Introduction
Non-infectious endophthalmitis is an inflammatory condition that affects the inside of the eye, specifically the vitreous and aqueous humors. Non-infectious endophthalmitis, as opposed to infectious endophthalmitis, is caused by an autoimmune reaction, trauma, or surgery, rather than bacterial, fungal, or viral pathogens. If not treated promptly and effectively, this condition can lead to significant vision impairment.
Patients with non-infectious endophthalmitis typically experience eye pain, redness, blurred vision, and light sensitivity. Although the severity of these symptoms varies, untreated inflammation can cause permanent damage to ocular structures. Non-infectious endophthalmitis pathophysiology is characterized by an inappropriate immune response in which the body’s defense mechanisms mistakenly target ocular tissues, resulting in inflammation and damage.
A comprehensive eye examination, including slit-lamp biomicroscopy, fundus examination, and imaging studies such as optical coherence tomography (OCT) and ultrasound, is required to diagnose non-infectious endophthalmitis. These diagnostic tools can help determine the severity of inflammation and rule out infectious causes. Laboratory tests, such as blood work and aqueous or vitreous tap, may also be required to rule out infectious agents or identify underlying systemic conditions.
Understanding the causes and underlying mechanisms of non-infectious endophthalmitis is critical for developing effective treatments. Common causes include cataract surgery, intravitreal injections, and systemic autoimmune diseases like Behçet’s disease and sarcoidosis. Awareness and early detection of the condition can help to prevent serious visual outcomes and improve patient quality of life.
Standard Treatments for Non-Infectious Endophthalmitis
Non-infectious endophthalmitis management and treatment aims to reduce inflammation, preserve vision, and address any underlying conditions. Standard treatment methods include anti-inflammatory medications, immunosuppressive therapies, and supportive care.
Corticosteroid Treatment
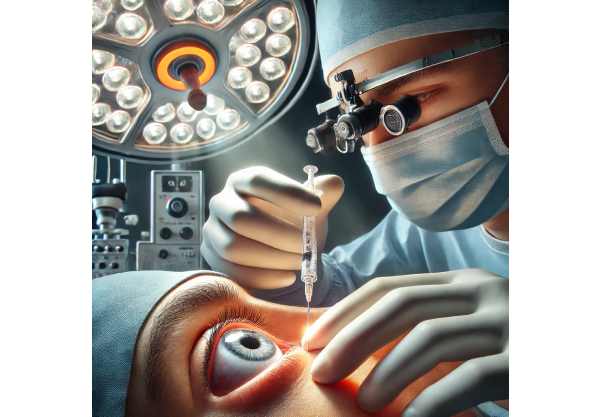
Because of their potent anti-inflammatory properties, corticosteroids are the primary treatment for non-infectious endophthalmitis. Topical eye drops, oral tablets, periocular injections, and intravitreal injections are all options for administering these medications. The method of administration is determined by the severity of the inflammation and the patient’s overall health.
Prednisolone acetate, for example, is a popular topical corticosteroid for mild to moderate inflammation. In more severe cases, periocular or intravitreal corticosteroid injections, such as triamcinolone acetonide, may be required to increase drug concentrations at the site of inflammation. Oral corticosteroids, such as prednisone, can be used in conjunction with local treatments to provide systemic anti-inflammatory benefits.
Immunosuppressive Therapy
Immunosuppressive agents are considered when corticosteroids alone are insufficient or not tolerated. These medications help to regulate the immune response and reduce inflammation. Methotrexate, azathioprine, mycophenolate mofetil, and cyclosporine are all commonly used immunosuppressive agents.
Methotrexate, a folate antagonist, effectively reduces inflammation by inhibiting immune cell proliferation. Azathioprine and mycophenolate mofetil suppress immune cell production and thus reduce the immune response. Cyclosporine, a calcineurin inhibitor, prevents T-lymphocyte activation, which reduces inflammation. These agents are frequently used in conjunction with corticosteroids to increase their efficacy and allow for lower corticosteroid doses, reducing potential side effects.
Biological Agents
Biologic agents are a newer class of medications that target specific immune system components that cause inflammation. These medications have shown promise in treating a variety of autoimmune and inflammatory diseases, including non-infectious endophthalmitis. Adalimumab, infliximab, and rituximab are some examples of biologic agents used in this context.
Adalimumab and infliximab are tumor necrosis factor (TNF) inhibitors that inhibit the action of TNF, a cytokine that plays an important role in inflammation. By inhibiting TNF, these agents help to reduce inflammation and prevent tissue damage. Rituximab, a monoclonal antibody that targets CD20-positive B cells, reduces inflammation by depleting B cells that are involved in the immune response.
Supportive Care and Monitoring
Supportive care is an important part of treating non-infectious endophthalmitis. Patients may require additional treatments to alleviate specific symptoms and complications. Nonsteroidal anti-inflammatory drugs (NSAIDs) are one example of a medication that can be used to treat inflammation-related pain. Cycloplegic agents may be prescribed to treat ciliary muscle spasms and pain.
Regular monitoring and follow-up are essential for assessing the response to treatment, adjusting medications as needed, and detecting any signs of relapse or complications. Follow-up appointments with an ophthalmologist usually include visual acuity testing, a slit-lamp examination, and imaging studies like OCT to assess the extent of inflammation and monitor ocular structures.
Cutting-Edge Innovations in Non-infectious Endophthalmitis Treatment
Advances in understanding non-infectious endophthalmitis, as well as the development of novel treatment strategies, have significantly improved the condition’s management. These cutting-edge treatments aim to provide more targeted and effective therapies, lower the risk of complications, and improve patients’ outcomes.
Intravenous Implants
One of the most promising advances in the treatment of non-infectious endophthalmitis is the use of intravitreal implants. These implants continuously deliver corticosteroids or other anti-inflammatory medications into the vitreous cavity. The sustained-release formulation ensures consistent drug delivery, which reduces the need for frequent injections and improves patient compliance.
Ozurdex (Dexamethasone Intravitreal Implant) is a biodegradable implant that gradually releases dexamethasone. Clinical trials have shown that it can reduce inflammation and improve visual outcomes in patients with non-infectious uveitis, which is closely related to non-infectious endophthalmitis. The implant is placed in the vitreous cavity using a minimally invasive procedure and gradually dissolves over time, providing long-term anti-inflammatory benefits.
Biological Agents and Targeted Therapies
The introduction of biologic agents and targeted therapies has transformed the treatment of autoimmune and inflammatory diseases, including non-infectious endophthalmitis. These therapies target specific molecules involved in the inflammatory process, resulting in more precise and effective treatments with fewer side effects.
Interleukin-6 (IL-6) inhibitors, including tocilizumab, have shown promise in treating non-infectious endophthalmitis. IL-6 is a cytokine that plays a critical role in the inflammatory response, and inhibiting it can help reduce inflammation and tissue damage. Clinical trials are currently underway to assess the safety and efficacy of IL-6 inhibitors in patients with noninfectious uveitis and endophthalmitis.
Janus kinase (JAK) inhibitors are another type of targeted therapy that has received attention for its potential to treat noninfectious endophthalmitis. JAK inhibitors, such as tofacitinib, inhibit the JAK-STAT signaling pathway, which is involved in immune response. JAK inhibitors, by inhibiting this pathway, can reduce inflammation and prevent ocular damage progression. Early-phase clinical trials have yielded promising results, and additional research is underway to determine their role in the treatment of non-infectious endophthalmitis.
Genetic Therapy
Gene therapy is a developing field that has the potential to transform the treatment of genetic and acquired ocular conditions, such as non-infectious endophthalmitis. This method involves delivering specific genes or genetic material to specific cells in order to correct underlying genetic defects or modulate immune responses.
Recent advances in gene therapy have demonstrated promise in experimental models of autoimmune and inflammatory eye disease. Researchers are investigating the use of adeno-associated virus (AAV) vectors to deliver anti-inflammatory genes directly to ocular tissues. These vectors can deliver genes that encode anti-inflammatory proteins, reducing inflammation and protecting ocular structures.
While gene therapy for non-infectious endophthalmitis is still in its early stages of development, initial findings are promising. Ongoing clinical trials aim to assess the safety and efficacy of these novel approaches, with the goal of providing long-term solutions for patients with refractory or recurrent inflammation.
Stem Cell Therapy
Stem cell therapy is another cutting-edge innovation that has the potential to regenerate damaged ocular tissues and restore sight. This method involves transplanting stem cells that can differentiate into retinal and immune cells, thereby assisting in the repair of inflammation-induced damage.
Mesenchymal stem cells (MSCs) have shown promise in preclinical studies by modulating immune responses, reducing inflammation, and promoting tissue repair. When transplanted into the eye, MSCs can release anti-inflammatory cytokines and growth factors, reducing inflammation and promoting ocular cell regeneration. Early-phase clinical trials are currently underway to assess the safety and efficacy of MSC therapy in patients suffering from non-infectious endophthalmitis and other inflammatory eye diseases.






