis is a rare disorder characterized by the accumulation of proteinaceous material within the alveoli. This buildup interferes with normal gas exchange and can lead to respiratory distress.
- Etiology:
The condition is often linked to impaired clearance by alveolar macrophages or autoimmune processes. - Symptoms:
Patients may experience progressive dyspnea, a persistent cough, and fatigue. The gradual filling of the alveolar spaces compromises oxygen diffusion. - Management:
Therapeutic lung lavage is commonly used to remove the accumulated material, and immune-modulating therapies may be beneficial in certain cases.
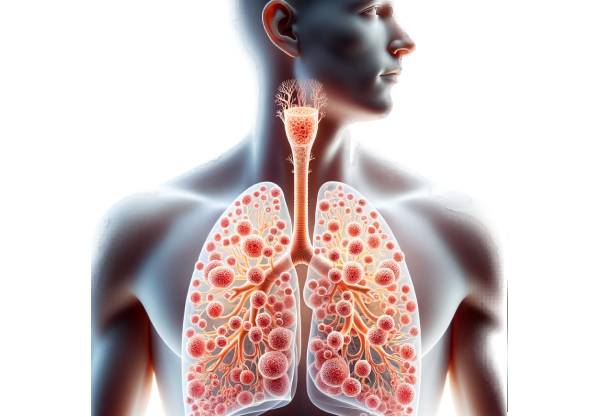
Lung Cancer Involving Alveolar Tissue
Lung cancer can directly affect the alveoli, either by invading the alveolar walls or by forming tumors that obstruct airways. Early detection and treatment are crucial for improving outcomes.
- Pathophysiology:
Malignant cells can disrupt the normal architecture of the alveoli, impeding gas exchange and potentially leading to necrosis of lung tissue. - Clinical Features:
Symptoms often include a persistent cough, chest pain, hemoptysis (coughing up blood), and unexplained weight loss. - Therapeutic Challenges:
Treatment may involve a combination of surgery, chemotherapy, and radiation therapy, depending on the tumor type and stage.
Summarizing the Challenges
Disorders affecting the alveoli can dramatically impair respiratory efficiency and overall health. From infections like pneumonia to chronic conditions such as COPD and pulmonary fibrosis, these diseases underscore the critical need for early detection, targeted treatment, and effective preventive strategies. Recognizing the signs and understanding the underlying mechanisms of these conditions are essential steps toward better respiratory health management.
Comprehensive Diagnostic Methods
Accurate diagnosis of alveolar disorders is paramount for effective treatment. A multidisciplinary approach that integrates clinical evaluation, imaging studies, laboratory tests, and specialized procedures is essential for unraveling the complexity of alveolar pathology. This section outlines the key diagnostic strategies used to assess alveolar health.
Detailed Clinical Evaluation
The diagnostic process begins with a thorough clinical evaluation. A detailed patient history and physical examination provide critical clues about the nature and extent of alveolar involvement.
- Symptom Analysis:
Clinicians assess the duration, severity, and progression of symptoms such as cough, dyspnea, and chest discomfort. Special attention is paid to factors such as recent infections, exposure to environmental toxins, and smoking history. - Physical Examination:
Auscultation of the lungs can reveal abnormal sounds such as crackles, wheezes, or diminished breath sounds, which may indicate underlying alveolar pathology. Additionally, measuring oxygen saturation levels provides immediate feedback on respiratory function.
Imaging Modalities
Imaging techniques are indispensable for visualizing alveolar structure and identifying pathological changes. The following modalities are commonly used:
- Chest X-Ray:
As an initial imaging tool, chest X-rays can reveal areas of consolidation, interstitial markings, and alveolar infiltrates. They are particularly useful for diagnosing pneumonia and identifying gross structural abnormalities. - Computed Tomography (CT) Scan:
CT imaging offers detailed cross-sectional views of the lung, allowing for precise evaluation of alveolar and interstitial changes. High-resolution CT (HRCT) is the gold standard for detecting pulmonary fibrosis, emphysema, and subtle inflammatory changes. - Magnetic Resonance Imaging (MRI):
Although less frequently used for routine lung imaging, MRI can provide valuable information in cases where radiation exposure is a concern or when soft tissue characterization is required. - Positron Emission Tomography (PET) Scan:
PET scans are useful in assessing metabolic activity within lung tissue, aiding in the staging and evaluation of lung cancer. They can help differentiate between benign and malignant lesions by highlighting areas of increased tracer uptake.
Laboratory Assessments
Biochemical tests complement imaging studies by providing insights into the functional status of the alveoli and overall respiratory system.
- Arterial Blood Gas (ABG) Analysis:
ABG tests measure oxygen and carbon dioxide levels in the blood, offering a direct assessment of gas exchange efficiency. They are essential for detecting hypoxemia and hypercapnia. - Complete Blood Count (CBC) and Inflammatory Markers:
A CBC can help identify infections or systemic inflammation, while markers such as C-reactive protein (CRP) may indicate an inflammatory process affecting the lungs. - Sputum Analysis:
Examination of sputum samples can reveal infectious organisms, inflammatory cells, or malignant cells, providing clues to the underlying cause of alveolar dysfunction.
Pulmonary Function Testing
Pulmonary function tests (PFTs) assess lung capacity, airflow, and gas diffusion, offering objective measurements of respiratory performance.
- Spirometry:
This test measures the volume and speed of air that can be inhaled and exhaled, helping to diagnose obstructive and restrictive lung diseases. - Diffusing Capacity for Carbon Monoxide (DLCO):
DLCO testing evaluates the efficiency of gas transfer from the alveoli to the blood. A reduced DLCO can indicate interstitial lung disease, emphysema, or other conditions that impair alveolar-capillary function.
Invasive Procedures and Biopsies
When non-invasive methods are insufficient, invasive procedures may be necessary to obtain tissue samples or further evaluate alveolar pathology.
- Bronchoscopy:
A bronchoscope is used to visualize the airways and alveoli directly. It allows for bronchoalveolar lavage (BAL) to collect cells and fluids, and for transbronchial biopsies to obtain tissue samples. - Surgical Lung Biopsy:
In cases of complex or ambiguous lung disease, a surgical biopsy—often performed via video-assisted thoracoscopic surgery (VATS)—can provide a definitive histopathological diagnosis.
Summary of Diagnostic Strategies
A comprehensive diagnostic workup that combines clinical evaluation, imaging, laboratory testing, and invasive procedures is crucial for accurately identifying alveolar disorders. This multidisciplinary approach enables healthcare providers to tailor treatment strategies based on the precise nature and severity of the disease, ultimately improving patient outcomes.
Advanced Treatment Modalities
Effective management of alveolar disorders requires a multifaceted treatment approach that addresses both the underlying cause and the resultant functional impairment. This section reviews the array of therapeutic strategies available, ranging from pharmacologic interventions to advanced surgical techniques and supportive therapies.
Pharmacologic Interventions
Medications form the cornerstone of treatment for many alveolar disorders. The choice of therapy depends on the specific condition and its severity.
- Antibiotics:
For infectious processes such as pneumonia, appropriate antibiotics are critical. The selection is based on the suspected pathogen and local resistance patterns. - Antivirals and Antifungals:
In cases of viral or fungal lung infections, targeted antiviral or antifungal medications are used to control the spread of infection and reduce inflammation. - Corticosteroids:
These potent anti-inflammatory agents are used in conditions such as COPD exacerbations, interstitial lung diseases, and acute respiratory distress syndrome (ARDS). They help reduce inflammation and improve airflow, though long-term use requires careful monitoring for side effects. - Bronchodilators:
Beta-agonists and anticholinergics are prescribed to relax airway muscles, improving ventilation in obstructive lung diseases like asthma and COPD. - Mucolytics:
Agents such as N-acetylcysteine (NAC) help break down mucus, facilitating its clearance from the airways and reducing the work of breathing.
Supportive and Respiratory Therapies
Supportive treatments play an essential role in managing alveolar dysfunction and maintaining respiratory stability.
- Oxygen Therapy:
Supplemental oxygen is used to maintain adequate blood oxygen levels in patients with chronic or acute hypoxemia. Delivery methods range from nasal cannulae to high-flow oxygen systems. - Mechanical Ventilation:
In severe cases of respiratory failure, mechanical ventilation provides critical support, ensuring proper oxygenation and carbon dioxide removal. Ventilation settings are carefully tailored to the patient’s lung mechanics. - Pulmonary Rehabilitation:
Comprehensive rehabilitation programs combine physical exercise, nutritional counseling, and breathing techniques to improve respiratory muscle strength and overall quality of life. - Extracorporeal Membrane Oxygenation (ECMO):
ECMO is a lifesaving intervention used in critical care settings for patients with severe respiratory or cardiac failure. It temporarily takes over the function of the lungs (and sometimes the heart), allowing time for recovery or bridging to transplantation.
Surgical and Interventional Procedures
When medical management is insufficient, surgical or minimally invasive interventions may be necessary.
- Lung Volume Reduction Surgery (LVRS):
For patients with severe emphysema, LVRS involves the resection of damaged lung tissue, allowing healthier regions to function more effectively and improving overall lung mechanics. - Lung Transplantation:
In end-stage lung disease, transplantation can be the definitive treatment option. Although complex and requiring lifelong immunosuppression, lung transplants can dramatically enhance quality of life and survival. - Bronchoscopic Interventions:
Techniques such as endobronchial valve placement or stent insertion can alleviate airway obstruction and improve ventilation in select patients. - Lung Lavage:
For conditions like alveolar proteinosis, therapeutic lung lavage is used to wash out the proteinaceous material that accumulates in the alveoli, thereby restoring gas exchange.
Emerging and Targeted Therapies
Advances in medical research continue to expand the therapeutic arsenal for alveolar disorders.
- Targeted Molecular Therapy:
For lung cancers and other malignancies affecting the alveoli, targeted therapies that block specific molecular pathways are being developed. These agents offer the potential for effective treatment with fewer systemic side effects. - Immunotherapy:
Harnessing the body’s immune system to combat malignancies is an exciting frontier in the treatment of lung cancer. Immune checkpoint inhibitors and other immunotherapeutic agents have shown promise in improving survival rates. - Regenerative Medicine:
Stem cell therapies and tissue engineering techniques are being investigated as potential treatments for repairing damaged alveolar structures, with the long-term goal of restoring normal lung function.
Recap of Therapeutic Strategies
The management of alveolar disorders is complex and requires a tailored approach that combines pharmacologic treatments, supportive care, and, when necessary, surgical interventions. By targeting both the underlying pathology and its functional consequences, these advanced treatment modalities aim to restore effective gas exchange, alleviate symptoms, and improve patient outcomes.
Nutritional & Supplementary Interventions
In addition to conventional medical therapies, nutrition and targeted supplements can play a significant role in supporting alveolar health. Optimizing dietary intake and incorporating specific nutrients may help reduce inflammation, protect against oxidative stress, and promote overall lung function.
Key Nutrients for Lung Health
A well-balanced diet is fundamental to maintaining the integrity and functionality of the alveoli. Several nutrients have been identified as particularly beneficial for respiratory health:
- Omega-3 Fatty Acids:
These essential fats, found in fish oils and flaxseeds, possess strong anti-inflammatory properties. By reducing inflammation in the lung tissue, omega-3s help preserve alveolar integrity and improve overall respiratory function. - Vitamin D:
Beyond its role in bone health, vitamin D is crucial for immune modulation. Adequate levels of vitamin D have been linked to a reduced risk of respiratory infections and improved lung function. - Vitamin C:
As a potent antioxidant, vitamin C protects the alveolar cells from oxidative damage caused by environmental pollutants and free radicals. Its immune-boosting effects further contribute to respiratory resilience. - Magnesium:
This mineral supports muscle relaxation and can help reduce bronchospasm, facilitating easier breathing and optimal lung function.
Herbal and Natural Supplements
Certain herbal supplements and natural compounds have demonstrated benefits for lung health, particularly in reducing inflammation and enhancing mucociliary clearance:
- N-Acetylcysteine (NAC):
NAC serves as a mucolytic agent, breaking down thick mucus and improving its clearance from the airways. In addition, it boosts glutathione production, a key antioxidant that protects lung tissue. - Turmeric (Curcumin):
With its potent anti-inflammatory properties, curcumin can help reduce lung inflammation and support the repair of damaged alveolar cells. - Green Tea Extract:
Rich in antioxidants such as catechins, green tea extract may help mitigate oxidative stress in the lungs and enhance overall respiratory health. - Ginger:
Known for its anti-inflammatory and antiemetic properties, ginger can improve respiratory comfort and support immune function.
The Role of Antioxidants
Oxidative stress is a major contributor to lung tissue damage and alveolar dysfunction. Incorporating antioxidants into one’s diet can help neutralize harmful free radicals and protect the delicate alveolar structures.
- Glutathione:
Often referred to as the body’s “master antioxidant,” glutathione plays a central role in detoxifying the lungs. Supplementation may be beneficial for individuals with chronic lung conditions. - Coenzyme Q10:
This antioxidant supports cellular energy production and may help improve lung muscle function and overall respiratory efficiency.
Dietary Strategies for Respiratory Wellness
Adopting a lung-friendly diet involves more than just adding supplements—it requires a holistic approach to nutrition:
- Whole Foods:
Focus on consuming a variety of fruits, vegetables, lean proteins, and whole grains. These foods provide essential vitamins, minerals, and antioxidants that support lung health. - Anti-Inflammatory Diet:
Incorporate foods known to reduce inflammation, such as leafy greens, nuts, berries, and fatty fish. - Hydration:
Adequate water intake is essential for maintaining mucociliary clearance and overall cellular function in the lungs.
In Summary
Nutritional and supplementary interventions can significantly enhance alveolar health by reducing inflammation, combating oxidative stress, and supporting the body’s natural defense mechanisms. When combined with traditional medical treatments, these strategies offer a holistic approach to respiratory wellness.
Strategies for Optimal Alveolar Function
Maintaining the health of your alveoli requires a proactive approach that extends beyond clinical treatment. Lifestyle modifications and preventive measures play a crucial role in preserving lung function and preventing respiratory diseases. This section provides actionable strategies for optimizing alveolar health through everyday habits.
Smoking Cessation and Avoidance of Pollutants
Smoking is one of the most significant risk factors for alveolar damage. Quitting smoking and minimizing exposure to environmental pollutants are critical steps toward preserving lung health.
- Quit Smoking:
Cessation of tobacco use leads to a marked improvement in lung function over time. Support groups, counseling, and nicotine replacement therapies can aid in quitting. - Avoid Air Pollutants:
Reduce exposure to industrial chemicals, dust, and secondhand smoke. Consider using air purifiers at home and avoiding outdoor activities during periods of poor air quality.
Regular Physical Activity
Exercise not only enhances cardiovascular health but also strengthens the respiratory muscles and improves lung capacity.
- Aerobic Exercise:
Activities such as walking, cycling, and swimming promote better oxygen utilization and improve alveolar ventilation. - Breathing Exercises:
Techniques such as diaphragmatic breathing, pursed-lip breathing, and yoga can help improve lung efficiency and increase the strength of respiratory muscles. - Posture and Mobility:
Maintaining good posture supports optimal lung expansion. Regular stretching and core-strengthening exercises contribute to overall respiratory health.
Nutritional and Hydration Practices
A balanced diet rich in antioxidants and anti-inflammatory foods supports alveolar function, while proper hydration is essential for mucus clearance.
- Balanced Diet:
Emphasize nutrient-dense foods that support lung repair and reduce inflammation. - Hydration:
Drinking adequate water throughout the day is crucial for thinning mucus and facilitating its clearance from the respiratory tract.
Preventive Healthcare Measures
Regular health monitoring and preventive care are essential for early detection and management of potential alveolar disorders.
- Vaccinations:
Stay up to date with influenza and pneumococcal vaccines to reduce the risk of respiratory infections. - Regular Check-Ups:
Periodic medical evaluations, including lung function tests, can help detect early signs of respiratory impairment. - Environmental Awareness:
Monitor air quality indices and take precautions on days when pollution levels are high.
Stress Management and Overall Wellness
Chronic stress can have systemic effects, including on the respiratory system. Implementing stress management techniques can indirectly benefit alveolar function.
- Mindfulness and Meditation:
Regular meditation sessions can reduce stress levels, indirectly supporting overall lung health. - Adequate Sleep:
Quality sleep is vital for cellular repair and immune function, both of which contribute to healthy alveoli. - Balanced Lifestyle:
Combining physical activity, a healthy diet, and stress management fosters an environment conducive to optimal respiratory health.
Summary of Lifestyle Recommendations
By incorporating these practical strategies into your daily routine, you can protect and enhance the function of your alveoli. These measures not only improve immediate respiratory function but also contribute to long-term lung health, reducing the risk of chronic respiratory diseases and enhancing overall well-being.
Reputable Resources for Respiratory Health
Accessing reliable information is paramount for managing and improving lung health. The following curated list of resources—including books, academic journals, and mobile applications—provides trusted guidance and cutting-edge insights into alveolar and respiratory health.
Recommended Books
- “The Respiratory System at a Glance” by Jeremy P. T. Ward and Jane Ward:
This book offers a concise and visual overview of lung anatomy and physiology, making it a valuable resource for both students and healthcare professionals. - “Respiratory Physiology: The Essentials” by John B. West:
A definitive guide that delves into the mechanisms of pulmonary function and gas exchange, providing foundational knowledge critical for understanding alveolar dynamics. - “Breathe: The Simple, Revolutionary 14-Day Program to Improve Your Mental and Physical Health” by Belisa Vranich:
This book combines practical breathing exercises with insights into respiratory health, offering readers strategies to optimize lung function.
Academic Journals
- American Journal of Respiratory and Critical Care Medicine:
A leading publication that features the latest research on respiratory diseases, critical care, and innovative treatment approaches. - Chest:
A peer-reviewed journal dedicated to chest medicine, including clinical studies and reviews on lung health, respiratory therapy, and related topics.
Mobile Applications
- MyFitnessPal:
This app assists with tracking nutrition and exercise, supporting overall health and indirectly benefiting respiratory function. - Calm:
Designed to help manage stress through guided meditation and relaxation techniques, Calm can contribute to improved respiratory and overall health. - AirVisual:
A real-time air quality monitoring app that helps users avoid exposure to harmful pollutants, thereby protecting lung and alveolar function.
Recap of Resource Value
These resources offer invaluable insights into respiratory health, ranging from foundational textbooks and peer-reviewed journals to practical mobile applications. Leveraging these tools can empower individuals and healthcare professionals alike to stay informed and proactive about lung and alveolar health.
Frequently Asked Questions
What is the primary role of the alveoli in respiration?
The alveoli are the microscopic air sacs in the lungs where oxygen diffuses into the blood and carbon dioxide is removed. Their thin walls and extensive capillary network ensure rapid and efficient gas exchange.
How does surfactant benefit alveolar function?
Surfactant, produced by type II pneumocytes, reduces surface tension within the alveoli, preventing collapse during exhalation and ensuring uniform ventilation across different lung regions.
What are common conditions that affect alveolar health?
Common alveolar disorders include pneumonia, chronic obstructive pulmonary disease (COPD), pulmonary fibrosis, acute respiratory distress syndrome (ARDS), and alveolar proteinosis, all of which can impair gas exchange.
Which diagnostic tests are used to assess alveolar function?
Diagnostic evaluation typically includes imaging studies (chest X-ray, CT scan), pulmonary function tests (spirometry, DLCO), blood gas analysis, and sometimes invasive procedures like bronchoscopy with biopsy.
What lifestyle changes can help maintain healthy alveoli?
Adopting habits such as smoking cessation, regular exercise, a balanced diet rich in antioxidants, proper hydration, and avoiding air pollutants can significantly enhance alveolar function and overall lung health.
Disclaimer: The information provided in this article is for educational purposes only and is not a substitute for professional medical advice. Always consult a qualified healthcare provider for personalized guidance and treatment options.
We encourage you to share this article on Facebook, X (formerly Twitter), or your preferred social media platforms to help spread awareness about respiratory health and empower others with valuable knowledge!