Lacrimal gland tumors are abnormal growths that originate from the tissues of the lacrimal gland—an almond-shaped structure located in the upper outer quadrant of each eye orbit. The primary role of the lacrimal gland is to produce the watery component of the tear film, essential for eye lubrication and health. When tumors develop here, they can cause not only cosmetic deformities and discomfort, but also threaten vision and orbital structure.
Types of Lacrimal Gland Tumors
- Benign Tumors
- Pleomorphic adenoma: The most common benign tumor, slow-growing, encapsulated, and generally noninvasive.
- Other benign masses: Cystic lesions, inflammatory pseudotumors, and myoepitheliomas.
- Malignant Tumors
- Adenoid cystic carcinoma: The most frequent malignant tumor, known for aggressive local invasion and perineural spread.
- Carcinoma ex pleomorphic adenoma: A malignant transformation of a pre-existing benign tumor.
- Lymphoma: Both primary and secondary, particularly in older adults.
- Others: Mucoepidermoid carcinoma, acinic cell carcinoma, and rare metastatic lesions.
Pathophysiology
Lacrimal gland tumors disrupt normal gland function. Benign tumors typically expand slowly, compressing adjacent tissues, while malignant tumors often infiltrate surrounding structures and may metastasize. The biology, histology, and genetic makeup of these tumors profoundly influence the prognosis and therapeutic approach.
Epidemiology
- Prevalence:
- Lacrimal gland tumors account for 10% of all orbital masses.
- Approximately half are benign and half malignant in adult populations.
- Pleomorphic adenoma is most common in younger to middle-aged adults; malignant tumors rise in prevalence after age 50.
- Risk Factors:
- Age over 40, particularly for malignant variants.
- Prior history of orbital irradiation or trauma (rare).
- Certain genetic syndromes and family history.
Clinical Features
- Symptoms
- Gradual, painless swelling in the upper eyelid (benign).
- Rapid, painful onset with proptosis, diplopia, or decreased vision (suggestive of malignancy).
- Globe displacement, downward and inward.
- Visible mass, fullness, or asymmetry of the eyelid.
- Occasional tearing, dry eye, or discomfort.
- Warning Signs for Malignancy
- Rapid progression (weeks to months)
- Pain, numbness, or tingling (from nerve involvement)
- Restricted eye movement
Diagnosis
- Comprehensive Eye Examination
- Imaging Studies
- CT and MRI are essential for evaluating mass size, margins, calcifications, bone involvement, and perineural invasion.
- Biopsy
- Incisional or excisional biopsy for definitive histopathologic diagnosis.
- Fine-needle aspiration is rarely used due to risk of tumor seeding in pleomorphic adenoma.
- Systemic Workup
- To rule out metastasis or lymphoma elsewhere in the body.
Practical Tips:
If you notice persistent eyelid swelling, changes in eye position, or double vision—especially with rapid progression—see an ophthalmologist promptly. Early assessment and diagnosis are critical.
Conventional and Pharmacological Therapies
While surgical removal is the cornerstone for most lacrimal gland tumors, medical therapies play a pivotal role in specific scenarios—particularly for lymphoid or inflammatory lesions, inoperable cases, or as adjuncts to surgery.
Observation and Monitoring
- Benign, Stable Masses:
- If a benign tumor is confirmed and is asymptomatic, periodic observation with imaging may be appropriate, especially in elderly or high-risk surgical patients.
- Low-Grade Lymphomas:
- Indolent lymphomas may sometimes be managed conservatively with close monitoring.
Pharmacological Approaches
- Corticosteroids:
- Used for inflammatory pseudotumors, which can mimic neoplastic growths.
- Systemic or high-dose oral steroids often lead to rapid symptom improvement.
- Immunomodulatory Agents:
- Employed in autoimmune dacryoadenitis or inflammatory syndromes associated with the lacrimal gland.
- Chemotherapy and Targeted Therapy:
- For systemic or aggressive orbital lymphomas, modern regimens (e.g., R-CHOP, monoclonal antibodies) are highly effective.
- Targeted therapies (e.g., rituximab) are tailored to the specific lymphoma subtype.
- Antibiotics:
- Rarely indicated, unless infection is confirmed.
- Radiotherapy:
- Used as a primary or adjunctive treatment in lymphomas and some carcinomas.
- Often applied after incomplete excision or for tumor recurrence.
Supportive Measures
- Artificial Tears and Ocular Lubricants:
- To counteract dry eye symptoms from gland dysfunction.
- Pain Management:
- NSAIDs or analgesics for discomfort or post-procedural pain.
When to Escalate Care
- Sudden increase in mass size, pain, vision changes, or non-response to conservative measures should prompt urgent re-evaluation and possible biopsy.
Practical Advice:
Follow your care plan closely, keep a journal of symptoms, and notify your physician about any new or changing signs. Timely adjustments can make a crucial difference in outcome.
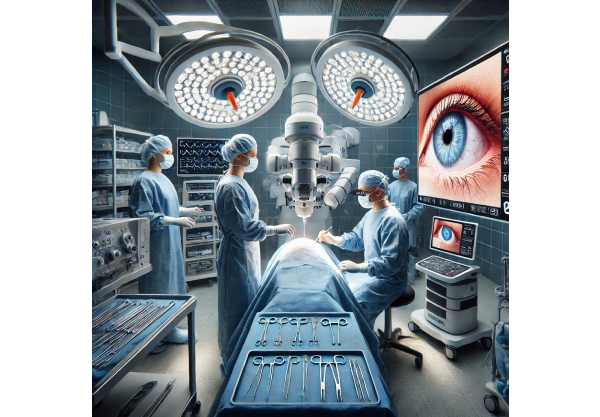
Surgical and Interventional Procedures
Surgery remains the gold standard for most lacrimal gland tumors, especially benign and localized malignant lesions. The choice of technique depends on tumor type, size, extent, and relationship to adjacent structures.
Principles of Surgical Management
- Complete Excision with Intact Capsule (Benign Tumors):
- Essential for pleomorphic adenoma to prevent recurrence and malignant transformation.
- “No-touch” technique minimizes risk of tumor spillage.
- Wide Local Excision (Malignant Tumors):
- Aim is complete removal with negative margins, sometimes requiring removal of adjacent bone or orbital tissues.
- Orbitotomy Approaches:
- Lateral Orbitotomy: The most common approach, offering direct access to the gland with minimal cosmetic deformity.
- Anterior Orbitotomy: Used for anteriorly situated lesions.
- Combined Approaches: May be necessary for large or complex tumors.
Advanced Surgical Techniques
- Image-Guided Surgery:
- Intraoperative navigation improves precision and safety, reducing risk of incomplete excision.
- Endoscopic Assistance:
- Minimally invasive, used for select anterior or small lesions.
- Reconstructive Surgery:
- Required after extensive excision to restore eyelid contour and function.
Adjuvant Procedures
- Radiation Therapy:
- For high-risk, incompletely excised, or inoperable malignancies.
- Chemotherapy:
- In aggressive carcinomas, metastatic disease, or systemic lymphomas.
- Cryotherapy:
- Occasionally used for small, superficial recurrences.
Complications and Their Management
- Recurrence:
- Higher in cases of incomplete excision or capsule violation.
- Dry Eye and Tear Deficiency:
- Result from partial or total gland removal; managed with lubricants or punctal occlusion.
- Cosmetic Deformity:
- Addressed with reconstructive eyelid and orbital procedures.
Recovery and Follow-Up
- Hospitalization:
- Most patients stay 1–2 days post-surgery.
- Postoperative Care:
- Cold compresses, antibiotics, pain control, and careful wound monitoring.
- Surveillance:
- Regular imaging and clinical evaluation, especially for malignant tumors.
Practical Tips:
- Ask your surgeon about the risks of recurrence, functional outcomes, and appearance after surgery.
- Arrange for support at home during recovery and keep scheduled follow-ups for early detection of complications.
Emerging Innovations and Advanced Technologies
The landscape of lacrimal gland tumor management is rapidly evolving, with breakthroughs in diagnostics, minimally invasive techniques, targeted therapies, and personalized care.
Diagnostic Innovations
- Molecular and Genetic Profiling:
- Next-generation sequencing enables more precise tumor characterization, guiding therapy choices and predicting outcomes.
- Liquid Biopsy:
- Detection of circulating tumor DNA for non-invasive diagnosis and monitoring of recurrence.
- AI-Assisted Imaging:
- Deep learning algorithms are increasingly used to analyze imaging, improving early detection and differentiation between benign and malignant lesions.
Therapeutic Advances
- Minimally Invasive and Robotic-Assisted Surgery:
- Smaller incisions, faster recovery, and reduced scarring.
- Robotic systems provide unmatched precision for complex orbital procedures.
- Custom 3D-Printed Implants:
- Used for orbital reconstruction, restoring anatomy and appearance after tumor resection.
- Targeted Biologic Agents:
- Monoclonal antibodies and checkpoint inhibitors for select lymphomas and carcinomas.
- Personalized immunotherapy is on the horizon for refractory or advanced cases.
Regenerative and Supportive Therapies
- Stem Cell-Based Tear Gland Regeneration:
- Preclinical studies focus on regenerating gland tissue, potentially restoring natural tear production after surgery.
- Advanced Lubricant Formulations:
- Longer-lasting and biologically active artificial tears for post-surgical dry eye.
Telemedicine and Digital Monitoring
- Virtual postoperative visits improve access, patient convenience, and adherence to follow-up care.
- Mobile applications empower patients to monitor healing and quickly report any concerning changes.
Quality of Life and Patient-Centered Care
- PROs (Patient-Reported Outcomes):
- New tools allow patients to share their experiences and goals, informing both care plans and research priorities.
Practical Advice:
- Ask about clinical trials or centers with advanced technologies.
- Don’t hesitate to inquire about less invasive options or supportive services that fit your lifestyle and personal needs.
Clinical Trials and Future Directions
Research and innovation continue to drive progress in the diagnosis and management of lacrimal gland tumors, improving outcomes for patients facing both benign and malignant disease.
Ongoing and Upcoming Clinical Trials
- Novel Systemic Therapies:
- Immunotherapy and targeted biologics for advanced and metastatic tumors.
- Radiation Modalities:
- Intensity-modulated and proton beam therapies are being studied to maximize tumor control while preserving surrounding tissue.
- Diagnostic Algorithms:
- Artificial intelligence platforms under development aim to reduce diagnostic delays and increase the accuracy of tumor characterization.
Translational Research
- Genomics and Personalized Oncology:
- Identification of actionable mutations is enabling truly individualized therapy.
- Biomarker Discovery:
- Researchers are seeking serum and tear film biomarkers to predict tumor behavior and treatment response.
Future Directions
- Integrated Multidisciplinary Care:
- Increasingly, teams of ophthalmologists, oncologists, radiologists, and reconstructive surgeons collaborate to deliver comprehensive, patient-focused care.
- Focus on Survivorship and Quality of Life:
- Rehabilitation, psychosocial support, and cosmetic outcomes are recognized as key aspects of holistic care.
- Global Access:
- Efforts are underway to make advanced diagnostics and therapies more widely available worldwide.
How Patients Can Participate
- Clinical Trial Enrollment:
- Patients with difficult-to-treat tumors may qualify for novel therapies not yet available elsewhere.
- Patient Advocacy:
- Sharing experiences, joining support networks, and engaging in advocacy can shape the future of research and care.
Practical Guidance:
- Stay informed about research and ask your providers about potential eligibility for ongoing studies.
- Share your goals and questions with your care team to ensure treatment plans align with your values.
Frequently Asked Questions
What are the most common symptoms of lacrimal gland tumors?
Most patients experience painless upper eyelid swelling, a visible or palpable lump, changes in eye position, and sometimes double vision. Sudden pain or rapid growth can signal a more aggressive tumor and warrants urgent medical attention.
How are lacrimal gland tumors diagnosed?
Diagnosis combines a thorough eye exam with imaging such as CT or MRI to assess the size and location. Definitive diagnosis is made by surgical biopsy, which allows for histopathological analysis.
Can lacrimal gland tumors be treated without surgery?
Some benign or lymphoid tumors can be monitored or treated with medications such as steroids or chemotherapy. However, most solid tumors require surgical removal for cure or control.
What is the prognosis for patients with lacrimal gland tumors?
Prognosis varies by tumor type. Benign tumors usually have excellent outcomes with surgery. Early-detected malignant tumors can also be cured, but aggressive types may recur or metastasize.
Are there new, less invasive treatments for lacrimal gland tumors?
Yes, advances such as minimally invasive and robotic-assisted surgeries, targeted therapies, and new radiation techniques are increasingly available, offering improved outcomes and shorter recovery.
How important is long-term follow-up after treatment?
Regular follow-up is crucial to detect recurrence, manage dry eye or cosmetic changes, and monitor for late effects of treatment, especially after malignant tumors.
Disclaimer:
This article is for educational purposes only and should not be considered a substitute for professional medical advice, diagnosis, or treatment. Always consult your healthcare provider for guidance about any medical condition.
If you found this resource helpful, please consider sharing it on Facebook, X (formerly Twitter), or any social media platform. Follow us for more eye health guides—and thank you for supporting our mission to provide quality, accessible medical information!






