Cartilages are a unique and specialized form of connective tissue that serve critical roles in the human body. They provide flexible support, absorb shock, and maintain the integrity of joints and other structures. This resilient tissue is found throughout the body – from the joints and rib cage to the nose and ears – where it facilitates smooth movement and protects vital organs. In this comprehensive guide, we delve into the intricate anatomy of cartilages, explore their physiological functions, examine common disorders, and discuss modern diagnostic techniques and treatment options. Additionally, you will find nutritional, supplemental, and lifestyle tips to help maintain cartilage health for overall well-being.
Table of Contents
- Anatomical Structure & Composition
- Biomechanical Functions & Roles
- Growth, Development & Repair Mechanisms
- Regional Variations & Specific Structures
- Cartilage Pathologies & Clinical Manifestations
- Diagnostic Evaluation Techniques
- Treatment Interventions & Strategies
- Nutritional Support & Supplementation
- Lifestyle Strategies for Cartilage Health
- Educational Resources & References
- Frequently Asked Questions
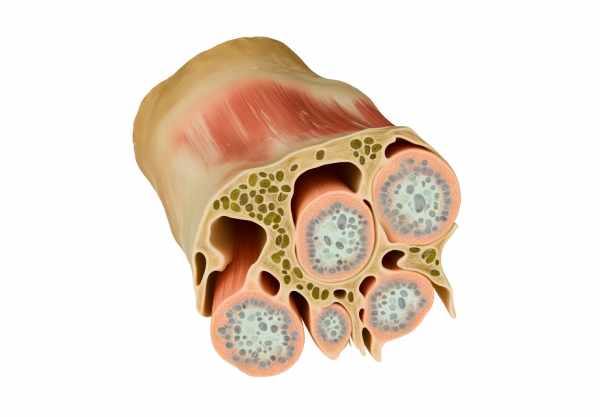
Anatomical Structure & Composition
Cartilage is a specialized, resilient connective tissue that is remarkably distinct in its structure compared to other tissues in the body. Unlike bone, cartilage is avascular, meaning it lacks its own blood supply. Instead, it relies on diffusion from surrounding tissues to obtain nutrients and eliminate waste. Its unique composition and arrangement of cells and extracellular matrix provide the flexibility and durability necessary for various functions.
Cellular Components and Matrix Organization
- Chondrocytes:
The primary cell type found in cartilage is the chondrocyte. These cells reside within small cavities known as lacunae and are responsible for producing and maintaining the extracellular matrix (ECM). They secrete essential components such as collagen fibers and proteoglycans, which give cartilage its strength and elasticity. - Extracellular Matrix (ECM):
The ECM of cartilage is composed of a dense network of collagen fibers—predominantly type II collagen—interwoven with proteoglycans and glycosaminoglycans (GAGs). This matrix not only provides structural support but also plays a key role in the tissue’s ability to absorb shock and resist compressive forces. - Basement Membrane and Perichondrium:
Although cartilage itself is avascular, it is often surrounded by a layer of dense connective tissue called the perichondrium. This membrane contains blood vessels that supply nutrients by diffusion. It also contains progenitor cells that can differentiate into chondroblasts, supporting cartilage growth and repair.
Distinctive Features of Cartilage Tissue
- Avascularity:
The absence of blood vessels in cartilage means that its metabolic processes rely on the slow diffusion of nutrients and oxygen through the ECM. This characteristic contributes to cartilage’s limited capacity for self-repair. - High Water Content:
Cartilage typically contains a significant amount of water, which is essential for maintaining its viscoelastic properties. The water is bound within the proteoglycan matrix, helping the tissue to resist compressive forces and maintain hydration. - Collagen and Proteoglycans:
The interplay between collagen fibers and proteoglycans is central to cartilage’s function. Collagen provides tensile strength and structural integrity, while proteoglycans attract water and impart resistance to compression.
Overall, the specialized structure of cartilage—characterized by chondrocytes embedded in a robust yet flexible extracellular matrix—enables it to fulfill its roles in support, cushioning, and facilitating smooth joint movements throughout the body.
Biomechanical Functions & Roles
Cartilage plays an essential role in ensuring the mechanical efficiency of various bodily structures. Its unique biomechanical properties allow it to serve as both a shock absorber and a facilitator of smooth, frictionless motion within joints and other areas.
Joint Support and Articulation
- Articular Cartilage:
Articular cartilage covers the ends of bones in synovial joints, providing a smooth, lubricated surface that minimizes friction during movement. This cushioning effect is critical for protecting the underlying bone from wear and tear, particularly in high-impact activities. - Load Distribution:
The cartilage in joints helps distribute forces evenly across the joint surface. By absorbing and dispersing shock, it prevents localized stress concentrations that could lead to joint degeneration or injury.
Structural Flexibility and Resilience
- Elastic Cartilage:
Found in structures such as the external ear and the epiglottis, elastic cartilage contains a high concentration of elastic fibers that impart flexibility and allow these structures to bend and return to their original shape. This flexibility is crucial for maintaining the form and function of organs that require both structural support and pliability. - Fibrocartilage:
In areas subjected to high mechanical stress, such as intervertebral discs and the menisci of the knee, fibrocartilage provides significant tensile strength and shock absorption. Its dense, fibrous composition helps resist compressive forces and protect adjacent bone and soft tissue.
Respiratory and Protective Functions
- Tracheal and Bronchial Cartilage:
In the respiratory system, hyaline cartilage rings in the trachea and bronchi play a critical role in maintaining airway patency. These cartilage structures prevent the collapse of the airways during inhalation and exhalation, ensuring unobstructed airflow. - Laryngeal Cartilage:
Cartilaginous structures within the larynx, including the thyroid, cricoid, and arytenoid cartilages, support the vocal cords and contribute to voice production. They also protect the airway during swallowing, preventing aspiration.
Protective and Cushioning Roles
- Shock Absorption:
Cartilage in the joints and intervertebral discs acts as a natural shock absorber, reducing the impact of forces transmitted through the skeletal system. This protective function is especially important during high-impact activities such as running or jumping. - Energy Dissipation:
The viscoelastic properties of cartilage allow it to dissipate energy efficiently, protecting surrounding tissues from injury during sudden movements or impacts.
The biomechanical roles of cartilage are vital for overall movement, stability, and protection of various body structures. Its capacity to reduce friction, distribute loads, and absorb shock makes it indispensable for maintaining joint integrity and ensuring the smooth functioning of the musculoskeletal system.
Growth, Development & Repair Mechanisms
Cartilage is unique in its growth and repair processes due to its avascular nature. While its lack of direct blood supply limits regenerative capacity, cartilage does exhibit specialized growth mechanisms that are crucial during development and, to some extent, for maintenance and repair throughout life.
Modes of Cartilage Growth
- Appositional Growth:
In this process, new cartilage is added to the surface by chondroblasts derived from the perichondrium. These cells differentiate into chondrocytes and secrete new matrix, allowing the cartilage to expand in width. - Interstitial Growth:
Interstitial growth occurs when chondrocytes within the cartilage divide and produce additional matrix. This form of growth is essential during the development of the skeletal system, particularly in the formation of long bones.
Endochondral Ossification
- Cartilage as a Bone Template:
During skeletal development, cartilage serves as a precursor to bone in a process known as endochondral ossification. In growth plates, cartilage is gradually replaced by bone tissue, facilitating the longitudinal growth of bones. - Role in Development:
Endochondral ossification is a critical mechanism during childhood and adolescence, allowing bones to grow in length while maintaining proper shape and structural integrity.
Limited Repair Capabilities
- Avascular Nature and Repair:
The lack of blood vessels in cartilage means that its repair mechanisms are slower compared to vascularized tissues. Nutrient diffusion is limited, which can impede the migration of repair cells to the site of injury. - Chondrocyte Activity:
Despite these limitations, chondrocytes play a crucial role in maintaining and repairing the cartilage matrix. They continuously produce and remodel the extracellular matrix, albeit at a slow pace. - Stimulated Repair Techniques:
Medical interventions such as microfracture, autologous chondrocyte implantation (ACI), and matrix-induced ACI (MACI) have been developed to stimulate cartilage repair by encouraging new cell growth and matrix production.
Factors Influencing Cartilage Regeneration
- Age:
Younger individuals typically exhibit more robust cartilage repair mechanisms compared to older adults, due to higher metabolic activity and greater cellular responsiveness. - Mechanical Stress:
Moderate, controlled mechanical loading can stimulate cartilage repair and maintenance, while excessive stress may lead to degeneration and injury. - Nutritional Status:
Adequate nutrition, particularly the availability of vitamins and minerals essential for collagen synthesis, is critical for maintaining cartilage health and facilitating repair processes.
Although cartilage has inherent limitations in its ability to regenerate, understanding the mechanisms behind its growth and repair has paved the way for advanced therapeutic interventions. By harnessing these natural processes, modern medicine continues to explore innovative ways to restore cartilage function and improve joint health.
Regional Variations & Specific Structures
Cartilage is not a uniform tissue; its structure and function vary significantly depending on its anatomical location. These regional differences allow cartilage to meet the unique mechanical and physiological demands of different body parts.
Articular Cartilage in Joints
- Structure and Function:
Articular cartilage covers the surfaces of bones in synovial joints, providing a smooth, lubricated interface that minimizes friction during movement. Its resilience and capacity to absorb shock are critical for protecting joints from wear and tear. - Clinical Relevance:
Degeneration of articular cartilage is a hallmark of osteoarthritis, leading to joint pain, stiffness, and reduced mobility.
Costal Cartilage
- Role in the Rib Cage:
Costal cartilage connects the ribs to the sternum, imparting both flexibility and stability to the thoracic cage. This cartilage allows the ribcage to expand and contract during respiration, supporting breathing. - Unique Features:
Its elastic properties are essential for accommodating the mechanical stresses of breathing and protecting the internal organs.
Nasal and Auricular Cartilage
- Nasal Cartilage:
The cartilage in the nose provides structural support while allowing for some degree of flexibility. It plays a key role in shaping the nasal contour and maintaining airway patency. - Auricular (Ear) Cartilage:
Found in the external ear, this cartilage is highly flexible, enabling the ear to maintain its shape while also allowing for movement and sound conduction.
Intervertebral Discs and Menisci
- Fibrocartilage in the Spine:
Intervertebral discs, composed largely of fibrocartilage, serve as shock absorbers between vertebrae. They facilitate spinal flexibility and help distribute compressive forces. - Knee Menisci:
The menisci in the knee are C-shaped fibrocartilaginous structures that enhance joint stability, absorb shock, and distribute loads across the joint surface.
Laryngeal and Tracheal Cartilage
- Airway Support:
Hyaline cartilage structures in the larynx and trachea maintain open airways, enabling effective respiration. They protect the airway from collapse during breathing and play roles in sound production and airway protection. - Functional Adaptations:
These cartilaginous rings are rigid enough to withstand the pressures of breathing while flexible enough to allow for movement and articulation of the vocal cords.
The diversity in cartilage types and structures across different regions of the body highlights the specialized roles this tissue plays. Each type of cartilage is uniquely adapted to fulfill the specific functional requirements of its location, from providing cushioning in joints to maintaining the structural integrity of airways and supporting facial features.
Cartilage Pathologies & Clinical Manifestations
Cartilage disorders can have a profound impact on mobility, joint function, and overall quality of life. Damage to cartilage may result from degenerative processes, autoimmune conditions, trauma, or congenital factors. Understanding the clinical manifestations of these conditions is essential for accurate diagnosis and effective management.
Osteoarthritis (OA)
- Pathophysiology:
Osteoarthritis is a degenerative joint disease characterized by the progressive loss of articular cartilage. As cartilage deteriorates, the underlying bone becomes exposed, leading to pain, inflammation, and joint stiffness. - Symptoms:
Patients typically experience joint pain, decreased range of motion, and crepitus (a grating sensation) during movement. The knees, hips, and hands are commonly affected. - Risk Factors:
Age, obesity, joint injuries, and genetic predisposition contribute to the development of OA.
Rheumatoid Arthritis (RA)
- Autoimmune Inflammation:
Unlike OA, rheumatoid arthritis is an autoimmune condition where the immune system mistakenly attacks joint tissues, including cartilage. This leads to chronic inflammation and subsequent erosion of cartilage and bone. - Clinical Presentation:
RA often affects multiple joints symmetrically, causing swelling, pain, and significant stiffness, particularly in the morning. - Management:
Treatment typically involves anti-inflammatory medications, disease-modifying antirheumatic drugs (DMARDs), and biologic agents to slow progression.
Chondromalacia Patellae
- Cartilage Softening:
This condition is characterized by the softening and deterioration of the cartilage on the underside of the patella (kneecap). It is often associated with malalignment of the knee joint. - Symptoms:
Patients report knee pain, especially when ascending or descending stairs, sitting for prolonged periods, or after physical activity. - Treatment:
Management includes physical therapy, rest, and in some cases, surgical interventions to realign the patella.
Intervertebral Disc Degeneration
- Fibrocartilage Breakdown:
Degeneration of the intervertebral discs, composed primarily of fibrocartilage, leads to decreased disc height, pain, and potential nerve compression. - Clinical Manifestations:
Patients may experience chronic back pain, sciatica, and reduced spinal flexibility. - Therapeutic Approaches:
Treatment options range from conservative management with physical therapy and medications to surgical interventions such as discectomy or spinal fusion.
Costochondritis
- Inflammatory Chest Pain:
Costochondritis involves inflammation of the costal cartilage connecting the ribs to the sternum, resulting in localized chest pain that can mimic cardiac conditions. - Diagnosis and Management:
The condition is typically self-limiting and is managed with rest, nonsteroidal anti-inflammatory drugs (NSAIDs), and lifestyle modifications.
Cartilage Injuries and Traumatic Lesions
- Acute Trauma:
Injuries to cartilage, especially in joints, can occur due to sports, accidents, or repetitive stress. Such injuries may lead to cartilage tears or fragmentation. - Clinical Impact:
Traumatic cartilage injuries often result in pain, swelling, and reduced joint mobility, potentially leading to early-onset osteoarthritis if left untreated. - Interventions:
Depending on severity, treatments may range from conservative management and physical therapy to surgical repair via arthroscopy.
Nasal Septum Deviation
- Structural Disruption:
A deviated nasal septum, caused by abnormal cartilage development or trauma, can lead to breathing difficulties and recurrent sinus infections. - Treatment:
Septoplasty, a surgical procedure to correct the alignment of the septum, is often required to restore proper airflow and alleviate symptoms.
Cauliflower Ear
- External Ear Deformity:
Repeated trauma to the ear’s elastic cartilage, commonly seen in contact sports, can cause the cartilage to become deformed and fibrotic, leading to the characteristic “cauliflower” appearance. - Management:
Early intervention with drainage and compression is key to preventing permanent deformity; severe cases may require surgical correction.
Each of these cartilage pathologies presents unique challenges, from the mechanical breakdown of tissue in osteoarthritis to the inflammatory destruction seen in rheumatoid arthritis. Early detection and targeted treatment are critical to preserving joint function and maintaining overall mobility.
Diagnostic Evaluation Techniques
Accurate diagnosis of cartilage disorders is crucial for determining the most appropriate treatment strategy. A comprehensive evaluation typically involves a combination of clinical assessments, imaging studies, and specialized tests to assess the integrity and function of cartilage.
Clinical Assessment and Patient History
- Detailed History:
A thorough patient history is essential for identifying symptoms, duration, and exacerbating factors. Key details include joint pain, stiffness, swelling, and any history of trauma or repetitive stress. - Physical Examination:
Clinicians assess joint range of motion, palpate for tenderness, and listen for crepitus (a grating sound) that may indicate cartilage wear. Observations of joint swelling or deformity further guide the diagnostic process.
Imaging Modalities
- X-rays:
Standard radiographs are useful for evaluating joint space narrowing, osteophyte formation, and other bony changes that indirectly indicate cartilage loss. - Magnetic Resonance Imaging (MRI):
MRI provides detailed images of both cartilage and soft tissues. Techniques such as T2 mapping and dGEMRIC (delayed gadolinium-enhanced MRI of cartilage) allow for quantitative analysis of cartilage composition and early degeneration. - Ultrasound:
Ultrasound is a non-invasive method for visualizing superficial cartilage structures, particularly in accessible joints like the knee. It can detect irregularities, effusions, and synovial inflammation. - Computed Tomography (CT):
Although primarily used for evaluating bone, CT scans, especially when combined with arthrography, can provide valuable insights into cartilage integrity and joint anatomy.
Arthroscopy
- Minimally Invasive Inspection:
Arthroscopy allows direct visualization of the joint interior. Surgeons can inspect the cartilage surface, identify tears or lesions, and perform diagnostic biopsies if necessary. - Therapeutic Interventions:
Arthroscopy is not only diagnostic but can also be used for treatment, including debridement, microfracture, or repair of cartilage defects.
Laboratory and Advanced Diagnostic Tests
- Synovial Fluid Analysis:
Analysis of joint fluid can help distinguish between inflammatory and degenerative joint diseases. Elevated inflammatory markers or the presence of crystals may indicate specific conditions such as gout or rheumatoid arthritis. - Biomarkers:
Emerging research into cartilage biomarkers aims to identify specific proteins or molecules in the blood or synovial fluid that correlate with cartilage degradation. - Genetic Testing:
In cases where hereditary conditions are suspected (e.g., certain forms of chondrodysplasia), genetic tests can provide definitive diagnoses.
By combining clinical evaluation with advanced imaging and laboratory techniques, healthcare providers can obtain a comprehensive picture of cartilage health. This integrative diagnostic approach is essential for planning effective treatments and monitoring disease progression.
Cartilage Treatment Strategies & Intervention Options
The management of cartilage disorders requires a personalized approach that considers the specific pathology, its severity, and the patient’s overall health. Treatment strategies range from non-surgical interventions and lifestyle modifications to advanced surgical procedures and emerging regenerative therapies.
Non-Surgical Approaches
- Physical Therapy:
Customized exercise programs aim to strengthen the muscles around affected joints, improve range of motion, and reduce pain. Low-impact exercises such as swimming, cycling, and walking are often recommended. - Medications:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs):
NSAIDs help manage pain and inflammation in conditions such as osteoarthritis and rheumatoid arthritis. - Analgesics:
Pain relievers like acetaminophen provide symptomatic relief without addressing the underlying inflammation. - Corticosteroid Injections:
Intra-articular corticosteroid injections offer temporary relief from inflammation, though repeated use may have adverse effects on cartilage integrity. - Hyaluronic Acid Injections:
Viscosupplementation with hyaluronic acid can improve joint lubrication and function in osteoarthritic joints. - Lifestyle Modifications:
Weight management, proper joint protection techniques, and low-impact exercise are critical for reducing stress on cartilage and slowing degeneration.
Surgical Treatments
- Arthroscopic Procedures:
- Debridement:
Removal of loose cartilage fragments and smoothing of damaged surfaces can alleviate pain and improve joint function. - Microfracture Technique:
Creating small perforations in the subchondral bone stimulates the formation of new fibrocartilage by encouraging blood and bone marrow factors to enter the defect. - Cartilage Restoration Techniques:
- Autologous Chondrocyte Implantation (ACI):
This two-stage procedure involves harvesting cartilage cells, culturing them, and re-implanting them into the cartilage defect to regenerate hyaline-like cartilage. - Osteochondral Autograft Transfer (OATS):
Involves transferring small plugs of cartilage and subchondral bone from less critical areas to regions of cartilage loss. - Matrix-Induced ACI (MACI):
An advanced form of ACI that uses a biodegradable scaffold to enhance cell delivery and integration, promoting more effective cartilage regeneration. - Joint Replacement:
For severe, end-stage cartilage loss, partial or total joint replacement may be necessary to restore function and alleviate chronic pain.
Emerging and Regenerative Therapies
- Stem Cell Therapy:
Research into mesenchymal stem cells (MSCs) aims to harness their regenerative potential to repair damaged cartilage and reduce inflammation. - Platelet-Rich Plasma (PRP):
PRP therapy involves concentrating platelets from the patient’s own blood and injecting them into the joint to promote healing and reduce inflammation. Though evidence is still evolving, some studies suggest beneficial effects on cartilage repair. - Biologic Agents:
Targeted biological therapies that modulate inflammatory pathways offer promising avenues for reducing cartilage degradation in autoimmune and degenerative joint diseases.
Overall, the treatment of cartilage disorders involves a multidisciplinary approach that may incorporate conservative management, advanced surgical interventions, and cutting-edge regenerative therapies. Tailoring the treatment plan to the patient’s specific condition is key to optimizing outcomes and preserving joint function.
Nutritional Support & Supplementation for Cartilage Maintenance
Nutrition plays a pivotal role in maintaining the health of cartilage. A well-balanced diet rich in essential vitamins, minerals, and bioactive compounds supports the synthesis and maintenance of the extracellular matrix and reduces inflammation. In addition, specific supplements can enhance cartilage repair and slow degenerative processes.
Essential Vitamins and Minerals
- Vitamin C:
Critical for collagen synthesis, vitamin C helps maintain the structural integrity of cartilage. Its antioxidant properties also protect chondrocytes from oxidative damage. - Vitamin D:
Vitamin D is essential for calcium homeostasis and bone health, indirectly supporting cartilage by promoting a strong skeletal framework. - B Vitamins:
Vitamins B6, B12, and folate play a role in cellular metabolism and may help reduce levels of homocysteine, a compound associated with cartilage and vascular damage. - Calcium and Magnesium:
These minerals are fundamental for bone and cartilage health, contributing to proper mineralization and cellular function.
Omega-3 and Other Polyunsaturated Fatty Acids
- Omega-3 Fatty Acids:
Found in fish oil and flaxseed, omega-3s have potent anti-inflammatory properties. They help reduce cartilage degradation by modulating inflammatory mediators. - Additional Polyunsaturated Fatty Acids:
These essential fats improve cell membrane fluidity and may support the overall metabolic health of cartilage tissue.
Herbal Supplements and Natural Compounds
- Turmeric (Curcumin):
Curcumin has well-documented anti-inflammatory effects and may help reduce joint pain and cartilage degradation in inflammatory conditions. - Boswellia Serrata:
This herb is known for its ability to inhibit pro-inflammatory enzymes, thereby reducing joint inflammation and potentially slowing cartilage damage. - Ginger:
Ginger’s anti-inflammatory properties can contribute to improved joint function and cartilage protection.
Enzymes and Antioxidants
- Bromelain:
An enzyme derived from pineapple, bromelain possesses anti-inflammatory and pain-relieving properties that may benefit joint health. - Coenzyme Q10 (CoQ10):
As an antioxidant, CoQ10 protects cells from oxidative stress and supports energy production, which is essential for the maintenance of cartilage. - N-acetylcysteine (NAC):
NAC is a precursor to glutathione, a critical antioxidant that helps maintain cellular redox balance in chondrocytes.
Hormonal Support
- DHEA (Dehydroepiandrosterone):
This hormone may support cartilage metabolism and reduce inflammation, contributing to overall joint health. - Melatonin:
Beyond its role in regulating sleep, melatonin offers antioxidant benefits that help protect cartilage from oxidative damage.
Incorporating these nutritional strategies and targeted supplements into your daily routine can provide a robust foundation for cartilage health. A balanced diet combined with appropriate supplementation not only supports cartilage integrity but also contributes to overall joint function and mobility.
Lifestyle Strategies for Preserving Cartilage Function
Maintaining healthy cartilage is not only about treatment and nutrition—it also requires proactive lifestyle choices. Adopting habits that reduce stress on joints and support overall physical well-being can help preserve cartilage and prevent premature degeneration.
Weight Management and Exercise
- Healthy Weight:
Maintaining an optimal body weight is crucial because excess weight places additional stress on joints, accelerating cartilage wear. A balanced diet and regular exercise help manage weight effectively. - Low-Impact Exercise:
Activities such as swimming, cycling, and walking are ideal for strengthening the muscles around joints without putting undue pressure on cartilage. These exercises improve joint stability and support cartilage by enhancing blood flow and nutrient delivery. - Strength Training and Flexibility:
Incorporating resistance exercises and stretching routines can help maintain muscle strength and joint mobility, reducing the likelihood of cartilage injury.
Joint Protection and Ergonomics
- Proper Body Mechanics:
Using correct posture and body mechanics during daily activities and exercise can minimize unnecessary stress on joints. Ergonomic adjustments in the workplace and at home can also protect cartilage. - Supportive Footwear:
Wearing shoes that provide adequate cushioning and support can help reduce the impact on lower extremity joints, preserving cartilage over time.
Avoidance of Harmful Substances
- Smoking Cessation:
Smoking is associated with reduced blood flow and impaired nutrient delivery to cartilage, hindering its ability to repair. Quitting smoking is one of the most beneficial steps for overall joint health. - Moderate Alcohol Consumption:
Excessive alcohol intake can contribute to systemic inflammation and negatively affect joint health. Moderation is key to preserving cartilage function.
Stress Management and Rest
- Stress Reduction:
Chronic stress can lead to elevated levels of inflammatory hormones such as cortisol, which may exacerbate cartilage degradation. Mindfulness practices, meditation, and yoga can help manage stress levels effectively. - Adequate Sleep:
Sleep is essential for the body’s natural repair processes. Ensuring you get enough quality sleep each night supports the regeneration of cartilage and overall recovery.
Regular Health Monitoring
- Periodic Check-Ups:
Regular medical examinations can help detect early signs of cartilage deterioration or joint issues. Early intervention is crucial for preventing long-term damage. - Personalized Exercise and Nutrition Plans:
Working with healthcare professionals to develop tailored plans that address individual risk factors can lead to better long-term outcomes for joint and cartilage health.
By integrating these lifestyle practices into daily routines, individuals can significantly support cartilage health. These proactive measures, in conjunction with proper medical care, create a strong foundation for maintaining joint function and overall mobility throughout life.
Educational Resources & References
Staying informed about cartilage health and related conditions is essential for both patients and healthcare professionals. A variety of reputable sources provide in-depth insights, up-to-date research findings, and practical guidance for managing cartilage disorders.
Recommended Books
- “Principles of Cartilage Repair” by W. Hogendoorn:
This book offers comprehensive insights into the biology of cartilage, innovative repair techniques, and the latest advances in regenerative medicine. - “Arthritis: What Exercises Work” by Dava Sobel and Arthur C. Klein:
A practical guide focusing on exercises that promote joint and cartilage health, with step-by-step instructions and illustrations. - “The Arthritis Cure” by Jason Theodosakis:
This resource explores lifestyle changes, nutritional strategies, and supplements that can help manage arthritis and support cartilage integrity.
Academic Journals
- Journal of Orthopaedic Research:
This peer-reviewed journal publishes high-quality studies on musculoskeletal biology, cartilage repair, and joint degeneration. - Osteoarthritis and Cartilage:
A specialized journal focusing on cartilage research and the pathophysiology of joint disorders, including new therapeutic interventions.
Digital Tools and Mobile Apps
- MyFitnessPal:
A comprehensive app that tracks diet and exercise, helping users maintain a balanced lifestyle that supports joint and cartilage health. - MapMyWalk:
Encourages regular physical activity by tracking walking routes and distances, promoting cardiovascular and joint health. - Jointfully:
Designed specifically for individuals with arthritis, this app offers symptom tracking, medication reminders, and tailored exercise tips to support cartilage and joint function.
These trusted resources provide valuable information and practical tools for anyone seeking to enhance their understanding of cartilage health and its maintenance. Whether you are a patient or a professional, these references can offer guidance and up-to-date insights on managing cartilage-related conditions.
Frequently Asked Questions About Cartilages
What is cartilage and why is it important?
Cartilage is a specialized connective tissue that provides flexible support, cushions joints, and maintains structural integrity in various parts of the body. Its unique composition helps reduce friction and absorb shock, which is crucial for movement and overall joint health.
How does cartilage differ from bone?
Unlike bone, cartilage is avascular and has a high water content, making it more flexible but less capable of self-repair. Cartilage relies on diffusion from surrounding tissues for nutrients, whereas bone has its own blood supply, allowing for more robust regeneration.
What are the most common cartilage disorders?
Common cartilage disorders include osteoarthritis, rheumatoid arthritis, chondromalacia patellae, intervertebral disc degeneration, and traumatic cartilage injuries. These conditions can lead to joint pain, reduced mobility, and functional impairment.
How is cartilage damage diagnosed?
Cartilage damage is diagnosed through a combination of clinical assessments, patient history, imaging techniques such as X-rays and MRI, and sometimes invasive procedures like arthroscopy or biopsy to directly evaluate the cartilage tissue.
What lifestyle changes can help maintain healthy cartilage?
Maintaining a healthy weight, engaging in low-impact exercise, following a balanced diet rich in antioxidants, avoiding smoking, and managing stress are key lifestyle changes that support cartilage health and slow degeneration.
Disclaimer:
The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a healthcare provider for personalized guidance.
If you found this guide helpful, please share it on Facebook, X (formerly Twitter), or your preferred social media platform to help spread awareness about cartilage health and joint wellness.


