What is Birdshot Chorioretinopathy?
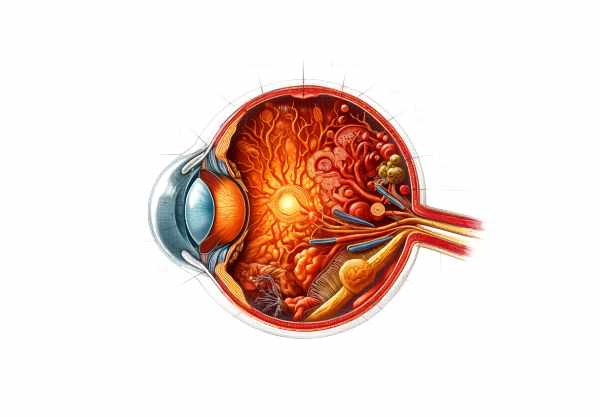
Birdshot chorioretinopathy, also called birdshot retinochoroidopathy or birdshot uveitis, is a rare, chronic, and potentially blinding autoimmune inflammatory disease that affects the retina and choroid of the eye. It is named after the characteristic appearance of scattered, light-colored spots on the retina that resemble birdshot from a shotgun. This condition primarily affects middle-aged Caucasians and is strongly linked to the HLA-A29 genetic marker. Birdshot chorioretinopathy can cause progressive vision loss if not managed properly, so early detection and treatment are critical for maintaining visual function.
Birdshot Chorioretinopathy Insights
Birdshot chorioretinopathy is an autoimmune disorder in which the immune system mistakenly attacks the retina and choroid, resulting in chronic inflammation. The condition’s exact cause is unknown, but it is thought to be a combination of genetic and environmental factors. The strong association with the HLA-A29 genetic marker indicates a genetic predisposition, whereas environmental triggers, such as infections, may start the inflammatory process.
Pathophysiology
The pathophysiology of birdshot chorioretinopathy is characterized by an autoimmune response that targets specific antigens in the retina and choroid. The inflammation primarily affects the choroidal blood vessels and the retinal pigment epithelium. Over time, this inflammation can damage the photoreceptors and other retinal structures, resulting in progressive vision loss.
Clinical Features
Birdshot chorioretinopathy is characterized by a variety of ocular symptoms that can be severe and progressive. Common clinical characteristics include:
- Blurry Vision: Patients frequently experience gradual blurring of vision, which can impair both near and distant vision.
- Floaters: The presence of floaters, or small moving spots in the field of vision, is common and caused by inflammation in the vitreous humor.
- Night Blindness: Difficulty seeing in low light, also known as nyctalopia, is a common symptom caused by rod photoreceptor loss.
- Photopsia: Patients may experience flashes of light or visual disturbances, which indicate retinal involvement.
- Color Vision Deficiency: Changes in color perception, particularly difficulty distinguishing between specific colors, can occur as the disease progresses.
- Peripheral Vision Loss: Visual field constriction, which causes peripheral vision loss, is common and can have a significant impact on daily activities.
Ophthalmic findings
Birdshot chorioretinopathy is characterized by several clinical findings:
- Birdshot Lesions: The condition is distinguished by the presence of numerous cream-colored lesions scattered throughout the retina, particularly in the posterior pole. These lesions are typically round or oval in shape and can vary in size.
- Retinal Vasculitis: Inflammation of the retinal blood vessels can occur, resulting in vessel sheathing and leakage.
- Cystoid Macular Edema (CME): Swelling of the macula caused by fluid accumulation is a common complication that can severely impair central vision.
- Vitritis: Inflammation of the vitreous humor, also known as vitritis, can result in the presence of cells and haze, which can cause visual disturbances.
- Optic Disc Edema: Swelling of the optic nerve head can occur in some cases, indicating more severe inflammation.
Genetic Predisposition
The strong link between birdshot chorioretinopathy and the HLA-A29 genetic marker indicates a genetic predisposition to the disease. HLA-A29 is a type of human leukocyte antigen (HLA) that regulates the immune response. Almost all people with birdshot chorioretinopathy are HLA-A29 positive, making it one of the most powerful genetic associations with an autoimmune disease. However, not all HLA-A29 positive individuals will develop birdshot chorioretinopathy, implying that other genetic and environmental factors influence disease progression.
Differential Diagnosis
Several other conditions can present with similar clinical features to birdshot chorioretinopathy, so differential diagnosis is critical. These conditions include the following:
- Sarcoidosis is an inflammatory disease that can affect several organs, including the eyes, causing uveitis and retinal vasculitis. Sarcoidosis can cause similar retinal lesions, but it usually manifests with systemic symptoms like lung involvement.
- Multiple Evanescent White Dot Syndrome (MEWDS): A condition marked by the presence of multiple white spots in the retina, which is frequently associated with a viral prodrome. Unlike birdshot chorioretinopathy, MEWDS typically affects young people and has a self-limiting course.
- Acute Posterior Multifocal Placoid Pigment Epitheliopathy (APMPPE) is an inflammatory condition characterized by the sudden appearance of yellowish-white retinal lesions. APMPPE is often associated with a viral illness and can resolve on its own, as opposed to birdshot chorioretinopathy, which is chronic.
- Vogt-Koyanagi-Harada (VKH) Syndrome is an autoimmune disease of the eyes, skin, and central nervous system. VKH can result in bilateral uveitis and retinal detachment, but it is frequently accompanied by systemic symptoms such as hearing loss and skin changes.
- Tuberculosis-Associated Uveitis: Tuberculosis infection can cause uveitis that looks like vasculitis and retinal lesions. A thorough evaluation for systemic tuberculosis is required to distinguish it from birdshot chorioretinopathy.
Progress and Prognosis
Birdshot chorioretinopathy is a chronic, progressive disease that goes through periods of exacerbation and remission. The rate of progression varies between individuals, with some experiencing rapid vision deterioration and others taking a more leisurely approach. The prognosis for visual outcomes is determined by the severity of retinal damage and the efficacy of treatment in controlling inflammation.
Early diagnosis and treatment are critical for preserving vision and avoiding irreversible retinal damage. Regular follow-up and monitoring are required to detect disease activity and adjust treatment accordingly. With proper care, many patients can maintain functional vision and live active lives.
Essential Preventive Tips
- Regular Eye Exams: Schedule routine comprehensive eye exams with an ophthalmologist to detect early signs of birdshot chorioretinopathy and track disease progression. Early detection can help manage symptoms and protect vision.
- Protective Eyewear: Wear sunglasses with UV protection to protect your eyes from harmful ultraviolet rays, which can worsen retinal damage and inflammation.
- Healthy Diet: Eat a well-balanced diet high in antioxidants, vitamins, and minerals to promote overall eye health. Fish and leafy green vegetables are good sources of omega-3 fatty acids.
- Don’t Smoke: Smoking can hasten the progression of retinal diseases. Avoiding tobacco smoke is critical for maintaining vision and reducing inflammation.
- Manage Systemic Health: Manage systemic conditions like hypertension, diabetes, and hyperlipidemia, which can harm retinal health and worsen ocular inflammation.
- Stress Management: Use stress-reduction techniques like yoga, meditation, and deep breathing exercises to help manage stress, which can have an impact on overall health and potentially cause disease flares.
- Stay Informed: Learn more about birdshot chorioretinopathy and its associated risks. Staying informed can help you make better decisions about your eye health and seek medical attention as needed.
- Multidisciplinary Care: Collaborate with a team of healthcare providers, including ophthalmologists, rheumatologists, and immunologists, to provide comprehensive care and management for both the ocular and systemic aspects of birdshot chorioretinopathy.
- Regular Health Screenings: Get regular health screenings to detect and treat any underlying systemic conditions that could worsen birdshot chorioretinopathy. Early detection and treatment of these conditions can improve outcomes while decreasing the risk of ocular complications.
- Avoid Self-Medication: Do not self-medicate or use over-the-counter eye drops without first consulting a healthcare professional, as improper use can exacerbate symptoms or lead to additional complications. Always follow your doctor’s recommendations for treatment and medication.
Diagnostic methods
Birdshot chorioretinopathy is diagnosed using a combination of clinical evaluation, imaging techniques, and genetic testing to confirm the condition’s presence and severity.
Clinical Evaluation
The first step in diagnosing birdshot chorioretinopathy is a thorough eye examination by an ophthalmologist. This includes taking a thorough patient history to identify symptoms like blurred vision, floaters, night blindness, and changes in color vision. Visual acuity tests are used to determine the level of vision impairment.
Fundus Examination
A fundus examination with an ophthalmoscope allows the ophthalmologist to see the retina and the choroid. Birdshot chorioretinopathy is characterized by multiple cream-colored spots scattered across the retina. These lesions are commonly found in the posterior pole and can range in size and shape.
Fluorescein Angiography(FA)
Fluorescein angiography (FA) is an important diagnostic tool that involves injecting a fluorescent dye into the bloodstream and taking multiple photographs of the retina. FA can reveal areas of retinal vasculitis, vessel leakage, and the severity of cystoid macular edema. This imaging technique aids in determining the severity of inflammation and informing treatment decisions.
Indocyanine green angiography (ICGA)
Indocyanine green angiography (ICGA) is a technique for visualizing choroidal circulation. This technique can identify abnormalities in the choroidal vasculature, such as hypoperfusion and leakage, which are common in birdshot chorioretinopathy. The ICGA method provides additional information about choroidal involvement and aids in distinguishing birdshot lesions from other similar conditions.
Optical Coherence Tomography(OCT)
Optical coherence tomography (OCT) is a noninvasive imaging technique that produces high-resolution cross-sectional images of the retina. OCT is used to detect retinal thickening, subretinal fluid, and cystoid macular edema (CME). This technique is extremely useful for tracking disease progression and response to treatment.
Electroretinography (ERG)
Electroretinography (ERG) measures the retina’s electrical responses to light stimuli. In birdshot chorioretinopathy, ERG responses are typically reduced, indicating photoreceptor and RPE dysfunction. This test is especially useful for determining the functional impact of the disease on the retina.
Genetic Testing
Genetic testing for the HLA-A29 marker can help with the diagnosis of birdshot chorioretinopathy. Almost all patients with birdshot chorioretinopathy have HLA-A29, making it a reliable diagnostic marker. This test can help to confirm the diagnosis and distinguish birdshot chorioretinopathy from other uveitis conditions.
Birdshot Chorioretinopathy Treatments
The treatment for birdshot chorioretinopathy focuses on reducing inflammation, preventing disease progression, and maintaining vision. A multidisciplinary approach with ophthalmologists and rheumatologists is frequently required.
Corticosteroids
Corticosteroids are the standard treatment for acute inflammation in birdshot chorioretinopathy. They can be given orally, intravenously, or as periocular injections. High-dose corticosteroids are typically used first to reduce inflammation quickly, followed by a tapering period to minimize side effects. Long-term corticosteroid use is associated with serious side effects such as increased intraocular pressure, cataracts, and systemic complications, necessitating close monitoring.
Immunosuppressive Agents
Methotrexate, azathioprine, and cyclosporine are examples of immunosuppressive agents that are commonly used as steroid-free treatments for chronic inflammation. These medications help to regulate the immune response, reducing the frequency and severity of disease flares. Regular monitoring for possible side effects, such as liver toxicity and bone marrow suppression, is required.
Biological Therapies
Biologic therapies represent a significant advancement in the treatment of birdshot chorioretinopathy. Tumor necrosis factor (TNF) inhibitors like infliximab and adalimumab, as well as interleukin inhibitors like tocilizumab, have been shown to be effective in treating severe and refractory inflammation. These agents target specific components of the inflammatory process, providing better results with potentially fewer side effects than traditional immunosuppressive drugs.
Intravitreal Injections
Cystoid macular edema (CME) and retinal vasculitis can be treated with intravitreal injections of corticosteroids or anti-VEGF (vascular endothelial growth factor) agents such as bevacizumab (Avastin) and ranibizumab (Lucentis). These injections deliver high concentrations of medication directly to the affected area, resulting in quick and precise relief.
Laser Photocoagulation
Laser photocoagulation is a targeted treatment that uses laser energy to seal leaking blood vessels and prevent retinal detachments. This procedure may help stabilize vision and prevent further deterioration in patients with birdshot chorioretinopathy. Laser photocoagulation is frequently used in conjunction with other treatments to achieve the best results.
Emerging and Innovative Therapeutics
Immunotherapy
Immunotherapy, which includes checkpoint inhibitors and adoptive cell transfer, is an emerging treatment option for a variety of autoimmune diseases. Immunotherapy, which boosts the body’s immune response to inflammatory cells, may help control the underlying immune dysregulation in birdshot chorioretinopathy. Clinical trials are currently underway to determine the efficacy of these treatments in birdshot chorioretinopathy.
Genetic Therapy
Gene therapy is a novel approach that seeks to correct genetic defects and alter disease pathways at the molecular level. While still in the experimental stages, gene therapy has the potential to treat birdshot chorioretinopathy by targeting the genetic and molecular mechanisms that cause inflammation. Future research may shed new light on the use of gene therapy for birdshot chorioretinopathy.
Stem Cell Therapy
Stem cell therapy is another novel approach being studied for the treatment of retinal degeneration. Researchers hope to restore vision by transplanting healthy retinal cells derived from stem cells into damaged retinas. Early-stage clinical trials are currently underway to determine the safety and efficacy of this approach in birdshot chorioretinopathy.
Trusted Resources
Books
- “Retinal Degenerations: Biology, Diagnostics, and Therapeutics” by Matthew M. LaVail, Joe G. Hollyfield, and Robert E. Anderson
- “Clinical Ophthalmic Oncology: Uveal Tumors” by Arun D. Singh and Bertil Damato
- “Ocular Disease: Mechanisms and Management” by Leonard A. Levin, James Ver Hoeve, Samuel Wu, and David L. Kaufman
Online Resources
- National Eye Institute: https://www.nei.nih.gov
- American Academy of Ophthalmology: https://www.aao.org
- Birdshot Uveitis Society: https://www.birdshot.org.uk
- Orphanet: https://www.orpha.net










