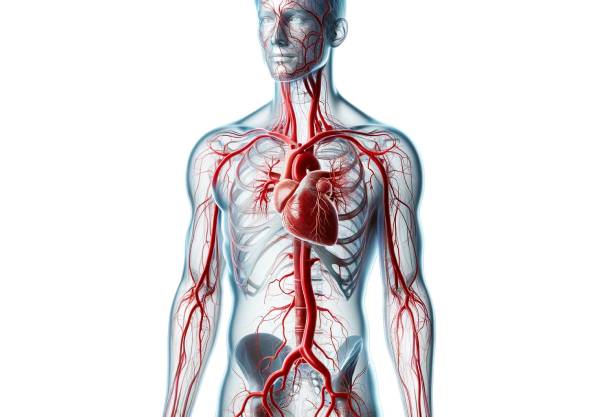
Arteries are vital blood vessels that transport oxygenated blood from the heart to every cell in the body. Their complex structure—comprising multiple layers designed for strength, flexibility, and regulation—allows them to withstand high pressure and adapt to varying circulatory demands. This guide delves into arterial anatomy, explores the essential functions arteries perform, examines common disorders affecting them, and reviews modern diagnostic and treatment strategies. In addition, practical nutritional and lifestyle tips are provided to help maintain optimal arterial health, ensuring a well-functioning cardiovascular system and overall wellness.
Table of Contents
- Detailed Arterial Structure
- Vital Arterial Functions
- Major Arterial Systems
- Common Arterial Disorders
- Diagnostic Techniques
- Treatment Interventions
- Nutritional & Supplementary Support
- Lifestyle Strategies
- Trusted Resources
- Frequently Asked Questions
Detailed Arterial Structure
Arteries are designed with a multi-layered structure that ensures durability and the ability to respond dynamically to the pulsatile force of blood flow. Each artery consists of three primary layers that contribute uniquely to its function.
Tunica Intima
The innermost layer of an artery, the tunica intima, is composed of:
- Endothelial Cells:
These cells form a smooth, continuous lining that minimizes friction, facilitating efficient blood flow. Their anti-thrombotic properties help prevent clot formation. - Basement Membrane & Connective Tissue:
A delicate meshwork that supports the endothelial cells, aids in nutrient exchange, and serves as a barrier against harmful substances.
Tunica Media
The middle layer, the tunica media, is the most substantial part of the arterial wall:
- Smooth Muscle Cells:
These cells are responsible for vasoconstriction and vasodilation, allowing arteries to regulate their diameter and, consequently, blood pressure. - Elastic Fibers:
Predominantly found in large arteries (elastic arteries), these fibers allow vessels like the aorta to expand during systole and recoil during diastole, thus smoothing out the pulsatile flow of blood.
Tunica Externa (Adventitia)
The outermost layer, the tunica externa, provides structural support:
- Connective Tissue:
This layer is rich in collagen, which offers strength and resilience. - Vasa Vasorum and Nerves:
Small blood vessels (vasa vasorum) supply nutrients to the arterial wall, while nerve fibers regulate vascular tone and coordinate responses to various stimuli.
Structural Adaptations
Arteries exhibit variations in their structure depending on their size and function:
- Elastic Arteries:
Large arteries like the aorta have a thick tunica media with abundant elastic fibers, which buffer the high-pressure output of the heart. - Muscular Arteries:
These arteries contain more smooth muscle cells relative to elastic fibers, allowing fine-tuned regulation of blood flow to specific organs. - Arterioles:
The smallest arterial branches, arterioles, have a thin wall that is crucial for controlling peripheral resistance and blood pressure.
This sophisticated architecture enables arteries to perform reliably under continuous stress while maintaining the flexibility to adapt to the body’s changing circulatory needs.
Vital Arterial Functions
Arteries play a central role in maintaining circulatory homeostasis by ensuring that oxygenated blood reaches tissues and organs efficiently. Their functions extend far beyond mere conduits for blood.
Blood Distribution and Oxygenation
- Oxygen Transport:
Arteries deliver oxygen-rich blood from the heart to every part of the body, ensuring that cells have the oxygen needed for aerobic metabolism. - Nutrient Delivery:
They also transport essential nutrients, including glucose, amino acids, and lipids, which are vital for cell repair, growth, and energy production.
Regulation of Blood Pressure and Flow
The muscular walls of arteries allow for dynamic regulation of blood pressure:
- Vasoconstriction and Vasodilation:
Smooth muscle contraction narrows the vessel, increasing resistance and raising blood pressure. Conversely, relaxation of these muscles dilates the vessel, reducing resistance. - Baroreceptor Function:
Specialized sensors located in the arterial walls (e.g., in the carotid sinus and aortic arch) detect changes in blood pressure and initiate reflexes to maintain homeostasis.
Elasticity and Hemodynamic Stability
- Elastic Recoil:
Elastic arteries expand to accommodate the surge of blood during systole and recoil during diastole, ensuring a steady flow of blood even when the heart is at rest. - Buffering Pulsatile Flow:
This elastic property reduces the pulsatile force of blood, protecting smaller vessels and capillaries from damage.
Maintenance of Vascular Integrity
- Endothelial Function:
The endothelium not only reduces friction but also produces vital substances like nitric oxide, which helps maintain vascular tone and prevent thrombosis. - Inflammatory Response:
In response to injury or stress, arteries can recruit immune cells to the site, facilitating repair processes and protecting against infections.
Through these diverse functions, arteries ensure that every cell in the body receives the oxygen and nutrients it requires while maintaining systemic blood pressure and vascular health.
Major Arterial Systems
The arterial system is an extensive network, with major arteries branching into smaller vessels that supply the entire body. Understanding these systems highlights the integral role arteries play in overall circulation.
The Aorta
- Primary Conduit:
As the largest artery in the body, the aorta originates from the left ventricle and distributes oxygenated blood to all systemic arteries. - Branching Patterns:
It gives rise to critical branches such as the coronary arteries, which supply the heart, and the brachiocephalic, carotid, and subclavian arteries, which serve the brain, neck, and arms.
Coronary Arteries
- Heart’s Lifeline:
These arteries branch off from the aorta and provide the myocardium with oxygen and nutrients essential for continuous heart function. - Clinical Significance:
Obstructions in coronary arteries can lead to ischemia and myocardial infarction (heart attacks).
Carotid Arteries
- Cerebral Supply:
The common carotid arteries split into internal and external branches, supplying blood to the brain and facial structures. - Stroke Prevention:
Maintaining the health of the carotid arteries is crucial for preventing cerebrovascular accidents (strokes).
Pulmonary Arteries
- Lung Circulation:
Unlike systemic arteries, pulmonary arteries carry deoxygenated blood from the right ventricle to the lungs for gas exchange. - Unique Physiology:
These arteries operate under lower pressure compared to systemic arteries, reflecting their specialized role in the pulmonary circuit.
Peripheral Arteries
- Distribution to Limbs:
Muscular arteries supply blood to the arms and legs, ensuring that tissues receive adequate oxygen during both rest and physical activity. - Regulation of Local Blood Flow:
These vessels adjust their diameter based on the metabolic demands of the tissues they serve, providing precise control of blood distribution.
Each of these arterial systems plays a distinct role in maintaining the body’s circulatory efficiency and overall health.
Common Arterial Disorders
Various conditions can compromise arterial health, leading to significant cardiovascular risks. This section explores the most prevalent arterial disorders, their causes, and their clinical implications.
Atherosclerosis
- Pathophysiology:
Atherosclerosis involves the buildup of fatty plaques within arterial walls, initiated by endothelial injury. These plaques consist of lipids, inflammatory cells, and fibrous tissue. - Risk Factors:
High cholesterol, hypertension, smoking, diabetes, and sedentary lifestyles contribute to plaque formation. - Clinical Consequences:
Plaque buildup narrows the arteries, reducing blood flow and increasing the risk of heart attacks, strokes, and peripheral artery disease.
Hypertension
- Definition:
Hypertension is the chronic elevation of blood pressure, which places excessive strain on arterial walls. - Contributing Factors:
Genetic predisposition, high salt intake, obesity, and stress are key contributors. - Complications:
Over time, uncontrolled hypertension can lead to arterial damage, atherosclerosis, and complications such as heart failure and kidney disease.
Aneurysms
- Nature of Aneurysms:
An aneurysm is an abnormal bulge in an arterial wall resulting from weakness in the vessel structure. They can be saccular (berry-shaped) or fusiform (spindle-shaped). - Risks:
Aneurysms may remain asymptomatic until rupture, which can cause catastrophic internal bleeding and high mortality. - Management:
Early detection and surgical or endovascular repair are essential to prevent rupture.
Peripheral Artery Disease (PAD)
- Definition:
PAD is caused by atherosclerotic plaque accumulation in the arteries supplying the limbs, leading to reduced blood flow. - Symptoms:
Patients often experience claudication—pain or cramping in the legs during exercise—which may progress to critical limb ischemia. - Treatment:
Lifestyle modifications, medications, and sometimes surgical interventions (such as angioplasty) are used to improve blood flow.
Raynaud’s Phenomenon
- Mechanism:
This condition is characterized by episodic vasoconstriction of small arteries, particularly in the fingers and toes, in response to cold or stress. - Symptoms:
Affected areas may change color (white to blue to red) and become numb or painful during attacks. - Management:
Treatment focuses on avoiding triggers and using vasodilator medications to improve blood flow.
Understanding these disorders is crucial for early intervention and for adopting strategies to prevent progression and complications.
Diagnostic Techniques
Accurate diagnosis of arterial diseases relies on a combination of clinical assessments, laboratory tests, and advanced imaging techniques. This comprehensive diagnostic approach enables healthcare providers to identify the nature and extent of arterial damage.
Clinical Assessment
- History and Physical Examination:
Detailed patient history regarding chest pain, leg pain, or other circulatory symptoms is essential. Physical examination may reveal weak pulses, abnormal sounds (bruits), and signs of poor tissue perfusion. - Risk Factor Evaluation:
Assessing lifestyle factors such as smoking, diet, and exercise habits helps identify patients at risk for arterial disorders.
Laboratory Tests
- Blood Tests:
Evaluating lipid profiles, blood glucose levels, and inflammatory markers like C-reactive protein (CRP) helps determine cardiovascular risk. - Biomarkers:
Specific biomarkers can indicate the presence and severity of arterial inflammation and atherosclerotic progression.
Imaging Modalities
- Doppler Ultrasound:
A non-invasive method that uses sound waves to assess blood flow velocity and detect arterial narrowing or blockages, particularly useful for evaluating PAD and carotid artery stenosis. - Computed Tomography Angiography (CTA):
CTA provides detailed cross-sectional images of the arteries, enabling visualization of plaques, aneurysms, and other structural abnormalities. - Magnetic Resonance Angiography (MRA):
MRA offers high-resolution images of blood vessels without the use of ionizing radiation, ideal for patients who require repeated imaging. - Coronary Angiography:
This invasive technique involves catheterization and contrast dye injection to directly visualize the coronary arteries, making it the gold standard for diagnosing coronary artery disease. - Intravascular Ultrasound (IVUS) and Optical Coherence Tomography (OCT):
These advanced imaging methods provide detailed views of the arterial wall and plaque composition, aiding in the planning of interventional procedures.
Functional Assessments
- Ankle-Brachial Index (ABI):
By comparing blood pressure measurements in the ankles and arms, ABI helps diagnose PAD and assess the severity of arterial blockages. - Stress Testing:
Evaluates how the heart and arteries respond to physical exertion, revealing ischemia or abnormal blood flow patterns that might not be evident at rest.
A thorough diagnostic workup is critical for tailoring treatment plans and ensuring that arterial disorders are managed effectively before they lead to severe complications.
Treatment Interventions
Managing arterial disorders involves a multifaceted approach that includes lifestyle modifications, pharmacotherapy, and interventional or surgical procedures. The goal is to restore and maintain optimal blood flow while reducing cardiovascular risks.
Lifestyle Modifications
- Dietary Changes:
Adopting a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins helps lower cholesterol and blood pressure. Reducing sodium intake is particularly important for managing hypertension. - Physical Activity:
Regular exercise—such as walking, cycling, or swimming—improves circulation, strengthens the heart, and reduces arterial stiffness. - Smoking Cessation:
Eliminating tobacco use is crucial to prevent further damage to arterial walls and reduce the risk of atherosclerosis. - Weight Management:
Maintaining a healthy weight lessens the burden on the cardiovascular system and improves overall arterial function. - Stress Reduction:
Techniques like meditation, yoga, and deep breathing help manage stress, which can have a positive impact on blood pressure and vascular health.
Pharmacologic Therapies
- Anti-platelet Agents:
Medications such as aspirin and clopidogrel help prevent blood clot formation by inhibiting platelet aggregation, thus reducing the risk of heart attack and stroke. - Statins:
These cholesterol-lowering drugs not only reduce lipid levels but also stabilize arterial plaques, slowing the progression of atherosclerosis. - Antihypertensives:
A range of medications—including ACE inhibitors, beta-blockers, and calcium channel blockers—are used to control high blood pressure and reduce the strain on arterial walls. - Vasodilators:
Drugs like nitroglycerin help widen blood vessels, improving blood flow and alleviating angina (chest pain). - Novel Agents:
Emerging therapies targeting inflammatory pathways and oxidative stress are under investigation for their potential to improve arterial health.
Interventional Procedures
- Angioplasty and Stenting:
This minimally invasive procedure involves inflating a balloon catheter to widen narrowed arteries, followed by stent placement to keep the vessel open. It is widely used to treat coronary and peripheral artery disease. - Coronary Artery Bypass Grafting (CABG):
CABG surgery creates a bypass around blocked coronary arteries using grafts from other parts of the body, significantly improving blood flow to the heart. - Endarterectomy:
The surgical removal of plaque from an artery, often performed on carotid arteries, to restore normal blood flow and reduce the risk of stroke. - Aneurysm Repair:
Aneurysms may be treated with either open surgical repair or endovascular techniques using stent grafts to reinforce weakened arterial walls. - Emerging Interventions:
Advances in minimally invasive and robotic-assisted surgeries continue to improve outcomes and reduce recovery times for patients with arterial disease.
A personalized treatment plan that integrates lifestyle modifications, medications, and, when necessary, interventional procedures is essential for effective management of arterial disorders.
Nutritional & Supplementary Support
In addition to conventional treatments, nutritional strategies and supplements play a supportive role in maintaining arterial health. Optimizing your diet can help reduce inflammation, lower cholesterol, and improve overall vascular function.
Essential Nutrients
- Omega-3 Fatty Acids:
Found in fish oil and flaxseed, these fatty acids are known to reduce inflammation and improve arterial flexibility, thereby supporting cardiovascular health. - Vitamin D:
Adequate vitamin D levels are associated with improved endothelial function and lower risk of arterial stiffness. - Magnesium:
This mineral promotes relaxation of vascular smooth muscle, helping to regulate blood pressure and maintain arterial tone. - Antioxidant Vitamins:
Vitamins C and E protect arterial walls from oxidative damage by neutralizing free radicals.
Herbal Supplements
- Garlic Extract:
Garlic has been widely studied for its cardiovascular benefits, including its ability to lower blood pressure and reduce plaque buildup. - Turmeric (Curcumin):
The anti-inflammatory properties of curcumin help mitigate oxidative stress and support the repair of arterial tissues. - Green Tea Extract:
Rich in catechins, green tea extract is a potent antioxidant that can improve endothelial function and reduce arterial inflammation.
Enzyme and Coenzyme Support
- Coenzyme Q10 (CoQ10):
CoQ10 supports cellular energy production and helps protect arterial cells from oxidative stress. - Digestive Enzymes:
Although primarily known for aiding digestion, certain enzymes may help optimize nutrient absorption, ensuring that the body receives the vitamins and minerals necessary for arterial repair and maintenance.
Dietary Strategies
- Adopt a Heart-Healthy Diet:
Emphasize whole foods, lean proteins, healthy fats, and plenty of fruits and vegetables to provide the nutrients required for arterial health. - Regular Meal Timing:
Consistent eating patterns help regulate metabolism and maintain steady energy levels, supporting overall cardiovascular function. - Hydration:
Adequate water intake is essential for proper circulation and the optimal function of all bodily systems, including the arteries.
By integrating these nutritional and supplementary approaches, you can bolster your arterial health and reduce the risk of cardiovascular diseases.
Lifestyle Strategies for Optimal Arterial Wellness
Maintaining healthy arteries goes beyond medical treatments and requires a proactive, comprehensive lifestyle approach. Incorporating the following strategies into your daily routine can promote arterial wellness and overall cardiovascular health.
Heart-Healthy Diet and Hydration
- Balanced Nutrition:
Consume a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. Such a diet not only supports arterial health but also reduces the risk of chronic diseases. - Fiber Intake:
High-fiber foods aid in lowering cholesterol levels and promoting vascular health. - Stay Hydrated:
Drinking sufficient water helps maintain blood volume and supports proper circulation.
Regular Physical Activity
- Aerobic Exercise:
Activities like brisk walking, jogging, cycling, and swimming strengthen the cardiovascular system, improve blood flow, and enhance arterial elasticity. - Strength Training:
Incorporate resistance exercises to build muscle mass, which can improve metabolism and support overall heart health. - Flexibility and Balance:
Yoga and stretching exercises promote relaxation and reduce stress, contributing indirectly to arterial health.
Avoidance of Harmful Substances
- Smoking Cessation:
Quitting smoking is one of the most effective ways to protect your arteries, as tobacco use is a major risk factor for atherosclerosis and other cardiovascular diseases. - Moderate Alcohol Consumption:
Excessive alcohol intake can raise blood pressure and damage arterial walls, so moderation is key.
Stress Management and Sleep
- Reduce Stress:
Engage in stress-reducing activities such as meditation, deep breathing exercises, and mindfulness practices. Chronic stress can negatively impact blood pressure and arterial function. - Prioritize Quality Sleep:
Aim for 7–9 hours of quality sleep per night to allow your body to recover and maintain optimal cardiovascular health.
Regular Health Monitoring
- Blood Pressure Checks:
Regular monitoring of blood pressure helps in early detection and management of hypertension. - Cholesterol and Glucose Testing:
Routine blood tests can provide insights into your cardiovascular risk factors and guide preventive strategies. - Medical Check-Ups:
Regular visits to your healthcare provider can help detect arterial issues early, allowing for timely intervention.
By embracing these lifestyle practices, you can create a strong foundation for arterial health and reduce your risk of developing cardiovascular complications.
Trusted Resources for Arterial Health
Access to reliable information is crucial for making informed decisions about your arterial and cardiovascular health. Below is a curated list of reputable resources that offer comprehensive insights into arterial health, research, and clinical practices.
Recommended Books
- “The Cardiovascular Cure” by John P. Cooke:
An insightful guide that explores innovative approaches to reversing heart disease and maintaining vascular health. - “Beat the Heart Attack Gene” by Bradley Bale and Amy Doneen:
This book delves into personalized strategies for reducing cardiovascular risk and enhancing arterial function. - “The End of Heart Disease” by Joel Fuhrman:
Offers a nutritional perspective on preventing and reversing arterial and cardiovascular diseases through a plant-based diet.
Academic Journals
- Journal of the American College of Cardiology (JACC):
A leading journal that publishes cutting-edge research on all aspects of cardiovascular health, including arterial pathology. - Circulation:
Focused on cardiovascular research, this journal covers advances in diagnosis, treatment, and prevention of arterial and heart diseases.
Mobile Applications
- MyFitnessPal:
An app that tracks your diet and exercise, helping you maintain a heart-healthy lifestyle. - Blood Pressure Companion:
Provides tools for monitoring and managing your blood pressure, essential for arterial health. - Headspace:
A mindfulness and meditation app that supports stress reduction, which is beneficial for cardiovascular wellness.
Frequently Asked Questions
What is the primary function of arteries?
Arteries transport oxygen-rich blood from the heart to tissues throughout the body, delivering essential nutrients and oxygen for cellular metabolism while helping regulate blood pressure.
How do arteries regulate blood pressure?
Arteries adjust blood pressure through vasoconstriction and vasodilation. Their smooth muscle layers contract or relax in response to hormonal and neural signals, controlling the vessel diameter and peripheral resistance.
What causes atherosclerosis?
Atherosclerosis is caused by the buildup of fatty plaques in the arterial walls, which result from factors like high cholesterol, hypertension, smoking, diabetes, and inflammation.
What imaging techniques are used to diagnose arterial disorders?
Common imaging techniques include Doppler ultrasound, CT angiography, MR angiography, and coronary angiography, all of which help visualize arterial blockages, aneurysms, and structural abnormalities.
How can I support arterial health through lifestyle changes?
Maintaining a heart-healthy diet, engaging in regular exercise, quitting smoking, managing stress, and monitoring blood pressure are key strategies for supporting arterial health and reducing cardiovascular risks.
Disclaimer: The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a qualified healthcare provider for personalized guidance and treatment options.
We encourage you to share this article on Facebook, X (formerly Twitter), or your preferred social media platform to help spread awareness about arterial health and empower others with valuable knowledge!




