Introduction
Arteritic anterior ischemic optic neuropathy (AAION) is a serious ocular condition marked by sudden vision loss caused by inflammation and occlusion of the arteries that supply blood to the optic nerve head. It is most commonly associated with giant cell arteritis (GCA), an inflammatory disease of the blood vessels that primarily affects older people. Awareness and early detection of AAION are critical because prompt treatment can prevent additional vision loss and lower the risk of serious systemic complications such as stroke and blindness in the other eye. Early detection and treatment of the underlying GCA is critical for maintaining vision and overall health.
Insights into Arteritic Anterior Ischemic Optic Neuropathy
Arteritic anterior ischemic optic neuropathy (AAION) is a type of optic neuropathy caused by inadequate blood supply to the optic nerve head as a result of small artery inflammation and thrombosis. This condition differs from non-arteritic anterior ischemic optic neuropathy (NAION), which is caused by non-inflammatory vascular occlusions. Understanding the pathophysiology, risk factors, and clinical characteristics of AAION is critical for prompt diagnosis and treatment.
Pathophysiology
The underlying cause of AAION is giant cell arteritis (GCA), also referred to as temporal arteritis. GCA is a systemic vasculitis that primarily affects medium and large arteries, with a focus on the extracranial branches of the carotid artery. The exact cause of GCA remains unknown, but it is thought to be a combination of genetic predisposition and immune-mediated mechanisms.
- Vascular Inflammation: GCA causes inflammation of the arterial walls as a result of an abnormal immune response. Giant cells are large, multinucleated immune cells that infiltrate vessel walls, causing granulomatous inflammation.
- Lumen Narrowing and Occlusion: Inflammation thickens the arterial walls, decreasing lumen diameter and impeding blood flow. This can result in thrombosis (blood clot formation), which further obstructs the blood supply.
- Ischemia of the Optic Nerve Head: The optic nerve head, or optic disc, is extremely sensitive to changes in blood flow. When the inflammatory process occludes the posterior ciliary arteries that supply the optic nerve head, ischemia (insufficient blood supply) occurs. This causes optic nerve damage and subsequent vision loss.
Risk Factors
Several factors can increase the risk of developing AAION, most of which are related to the underlying risk of GCA:
- Age: GCA, and thus AAION, primarily affects people over the age of 50, and the incidence rises with age.
- Gender: Women are more commonly affected by GCA than men, making them more vulnerable to AAION.
- Genetic Predisposition: Genetic factors influence the development of GCA. Specific genetic markers, such as HLA-DRB1*04, have been linked to an increased risk.
- Ethnicity: GCA is more common in Northern Europeans than in Asians and Africans.
Clinical Features
AAION is distinguished by the rapid onset of visual symptoms, which are frequently accompanied by systemic signs of GCA. Recognizing these clinical features is critical for early detection and treatment.
- Sudden Vision Loss: Patients with AAION usually have sudden, painless vision loss in one eye. The vision loss is often severe and can affect the central, peripheral, or both fields of vision.
- Scalp Tenderness: One of the most common symptoms of GCA is scalp tenderness, particularly around the temporal arteries. Patients may experience pain while combing their hair or wearing hats.
- Jaw Claudication: One of the most common symptoms of GCA is pain in the jaw muscles while chewing. This is caused by a reduction in blood flow to the masticatory muscles.
- Headache: Patients with GCA frequently report persistent, severe headaches, which are often localized to the temple area.
- Polymyalgia Rheumatica: Some GCA patients may also exhibit polymyalgia rheumatica symptoms, such as muscle pain and stiffness, particularly in the shoulders and hips.
- Systemic Symptoms: Common systemic symptoms of GCA include fever, fatigue, weight loss, and general malaise.
Differential Diagnosis
It is critical to distinguish AAION from other causes of optic neuropathy in order to provide appropriate treatment. Key differential diagnoses include:
- Non-Arteritic Anterior Ischemic Optic Neuropathy (NAION): NAION causes sudden vision loss but is not linked to systemic inflammation. It usually affects younger people who have cardiovascular risk factors like hypertension, diabetes, and hypercholesterolemia.
- Optic Neuritis: Inflammatory demyelination of the optic nerve, often associated with multiple sclerosis, characterized by vision loss and pain with eye movement. It primarily affects young adults.
- Central Retinal Artery Occlusion (CRAO): CRAO causes sudden, severe vision loss due to occlusion of the central retinal artery. Unlike AAION, CRAO is not linked to systemic inflammatory symptoms.
Complications
If not treated promptly, AAION can cause severe and irreversible vision loss. Complications include:
- Permanent Vision Loss: The ischemic damage to the optic nerve is frequently irreversible, resulting in permanent vision impairment or blindness in the affected eye.
- Bilateral Involvement: Without treatment, AAION can spread to the contralateral eye, resulting in bilateral blindness.
- Systemic Complications: GCA can result in systemic complications such as aortic aneurysm, aortic dissection, or stroke. These complications result from the involvement of larger arteries beyond the optic nerve.
Prognosis
The prognosis of AAION is dependent on timely diagnosis and treatment. Early treatment with high-dose corticosteroids can prevent additional vision loss and lower the risk of bilateral involvement. However, vision loss that occurs prior to treatment is usually permanent.
Public Awareness and Advocacy
Raising awareness of AAION and GCA is critical for early diagnosis and treatment. Advocacy groups and patient organizations play critical roles in educating the general public and healthcare providers about the signs and symptoms of these conditions. They also provide assistance and resources to affected individuals and their families.
Risk Reduction for Arteritic Anterior Ischemic Optic Neuropathy
- Regular Medical Check-Ups: Make regular appointments with your healthcare provider, especially if you are over 50 years old. Routine visits can help detect early signs of GCA and other conditions before they progress to AAION.
- Monitor Symptoms: Be aware of symptoms such as persistent headaches, scalp tenderness, jaw pain while chewing, and sudden vision changes. Please notify your doctor as soon as possible if you experience these symptoms.
- Manage Cardiovascular Health: Live a healthy lifestyle to reduce your risk of cardiovascular disease, including hypertension, diabetes, and hypercholesterolemia. Regular exercise, a healthy diet, and quitting smoking can all help reduce the risk of vascular complications.
- Educate Yourself: Discover the symptoms and risk factors for GCA and AAION. Awareness can lead to early detection and prompt medical attention, which is critical for avoiding vision loss.
- Seek Immediate Medical Attention: If you have sudden vision loss or other GCA symptoms, seek medical attention right away. Early diagnosis and corticosteroid treatment can help to prevent further vision loss and complications.
- Follow Treatment Plans: If diagnosed with GCA, strictly adhere to the prescribed treatment regimen. To manage inflammation and prevent AAION, medications must be used consistently and follow-up visits should be scheduled on a regular basis.
- Regular Eye Examinations: Regular comprehensive eye exams can detect changes in the optic nerve and other eye structures early on, allowing for timely intervention.
- Support Networks: Join support groups and organizations dedicated to GCA and AAION. These groups can offer valuable resources, emotional support, and information on the most recent research and treatment options.
- Healthy Diet: Eat anti-inflammatory foods like fruits, vegetables, whole grains, and lean protein. Reducing dietary inflammation can improve overall vascular health.
- Stay Informed About Research: Stay current on the latest research and advances in the treatment of GCA and AAION. Being informed allows you to advocate for the best possible care and treatment options.
Diagnostic methods
Arteritic anterior ischemic optic neuropathy (AAION) is diagnosed using a combination of clinical evaluation, imaging techniques, and laboratory tests to confirm the presence of giant cell arteritis (GCA) and determine the extent of optic nerve damage.
Standard Diagnostic Techniques
- Clinical Examination: The first step in diagnosing AAION is a thorough eye examination and a detailed patient history. Symptoms such as sudden vision loss, headache, scalp tenderness, and jaw claudication should be thoroughly investigated.
- Visual Acuity Test: This test determines the clarity of vision in each eye. Significant vision loss in one eye, often accompanied by other GCA symptoms, may indicate AAION.
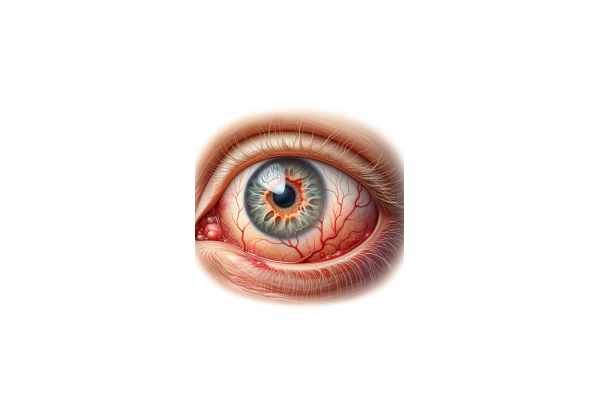
- Fundus Examination: The ophthalmologist examines the back of the eye with an ophthalmoscope, focusing on the optic disc. AAION is characterized by a pale, swollen optic disc (disc edema) due to ischemia.
- Fluorescein Angiography: This imaging technique involves injecting a fluorescent dye into the bloodstream to enable visualization of the retinal blood vessels. It aids in detecting perfusion defects in the optic nerve head and other retinal abnormalities.
- Intraocular Pressure Measurement: Elevated intraocular pressure may indicate glaucoma, which is a possible complication of AAION. Tonometry measures the pressure inside the eye.
Lab Tests
- Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP): These blood tests detect the presence of inflammation in the body. Elevated ESR and CRP levels are common in GCA and AAION patients.
- Complete Blood Count (CBC): This test can identify anemia and other hematological abnormalities linked to systemic inflammation.
- Temporal Artery Biopsy: The gold standard for detecting GCA. A small section of the temporal artery is surgically removed and examined under a microscope for evidence of inflammation and giant cells. A positive biopsy confirms GCA and supports the diagnosis of AAION.
Innovative Diagnostic Techniques
- Optical Coherence Tomography (OCT): OCT can produce high-resolution cross-sectional images of the retina and optic nerve head. It aids in the detection of structural changes, such as optic disc edema and retinal nerve fiber layer thinning, which are signs of AAION.
- Doppler Ultrasound: This noninvasive imaging technique assesses blood flow in the temporal arteries. Reduced or absent blood flow may indicate arterial occlusion due to GCA.
- Positron Emission Tomography (PET): PET scanning can detect inflammatory activity in arteries throughout the body, including the temporal arteries, giving a complete picture of the extent of GCA.
- Magnetic Resonance Imaging (MRI) and Magnetic Resonance Angiography (MRA): These imaging techniques can see through blood vessels and detect inflammation, stenosis, or occlusion of the arteries that supply the optic nerve.
Using a combination of these diagnostic methods, healthcare providers can accurately diagnose AAION, assess its severity, and initiate appropriate treatment to prevent further vision loss and systemic complications.
Treatment
Standard Treatments
- Corticosteroids: High-dose corticosteroids are the primary treatment for AAION and GCA. Immediate corticosteroid administration, such as prednisone or methylprednisolone, is critical to preventing further vision loss and reducing inflammation. The dosage is typically high at first and gradually reduced based on clinical response and inflammatory markers (ESR and CRP).
- Aspirin: Low-dose aspirin is frequently used as an adjunct therapy to reduce the risk of thrombotic events, such as stroke, associated with GCA.
- Calcium and Vitamin D Supplements: Long-term corticosteroid use may result in bone loss. Calcium and vitamin D supplements can help reduce this side effect and promote bone health.
Innovative and Emerging Therapies
- Biologic Agents: Tocilizumab, an interleukin-6 (IL-6) receptor antagonist, is emerging as a promising treatment for GCA. It reduces inflammation and has demonstrated efficacy in reducing the need for corticosteroids. Other biologic agents targeting various inflammatory pathways are also being investigated.
- Methotrexate and Other Immunosuppressants: Steroid-sparing agents include methotrexate and other immunosuppressive medications like azathioprine and mycophenolate mofetil. They help to keep the disease in remission while reducing corticosteroid side effects.
- Antiplatelet and Anticoagulant Therapy: In addition to aspirin, patients with GCA may benefit from other antiplatelet or anticoagulant medications to reduce the risk of thrombotic complications.
- Monitoring and Adjusting Therapy: Regular follow-up visits are required to assess the patient’s response to treatment, adjust medication dosages, and manage any side effects. Monitoring inflammatory markers (ESR and CRP) can help guide treatment adjustments.
Supportive Care
- Vision Rehabilitation: For patients who have suffered significant vision loss, vision rehabilitation services can help optimize remaining vision and improve overall quality of life. This could include low-vision aids, occupational therapy, and adaptive techniques.
- Lifestyle Modifications: Patients are encouraged to live a healthy lifestyle to improve their overall vascular health. This includes a healthy diet, regular exercise, quitting smoking, and managing other cardiovascular risk factors like hypertension and diabetes.
- Patient Education and Support: Educating patients about the symptoms of GCA and the importance of following treatment plans is critical. Support groups and counseling can offer emotional support and resources for dealing with vision loss and the difficulties of living with a chronic illness.
Integrating these standard and emerging treatments allows healthcare providers to effectively manage AAION, reduce inflammation, and prevent further complications, improving patient outcomes and preserving vision.
Trusted Resources
Books
- “Neuro-Ophthalmology Illustrated” by Valerie Biousse and Nancy J. Newman
- “Giant Cell Arteritis: Diagnosis and Management” by Bhaskar Dasgupta and Raashid Luqmani
- “Principles and Practice of Ophthalmology” by Daniel M. Albert and Frederick A. Jakobiec






