The bronchioles are the smallest airways within the lungs, playing a pivotal role in directing air to the alveoli where gas exchange occurs. Despite their diminutive size, these structures are integral to respiratory efficiency and defense. They actively regulate airflow, assist in trapping harmful particles, and facilitate the critical transition from air conduction to gas exchange. This guide delves into every facet of bronchiolar anatomy, physiological functions, common disorders, modern diagnostic techniques, treatment modalities, nutritional support, and lifestyle practices designed to preserve lung health. Discover the intricate workings of your respiratory system and learn effective strategies to support optimal bronchiolar function.
Table of Contents
- Structural Insights of Bronchioles
- Functional Dynamics and Airflow Control
- Disorders Impacting Bronchioles
- Diagnostic Approaches and Tools
- Treatment Modalities and Innovations
- Nutritional & Supplement Support
- Lifestyle Strategies for Bronchiolar Health
- Reliable Resources and Further Reading
- Frequently Asked Questions
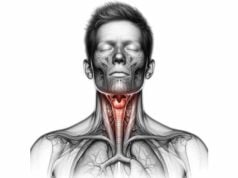
Structural Insights of Bronchioles
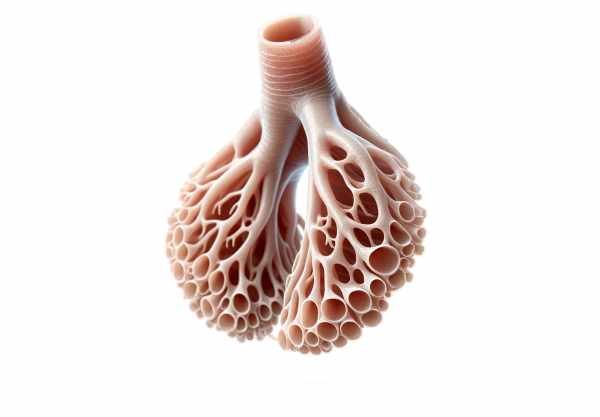
The bronchioles form an intricate network deep within the lungs, bridging the gap between the larger airways and the tiny alveolar sacs where gas exchange occurs. They begin where the bronchi subdivide into progressively smaller tubes, eventually culminating in the respiratory bronchioles. This elaborate branching ensures that air is evenly distributed throughout the lung tissue, optimizing the surface area for oxygen and carbon dioxide exchange.
Classification and Subtypes
Bronchioles can be categorized based on their location and function within the respiratory system:
- Primary (Lobular) Bronchioles: These are the first subdivisions emerging from the larger bronchi and serve as conduits directing air to individual lung lobules.
- Terminal Bronchioles: Found at the end of the conducting zone, these narrow passages mark the final stage of air conduction before transitioning to the respiratory region.
- Respiratory Bronchioles: Distinguished by the emergence of alveoli along their walls, these structures signify the beginning of the gas exchange area. Their delicate architecture facilitates the diffusion of oxygen into the bloodstream while expelling carbon dioxide.
Histological Layers and Cellular Composition
The structural integrity of bronchioles is maintained by a series of specialized layers, each with distinct functions:
- Epithelial Lining:
The inner surface is lined with a simple cuboidal or columnar epithelium. As bronchioles approach the alveolar sacs, the cells tend to flatten. This lining contains ciliated cells that aid in the removal of mucus and debris, and Clara (club) cells that detoxify inhaled substances and secrete essential surfactant components. - Lamina Propria:
Directly beneath the epithelium lies the lamina propria, a loose connective tissue rich in elastic fibers. This layer provides flexibility, allowing the bronchioles to stretch during inhalation and recoil during exhalation. - Smooth Muscle Layer:
Encircling the bronchioles is a layer of smooth muscle. This muscle is highly responsive to autonomic signals, enabling dynamic regulation of airway diameter through contraction (bronchoconstriction) and relaxation (bronchodilation). - Adventitia:
The outermost layer consists of connective tissue that anchors the bronchioles to the surrounding lung parenchyma, ensuring stability and structural support during respiratory movements.
Relationship with Adjacent Structures
Bronchioles interface seamlessly with several critical components of the respiratory system:
- Alveolar Ducts and Sacs:
Respiratory bronchioles open into alveolar ducts, which further subdivide into clusters of alveoli. This arrangement maximizes the area available for gas exchange, ensuring that every breath is effectively utilized. - Vascular Supply:
A dense network of capillaries envelops the bronchioles, supplied by both pulmonary and bronchial arteries. This vascular integration is essential for efficient nutrient delivery and rapid gas exchange, supporting the high metabolic demands of lung tissues. - Neural and Immune Elements:
The bronchioles are innervated by the autonomic nervous system, which precisely modulates airway tone. In addition, lymphatic channels and immune cells within the tissue contribute to local defense mechanisms, protecting the delicate airways from pathogens and environmental pollutants.
In summary, the structural design of the bronchioles—with their intricate branching, specialized cell types, and supportive connective tissues—ensures that air is delivered efficiently to the alveoli. This robust architecture is fundamental to maintaining optimal respiratory function and serves as the foundation for the many complex processes that sustain lung health.
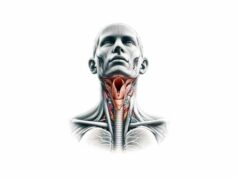
Functional Dynamics and Airflow Control
Bronchioles play a dynamic role in the respiratory system, extending far beyond simple air passageways. Their primary function is to regulate the distribution of air within the lungs, ensuring that every alveolus receives a sufficient supply of oxygen while facilitating the removal of carbon dioxide. This regulation is achieved through an intricate balance of muscular activity, neural input, and cellular processes.
Air Conduction and Distribution
At the heart of bronchiolar function is the effective conduction of air:
- Efficient Air Transport:
As air moves from the larger bronchi into the fine network of bronchioles, it is guided by the tapering diameter and extensive branching. This design allows for the even distribution of air across the entire lung surface. - Surface Area Maximization:
The vast network of bronchioles increases the overall surface area available for gas exchange. By the time air reaches the alveolar sacs, it is optimally conditioned for the diffusion of oxygen into the bloodstream.
Regulation of Airflow
The bronchioles actively modulate the resistance and flow of air through their smooth muscle layer:
- Bronchodilation:
Stimulation of the sympathetic nervous system relaxes the smooth muscle, widening the airways and reducing resistance. This process is particularly important during physical exertion or in response to stress, allowing for increased airflow. - Bronchoconstriction:
In contrast, parasympathetic activation results in the contraction of smooth muscle fibers, narrowing the bronchioles. This mechanism serves as a protective response against inhaled irritants, allergens, or harmful substances, reducing the risk of damage to delicate lung tissues.
Gas Exchange Facilitation
Although the primary site for gas exchange is the alveoli, the bronchioles play an essential preparatory role:
- Transition Zone:
The respiratory bronchioles, with their scattered alveoli, represent the critical transition from the conducting zone to the respiratory zone. This design ensures that oxygen is efficiently absorbed into the bloodstream and carbon dioxide is expelled. - Optimizing Air Conditions:
As air passes through the bronchioles, it is not only distributed evenly but also conditioned—warmed and humidified—to match the body’s requirements. This conditioning is vital for maintaining alveolar integrity and ensuring efficient gas exchange.
Protective and Cleansing Mechanisms
The bronchioles also contribute to the lung’s defense system:
- Mucociliary Clearance:
Although less prominent than in larger airways, the mucociliary apparatus in bronchioles traps inhaled particles and pathogens. The coordinated beating of cilia helps transport mucus, along with any entrapped debris, upward toward the pharynx for expulsion. - Clara Cells Functionality:
Clara cells, located within the bronchiolar epithelium, secrete surfactant components that reduce surface tension and maintain airway patency. They also play a detoxifying role, metabolizing harmful substances and protecting the lung tissue from damage.
Integration with Respiratory Mechanics
The dynamic functions of the bronchioles are seamlessly integrated with the overall mechanics of breathing:
- Lung Compliance and Elasticity:
The elastic fibers within the lamina propria contribute to the bronchioles’ ability to stretch and recoil. This elasticity is essential for maintaining lung compliance, allowing for efficient expansion during inhalation and recoil during exhalation. - Coordinated Response:
The bronchioles work in concert with the diaphragm, intercostal muscles, and other components of the respiratory system to ensure that the process of breathing remains smooth and efficient under varying physiological conditions.
In essence, the functional dynamics of the bronchioles encompass a range of activities—from air conduction and conditioning to active modulation of airflow and protective cleansing. Their ability to adapt to changing demands and environmental challenges is a testament to the sophisticated design of the respiratory system, ensuring that every breath supports optimal lung performance.
Disorders Impacting Bronchioles
A variety of pathological conditions can compromise the integrity and function of the bronchioles, leading to significant respiratory difficulties. Understanding these disorders is essential for early diagnosis, effective management, and prevention of long-term complications. In this section, we explore several common and clinically significant conditions that affect bronchiolar health.
Bronchiolitis
Bronchiolitis is an acute inflammatory condition primarily affecting the bronchioles, most commonly seen in infants and young children.
- Etiology and Presentation:
Often caused by viral infections—most notably respiratory syncytial virus (RSV)—bronchiolitis leads to swelling, mucus production, and narrowing of the airways. Clinical symptoms include persistent coughing, wheezing, and labored breathing. - Management:
Treatment is largely supportive, focusing on maintaining adequate hydration, oxygen supplementation, and, in severe cases, hospitalization for respiratory support. Preventative measures include hand hygiene and, where available, prophylactic therapies for high-risk infants.
Asthma
Asthma is a chronic inflammatory disease that affects both the large airways and the bronchioles.
- Pathophysiology:
Characterized by episodic bronchoconstriction and airway hyperresponsiveness, asthma triggers include allergens, irritants, and infections. In the bronchioles, the inflammation leads to increased mucus production and narrowing of the airways. - Clinical Features and Management:
Patients typically experience wheezing, shortness of breath, chest tightness, and coughing. Long-term management involves avoiding triggers, using inhaled bronchodilators, corticosteroids, and developing personalized asthma action plans to control symptoms.
Chronic Obstructive Pulmonary Disease (COPD)
COPD is an umbrella term that includes chronic bronchitis and emphysema, conditions that lead to persistent airflow limitation.
- Bronchiolar Involvement:
In COPD, chronic inflammation of the bronchioles results in mucus hypersecretion, structural remodeling, and airway narrowing. These changes contribute to the characteristic symptoms of chronic cough, sputum production, and dyspnea. - Treatment Strategies:
Management includes smoking cessation, pharmacotherapy with bronchodilators and corticosteroids, pulmonary rehabilitation, and oxygen therapy in advanced stages.
Bronchiolitis Obliterans
Also known as obliterative bronchiolitis, this condition involves progressive inflammation and fibrosis of the bronchioles.
- Causes and Manifestations:
It can result from severe infections, exposure to toxic chemicals, or complications following lung transplantation. Patients typically present with progressive shortness of breath and a persistent dry cough. - Management and Prognosis:
Treatment options are limited and often involve immunosuppressive therapies. In severe cases, lung transplantation may be considered; however, the condition generally has a poor prognosis.
Respiratory Infections
Acute and chronic infections can directly affect the bronchioles, leading to inflammation and compromised airway function.
- Common Pathogens:
Bacterial infections, such as those causing pneumonia or bronchitis, as well as viral pathogens, can trigger significant bronchiolar inflammation. - Management Approaches:
Appropriate antibiotic or antiviral therapy, along with supportive care such as hydration and oxygen therapy, is critical to resolving infections and preventing further complications.
Cystic Fibrosis
Cystic fibrosis is a genetic disorder that results in the production of thick, sticky mucus that can obstruct the bronchioles.
- Pathological Features:
The abnormal mucus impairs mucociliary clearance, making patients prone to recurrent infections and chronic inflammation. Over time, these changes can lead to permanent structural damage. - Treatment Considerations:
Management involves airway clearance techniques, mucolytic agents, aggressive antimicrobial therapy, and in advanced cases, lung transplantation.
Hypersensitivity Pneumonitis
This immunologically mediated condition occurs in response to repeated inhalation of organic dusts or chemicals.
- Clinical Presentation:
Patients often experience fever, cough, and dyspnea following exposure to allergens. The resulting inflammation can affect both the bronchioles and the alveoli. - Management:
Avoidance of the offending antigen is crucial, along with the use of corticosteroids to reduce inflammation.
In summary, disorders affecting the bronchioles range from acute viral infections to chronic inflammatory conditions and genetic disorders. Recognizing the distinct clinical features and underlying mechanisms of each condition is critical for timely intervention and effective long-term management, ultimately preserving respiratory function and improving patient outcomes.
Diagnostic Approaches and Tools
Accurate diagnosis of bronchiolar disorders is paramount to ensuring effective treatment and preventing irreversible lung damage. Clinicians employ a combination of clinical assessments, imaging modalities, and specialized tests to evaluate bronchiolar function and identify pathological changes.
Clinical Assessment
- Comprehensive History and Physical Examination:
The diagnostic process typically begins with a detailed patient history, focusing on symptoms such as coughing, wheezing, and shortness of breath. Clinicians also consider risk factors like exposure to irritants, smoking history, and family history of respiratory disorders. A thorough physical examination, including auscultation, helps detect abnormal lung sounds indicative of airway obstruction or inflammation. - Symptom Evaluation:
Symptoms are carefully correlated with potential triggers and environmental exposures. In cases of suspected asthma or bronchiolitis, clinicians look for episodic wheezing and a history of allergen exposure.
Pulmonary Function Testing (PFT)
Pulmonary function tests provide quantitative data on lung performance:
- Spirometry:
This test measures lung volumes and airflow parameters, such as Forced Expiratory Volume in one second (FEV₁) and Forced Vital Capacity (FVC). Abnormal values can indicate obstructive or restrictive lung patterns. - Bronchial Provocation Tests:
These tests assess airway hyperresponsiveness by exposing the patient to specific stimuli (e.g., methacholine) and monitoring the resultant changes in lung function.
Imaging Techniques
Visualizing the lung structure is crucial in diagnosing bronchiolar disorders:
- Chest X-ray:
Although a basic imaging modality, chest X-rays can reveal gross abnormalities such as hyperinflation, atelectasis, or focal infiltrates that suggest an underlying bronchiolar pathology. - High-Resolution Computed Tomography (HRCT):
HRCT scans provide detailed cross-sectional images of the airways and lung parenchyma. They are particularly valuable for detecting subtle changes like bronchiolar wall thickening, air trapping, and areas of mosaic attenuation. - Magnetic Resonance Imaging (MRI):
While less commonly used, MRI offers excellent soft tissue contrast without ionizing radiation and can be useful in evaluating complex congenital or inflammatory conditions.
Bronchoscopy and Related Procedures
- Flexible Bronchoscopy:
This minimally invasive procedure allows direct visualization of the bronchioles. It can identify mucosal abnormalities, obstructions, or signs of inflammation. Bronchoscopy also provides an opportunity for tissue biopsy when necessary. - Bronchoalveolar Lavage (BAL):
During bronchoscopy, a saline solution is instilled into the bronchioles and then retrieved for analysis. BAL fluid is examined for inflammatory cells, pathogens, and other markers that aid in diagnosis.
Laboratory and Advanced Diagnostic Tests
- Sputum Analysis:
Examining expectorated mucus can help identify infectious agents, inflammatory markers, or malignant cells. - Blood Tests:
Complete blood counts, immunological panels, and markers of inflammation (such as C-reactive protein) support the clinical diagnosis. - Lung Biopsy and Genetic Testing:
In uncertain or complex cases, a lung biopsy may be performed to obtain histopathological evidence. For genetic disorders like cystic fibrosis, genetic testing confirms the presence of specific mutations.
By integrating clinical evaluation with a broad spectrum of diagnostic tools—from simple spirometry to advanced imaging and invasive procedures—healthcare providers can form a comprehensive understanding of bronchiolar health. This multi-pronged approach is essential for tailoring treatment strategies to the individual needs of each patient.
Treatment Modalities and Innovations
Effective management of bronchiolar disorders requires a tailored approach that combines pharmacological therapies, non-pharmacological interventions, and, in some cases, advanced surgical techniques. The overarching goal is to alleviate symptoms, control inflammation, and preserve lung function over the long term.
Pharmacological Interventions
Medications remain a cornerstone in the treatment of bronchiolar conditions:
- Bronchodilators:
- Short-acting Beta-agonists (SABAs), such as albuterol, provide rapid relief from acute bronchoconstriction by relaxing the smooth muscle.
- Long-acting Beta-agonists (LABAs), including salmeterol, are used for maintenance therapy to keep the airways open over extended periods.
- Corticosteroids:
- Inhaled Corticosteroids (ICS) reduce chronic airway inflammation and are vital in conditions like asthma and COPD.
- Systemic Corticosteroids are reserved for severe exacerbations, providing potent anti-inflammatory effects.
- Antibiotics and Antivirals:
When bacterial or viral infections contribute to bronchiolar inflammation, targeted antibiotic or antiviral therapy is administered. - Mucolytics:
Agents such as N-acetylcysteine (NAC) help break down thick mucus, facilitating its clearance and improving airflow.
Non-Pharmacological Strategies
Alongside medications, several supportive therapies enhance bronchiolar function:
- Pulmonary Rehabilitation:
Structured exercise and breathing programs help improve lung capacity, reduce dyspnea, and enhance overall quality of life. - Oxygen Therapy:
Supplemental oxygen is provided in cases of significant hypoxemia to maintain adequate tissue oxygenation. - Lifestyle Modification:
Measures such as smoking cessation, allergen avoidance, and maintaining a clean living environment are integral to managing chronic respiratory conditions.
Surgical and Interventional Procedures
For patients unresponsive to conventional therapy, invasive options may be considered:
- Bronchial Thermoplasty:
This innovative procedure uses controlled thermal energy to reduce airway smooth muscle mass, thereby decreasing bronchoconstriction in severe asthma. - Lung Volume Reduction Surgery (LVRS):
LVRS removes diseased lung tissue, improving overall lung mechanics and breathing efficiency in patients with emphysema. - Lung Transplantation:
In cases of end-stage lung disease, transplantation offers a last-resort solution, albeit with significant risks and the need for lifelong immunosuppression.
Emerging and Experimental Therapies
Research continues to drive the development of novel treatments:
- Gene Therapy:
Investigational approaches aim to correct genetic defects underlying conditions like cystic fibrosis by targeting bronchiolar epithelial cells. - Regenerative Medicine:
Stem cell therapies and tissue engineering hold promise for repairing or regenerating damaged bronchiolar tissues. - Telemedicine and Digital Health:
Remote monitoring and virtual consultations enable real-time management of chronic respiratory conditions, enhancing patient adherence and timely interventions.
By combining these diverse treatment modalities, clinicians can address the multifaceted nature of bronchiolar disorders. Personalized care plans that integrate pharmacological, non-pharmacological, and innovative interventions offer the best chance of restoring and maintaining optimal respiratory function.
Nutritional & Supplement Support for Bronchiolar Wellness
A balanced diet and targeted nutritional supplementation can play a crucial role in reducing inflammation and supporting the overall health of the bronchioles. Specific vitamins, minerals, and natural compounds contribute to maintaining optimal lung function and enhancing the body’s natural defense mechanisms.
Key Nutrients for Respiratory Health
- Vitamin D:
Essential for modulating immune responses, vitamin D helps reduce airway inflammation and may decrease the frequency of respiratory infections. - Vitamin C:
A potent antioxidant, vitamin C mitigates oxidative stress within the bronchioles, supporting tissue repair and immune function. - Omega-3 Fatty Acids:
Found in fish oil and certain plant sources, omega-3s possess anti-inflammatory properties that can help alleviate chronic bronchial inflammation.
Herbal and Natural Supplements
- Echinacea:
Known for its immunomodulatory effects, echinacea is commonly used to bolster respiratory defenses, although evidence regarding its efficacy is mixed. - Licorice Root:
Traditionally used to soothe irritated airways, licorice root also acts as an expectorant, promoting the clearance of mucus.
Enzymatic and Antioxidant Agents
- N-acetylcysteine (NAC):
As a mucolytic agent, NAC helps break down thick mucus while providing antioxidant protection to the bronchiolar tissues. - Coenzyme Q10 (CoQ10):
This antioxidant supports cellular energy production and may help reduce oxidative damage in respiratory cells.
Hormonal Support
- Melatonin:
Beyond its role in regulating sleep, melatonin exhibits antioxidant properties that can protect the bronchioles from inflammatory damage, particularly in conditions where oxidative stress is elevated.
Integrating these nutritional strategies into your daily routine can support bronchiolar health by reducing inflammation, enhancing immune function, and promoting overall respiratory resilience. A diet rich in fruits, vegetables, lean proteins, and healthy fats, combined with targeted supplementation, provides a strong foundation for lung health.
Lifestyle Strategies for Sustained Bronchiolar Function
Maintaining bronchiolar health extends far beyond clinical treatments; everyday lifestyle choices play a significant role in supporting respiratory wellness. By adopting proactive habits and environmental strategies, you can protect your airways from chronic damage and promote long-term lung function.
Essential Lifestyle Modifications
- Smoking Cessation:
Avoiding tobacco smoke is critical, as smoking is a major risk factor for chronic respiratory diseases. Quitting smoking can dramatically improve bronchiolar function and reduce inflammation. - Hydration:
Drinking plenty of water helps keep mucus thin, facilitating its clearance from the airways and reducing irritation. - Regular Physical Activity:
Consistent exercise improves lung capacity, strengthens respiratory muscles, and enhances overall cardiovascular health.
Environmental and Home-Based Practices
- Air Quality Management:
Using air purifiers, maintaining clean indoor environments, and avoiding exposure to pollutants can minimize respiratory irritants. - Humidity Control:
Utilizing humidifiers, especially in dry climates or during winter months, helps prevent the bronchioles from becoming overly dry and inflamed. - Allergen Avoidance:
Identify and reduce exposure to allergens—such as dust mites, pollen, or pet dander—that can trigger bronchoconstriction and inflammation.
Preventive Healthcare Measures
- Vaccinations:
Regular immunizations against influenza, pneumonia, and other respiratory infections are essential to protect the bronchioles from infectious agents. - Hygiene Practices:
Frequent handwashing and maintaining overall cleanliness can reduce the risk of respiratory infections that compromise bronchiolar health.
Adopting these lifestyle strategies can substantially contribute to the preservation of bronchiolar function. Consistent, proactive habits not only support your respiratory system but also enhance overall health and resilience against environmental challenges.
Reliable Resources and Further Reading
Staying informed about bronchiolar health is essential for both patients and healthcare professionals. A wealth of authoritative resources is available, including books, academic journals, and digital tools, to provide ongoing education and insights into respiratory medicine.
Recommended Books
- “The Respiratory System at a Glance” by Jeremy P.T. Ward and Jane Ward:
An accessible guide that offers a comprehensive overview of lung anatomy, physiology, and the role of the bronchioles in respiratory function. - “Respiratory Physiology: The Essentials” by John B. West:
This text delves into the mechanics of breathing and explains the intricate processes that govern gas exchange. - “Principles of Pulmonary Medicine” by Steven E. Weinberger, Barbara A. Cockrill, and Jess Mandel:
A detailed resource covering a wide range of topics, including the diagnosis and treatment of bronchiolar disorders.
Academic Journals
- American Journal of Respiratory and Critical Care Medicine:
Publishes high-quality research on lung diseases and novel therapeutic approaches. - Chest:
A leading journal in respiratory medicine offering in-depth reviews and clinical studies on various aspects of lung health.
Digital Tools and Mobile Apps
- MyAsthma:
A mobile app designed to help individuals track asthma symptoms, manage medications, and monitor lung function. - Breathing Zone:
Provides guided breathing exercises aimed at improving respiratory efficiency and reducing stress. - Lung Health Check:
An app that offers easy access to lung function tests, health tips, and symptom tracking to promote proactive respiratory care.
These resources provide valuable information for anyone looking to deepen their understanding of bronchiolar health, stay abreast of the latest research, or find practical tools for managing chronic respiratory conditions.
Frequently Asked Questions About Bronchioles
What are bronchioles and why are they important?
Bronchioles are the smallest air passages in the lungs, responsible for directing air to the alveoli where gas exchange occurs. They play a crucial role in regulating airflow, protecting against inhaled irritants, and ensuring that oxygen is efficiently absorbed into the bloodstream.
How do bronchioles regulate airflow?
Bronchioles adjust their diameter through the contraction and relaxation of smooth muscle fibers. This regulation, controlled by the autonomic nervous system, ensures optimal airflow by balancing bronchodilation and bronchoconstriction in response to various stimuli.
What conditions commonly affect the bronchioles?
Conditions such as bronchiolitis, asthma, COPD, bronchiolitis obliterans, respiratory infections, cystic fibrosis, and hypersensitivity pneumonitis can adversely impact bronchiolar function, leading to symptoms like coughing, wheezing, and shortness of breath.
What diagnostic tests are used for bronchiolar disorders?
Diagnosis involves clinical assessments, pulmonary function tests (spirometry), imaging techniques (chest X-ray, HRCT, MRI), bronchoscopy with BAL, and laboratory tests such as sputum analysis and blood panels, which together help identify the specific nature of the disorder.
What lifestyle changes can improve bronchiolar health?
Improving bronchiolar health involves quitting smoking, staying well-hydrated, engaging in regular exercise, maintaining a balanced diet, controlling indoor allergens, using humidifiers, and getting vaccinated to prevent respiratory infections.
Disclaimer:
The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a healthcare provider for personalized guidance.
If you found this guide helpful, please share it on Facebook, X (formerly Twitter), or your preferred social media platform to help spread awareness about bronchiolar health and wellness.