What is Branch Retinal Artery Occlusion?
Branch retinal artery occlusion (BRAO) occurs when one of the smaller branches of the central retinal artery becomes blocked, resulting in a sudden loss of vision in the area supplied by the affected artery. This blockage obstructs blood flow to the retina, causing ischemia and potentially leading to permanent vision loss if not treated promptly. BRAO is classified as an ocular emergency and frequently indicates underlying systemic vascular or thromboembolic conditions that necessitate a thorough medical evaluation and management. Understanding the mechanisms, risk factors, and consequences of BRAO is critical for both patients and healthcare professionals.
Exploring Branch Retinal Artery Occlusion
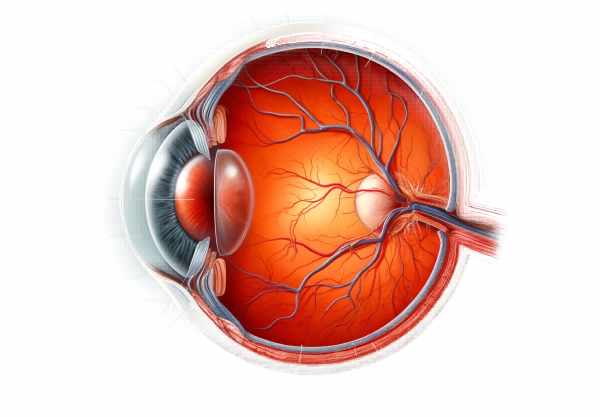
Branch retinal artery occlusion occurs when one of the branches of the central retinal artery, which supplies blood to the retina, becomes clogged. The retina is the light-sensitive layer at the back of the eye that converts light into neural signals, which are then transmitted to the brain to form visual images. The retina requires adequate blood flow to function and survive.
Pathophysiology
The pathophysiology of BRAO involves a sudden interruption of blood flow to a segment of the retina, which causes ischemia and hypoxia of the retinal tissues. This interruption is usually caused by emboli, which can come from a variety of sources:
- Embolic Sources: Emboli can come from the heart (cardiogenic emboli), the carotid arteries (carotid emboli), or even the retina itself. These emboli can be made of cholesterol (Hollenhorst plaques), calcified material, or platelet fibrin.
- Atherosclerosis: Atherosclerotic plaques in the carotid arteries can dislodge and migrate to the retinal arteries, resulting in occlusion. These plaques are made up of cholesterol and other substances that can constrict or block arteries.
- Cardiogenic Emboli: Conditions such as atrial fibrillation, endocarditis, or valvular heart disease can cause emboli to travel through the bloodstream and obstruct retinal arteries.
- Hypercoagulable States: Conditions that increase the likelihood of blood clotting, such as antiphospholipid syndrome, factor V Leiden mutation, or hyperhomocysteinemia, can cause BRAO.
Clinical Presentation
Patients with BRAO usually present with a sudden, painless vision loss in one eye. The extent of vision loss is determined by the occluded artery’s location and diameter. The key symptoms and signs are:
- Sudden Vision Loss: The main symptom is a sharp decrease in vision in one eye. The vision loss corresponds to the portion of the retina supplied by the occluded artery.
- Scotoma: Patients may detect a dark or blind spot (scotoma) in their visual field. The scotoma’s size and location are determined by the affected area of the retina.
- Fundoscopic Findings: If the central retinal artery is involved, the affected retina may appear edematous and pale, with a cherry-red spot at the macula. Emboli may be visible in the retinal arteries.
Risk Factors
Several risk factors raise the chances of developing BRAO:
- Age: BRAO primarily affects older adults, usually over the age of 60.
- Hypertension: High blood pressure is a major risk factor for the development of atherosclerosis.
- Diabetes Mellitus: Diabetes raises the risk of vascular diseases like BRAO.
- Hyperlipidemia: High cholesterol levels promote the formation of atherosclerotic plaques.
- Cardiovascular Diseases: Conditions like atrial fibrillation, valvular heart disease, and carotid artery stenosis raise the risk of embolic events.
- Smoking: Smoking significantly increases the risk of atherosclerosis and other vascular diseases.
- Hypercoagulable States: BRAO can result from genetic or acquired conditions that cause excessive blood clotting.
Complications
If not treated promptly, BRAO can cause a number of complications:
- Permanent Vision Loss: Prolonged ischemia can irreversibly damage retinal cells, resulting in permanent vision loss in the affected area.
- Neovascularization: Chronic ischemia can promote the formation of new, abnormal blood vessels (neovascularization), which can lead to additional complications like vitreous hemorrhage or retinal detachment.
- Secondary Glaucoma: Neovascularization can cause high intraocular pressure and secondary glaucoma, which can further impair vision.
Differential Diagnosis
When a patient presents with sudden vision loss, it is important to consider other possible causes:
- Central Retinal Artery Occlusion (CRAO): Similar to BRAO, but affects the central retinal artery, resulting in more extensive vision loss.
- Retinal Vein Occlusion (RVO): Blockage of the retinal veins can result in vision loss, but it is usually accompanied by retinal hemorrhages and dilated veins.
- Anterior Ischemic Optic Neuropathy (AION): Caused by ischemia of the optic nerve head, which results in sudden vision loss and optic disc swelling.
- Giant Cell Arteritis (GCA): An inflammatory condition that causes occlusion of the arteries that supply the optic nerve, resulting in vision loss.
Prognosis
The prognosis for BRAO depends on the severity and duration of the occlusion, as well as the timing of treatment. In some cases, spontaneous reperfusion can occur, resulting in a partial recovery of vision. However, significant and prolonged occlusion can lead to permanent vision loss.
Research to improve the outcomes of BRAO patients is ongoing, with a focus on understanding the mechanisms of retinal ischemia and developing new therapeutic approaches. Advances in imaging techniques, such as optical coherence tomography angiography (OCTA), improve our ability to diagnose and monitor BRAO, potentially leading to better outcomes through early detection and treatment.
Essential Preventive Measures
- Manage Blood Pressure: Maintain healthy blood pressure levels with regular monitoring and treatment. Hypertension is a major risk factor for BRAO, and controlling it can help reduce the likelihood of vascular occlusions.
- Control Blood Sugar Levels: For diabetics, maintaining good glycemic control is critical. Regular blood sugar monitoring and adherence to prescribed medications can help prevent vascular complications like BRAO.
- Lower Cholesterol: Follow a heart-healthy diet low in saturated fat and cholesterol. Statins may be prescribed to help manage cholesterol levels and lower the risk of atherosclerosis.
- Stop Smoking: Quitting smoking is one of the most effective ways to improve overall cardiovascular health. Seek help from cessation programs, counseling, or medications to quit smoking.
- Exercise Regularly: Regular physical activity can help improve cardiovascular health. Aim for 30 minutes of moderate exercise most days of the week.
- Healthy Diet: Eat a balanced diet high in fruits, vegetables, whole grains, and lean proteins. A diet rich in antioxidants and omega-3 fatty acids can help improve vascular health.
- Regular Health Check-Ups: Routine medical examinations can aid in the detection and management of BRAO risk factors. Screenings for hypertension, diabetes, and hyperlipidemia are critical for timely intervention.
- Manage Cardiovascular Conditions: If you have underlying cardiovascular diseases, such as atrial fibrillation or valvular heart disease, make sure they are properly treated and monitored on a regular basis.
- Anticoagulation Therapy: Individuals with hypercoagulable states or certain cardiovascular conditions may benefit from anticoagulation therapy to reduce the risk of thromboembolic events.
- Educate and Inform: Being aware of the symptoms and risk factors of BRAO is critical. Educate yourself and others on the significance of vascular health and the need for immediate medical attention in the event of sudden vision loss.
Diagnostic methods
Branch Retinal Artery Occlusion (BRAO) is diagnosed using a combination of clinical examination and advanced imaging techniques to determine the extent of retinal damage.
Clinical Examination
- Visual Acuity Test: This simple test assesses the clarity and sharpness of vision in each eye. Patients with BRAO frequently present with acute vision loss in one eye, which is detected during this test.
- Fundus Examination: The eye doctor uses an ophthalmoscope to examine the back of the eye, with a focus on the retina. A pale retina in the area supplied by the occluded artery, as well as a visible embolus, are common findings during this examination.
Imaging Techniques
- Fluorescein Angiography (FA): This procedure involves injecting a fluorescent dye into the bloodstream and photographing the retina. This technique focuses on blood flow within the retinal vessels, which aids in the identification of blockages and areas of ischemia.
- Optical Coherence Tomography (OCT): OCT can generate high-resolution cross-sectional images of the retina. It assesses the thickness of the retinal layers and detects swelling or thinning, which are signs of ischemia and subsequent retinal damage.
- Optical Coherence Tomography Angiography (OCTA): OCTA is a non-invasive imaging technique that produces detailed images of the retinal blood vessels without requiring dye injection. It allows for the visualization of blood flow and aids in the detection of capillary dropout or abnormal vessel growth.
Additional Diagnostic Tests
- Carotid Doppler Ultrasound: This ultrasound test measures blood flow through the carotid arteries. It aids in the detection of atherosclerosis or plaques that may dislodge and cause emboli, ultimately leading to BRAO.
- Echocardiography: This test uses ultrasound to produce images of the heart. It aids in the identification of potential emboli sources, such as valvular heart disease and atrial fibrillation.
- Blood Tests: Blood tests can reveal systemic conditions that heighten the risk of BRAO. These could include tests for cholesterol, blood sugar, clotting disorders, and inflammatory markers.
- Electrocardiogram (ECG): An ECG measures the electrical activity of the heart. It aids in the detection of arrhythmias like atrial fibrillation, which can lead to emboli.
Genetic Testing
In some cases, genetic testing may be necessary to identify inherited conditions that predispose people to hypercoagulability or vascular abnormalities. This is especially useful for young patients who have no known risk factors for BRAO.
Branch Retinal Artery Occlusion Treatments
The primary goal of treating BRAO is to restore blood flow to the retina as soon as possible in order to limit retinal damage and preserve vision. The treatment approach is determined by the severity of the occlusion and the underlying cause.
Immediate interventions
- Ocular Massage: A gentle massage of the eyeball may dislodge the embolus, allowing it to move downstream and restore blood flow. This technique is frequently used in an emergency situation.
- Anterior Chamber Paracentesis: This procedure removes a small amount of fluid from the anterior chamber of the eye to reduce intraocular pressure. The decrease in pressure may aid in dislodging the embolus and restoring retinal blood flow.
Medications
- Antiplatelet Agents: Aspirin and clopidogrel are commonly prescribed to reduce the risk of future embolic events by preventing platelet aggregation.
- Anticoagulants: Patients at high risk of thromboembolic events, such as those with atrial fibrillation, may be prescribed warfarin or direct oral anticoagulants (DOACs) to prevent blood clot formation.
- Intra-Arterial Thrombolysis: In certain cases, thrombolytic agents (clot-busting drugs) can be administered directly into the retinal artery to dissolve the embolus. This treatment is time-sensitive and risky, so it is usually reserved for severe cases.
Long-Term Management
- Control of Underlying Conditions: Managing risk factors like hypertension, diabetes, and hyperlipidemia is critical for avoiding recurrence. This includes lifestyle changes like eating a healthy diet, exercising regularly, and quitting smoking, as well as taking the right medications.
- Regular Monitoring: Patients with BRAO should schedule regular follow-up appointments with their ophthalmologist to monitor retinal health and visual function. This includes regular imaging to monitor retinal blood flow and detect new or recurring occlusions.
Innovative and Emerging Therapies
- Hyperbaric Oxygen Therapy (HBOT): HBOT consists of breathing pure oxygen in a pressurized chamber. It has shown promise in improving oxygen delivery to ischemic retinal tissues, which may aid in the recovery of retinal function.
- Neuroprotective Agents: Researchers are looking into neuroprotective agents that can protect retinal cells from ischemic damage. These agents are intended to reduce cell death and improve visual outcomes in BRAO patients.
- Retinal Implants: For patients with severe vision loss, retinal implants or prosthetic devices are being developed to restore some level of vision. These devices are still experimental, but they provide hope for future treatment options.
- Gene Therapy: Advances in gene therapy show promise for treating underlying genetic causes of vascular occlusions. Gene therapy, by correcting genetic defects, has the potential to prevent BRAO from recurring in patients with inherited predispositions.
Trusted Resources
Books
- “Retinal Vascular Disease” by A.M. Joussen, T.W. Gardner, B. Kirchhof, and S.J. Ryan
- “Retinal Vein Occlusion: Evidence-Based Management” by Ingrid U. Scott, Sharon Fekrat, and F. Michael Michael
Online Resources
- American Academy of Ophthalmology: https://www.aao.org
- National Eye Institute: https://www.nei.nih.gov
- Retina Society: https://www.retinasociety.org
- National Institutes of Health: https://www.nih.gov










