Introduction to Central Serous Retinopathy
Central Serous Retinopathy (CSR) is a retinal condition characterized by the accumulation of fluid beneath the retina, particularly beneath the macula, which is responsible for central vision. This fluid buildup causes a localized retinal detachment, resulting in blurred vision, distorted images (metamorphopsia), and a central dark spot (scotoma). CSR primarily affects adults aged 20 to 50, with a higher prevalence in men. Stress, steroids, and certain medical conditions are all known risk factors. While many cases resolve spontaneously, recurrent and chronic forms can cause long-term vision problems, necessitating a thorough understanding and management of the condition.
Central Serous Retinopathy: Detailed Overview
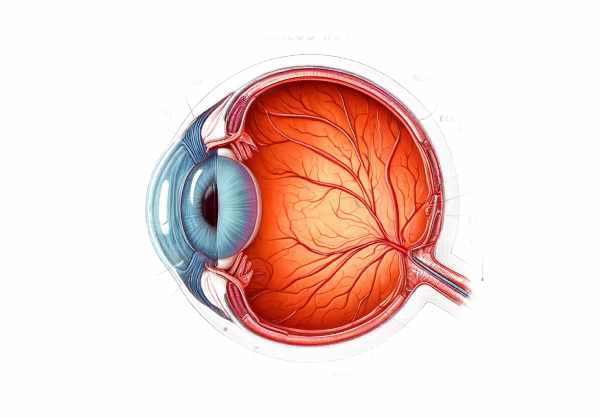
Central Serous Retinopathy (CSR), also known as Central Serous Chorioretinopathy (CSCR), is the leakage of fluid from the choroid, the eye’s vascular layer, into the space beneath the retina. This causes the neurosensory retina to detach from the underlying retinal pigment epithelium (RPE), primarily affecting the macula. The exact pathophysiology of CSR is unknown, but several key factors influence its development and progression.
Pathophysiology
The underlying mechanism of CSR is RPE dysfunction, which normally acts as a barrier and pump to prevent fluid accumulation beneath the retina. When the RPE’s function is compromised, fluid from the choroid leaks into the subretinal space, causing detachment. Factors associated with RPE dysfunction include:
- Choroidal Hyperpermeability: Increased permeability of the choroidal blood vessels can cause excessive fluid leakage, exceeding the RPE’s ability to manage the fluid.
- Corticosteroids: Systemic and topical steroid use has been linked to CSR, most likely due to their effects on vascular permeability and stress response.
- Psychological Stress: Excessive stress and associated catecholamine release can alter vascular tone and permeability, contributing to the development of CSR.
- Hormonal Influence: CSR has been linked to elevated levels of cortisol and other stress-related hormones, which explains why it is more common in people who work in high-stress jobs or live stressful lifestyles.
Risk factors
There are several risk factors associated with CSR, including:
- Age and Gender: CSR primarily affects males aged 20 to 50 years. The male-to-female ratio ranges between 6:1 and 10:1.
- Psychological Stress: People with high levels of stress are more likely to develop CSR.
- Steroid Use: Both systemic and local steroid treatments elevate the risk of CSR.
- Type A Personality: People with type A personalities are more likely to engage in CSR because they are competitive and have a strong sense of urgency.
- Medical Conditions: Hypertension, obstructive sleep apnea, and autoimmune diseases are all associated with an increased risk of CSR.
- Medications: Some medications, such as antihistamines and psychotropic drugs, may contribute to the development of CSR.
Clinical Presentation.
The onset of CSR is frequently sudden, with patients typically reporting one or more of the following symptoms.
- Blurred Vision: Visual acuity is often significantly reduced, particularly in the central vision.
- Metamorphopsia: Objects may appear distorted, with straight lines becoming wavy or bent.
- Central Scotoma: Patients frequently report having a dark or gray spot in their central vision.
- Micropsia: Objects may appear smaller than they actually are.
- Color Desaturation: Colors may appear less vibrant, making it difficult for patients to distinguish between similar hues.
Types of CSR
CSR can be classified into two primary types based on its duration and frequency:
- Acute CSR: This condition usually goes away on its own after three to six months. Vision usually returns to normal or near-normal levels, but some patients may experience residual visual disturbances.
- Chronic CSR: Chronic CSR, also known as diffuse retinal pigment epitheliopathy (DRPE), lasts more than six months and can result in permanent retinal damage and significant visual impairment. It frequently involves multiple episodes or ongoing fluid leakage.
Impact on vision
The impact of CSR on vision varies greatly. Many patients experience spontaneous resolution and significant visual recovery, but others may have persistent symptoms or recurrent episodes. Chronic CSR can cause permanent RPE changes and photoreceptor damage, resulting in long-term visual deficits.
Prognosis
The prognosis for CSR is generally positive, particularly in acute cases. Approximately 80-90% of acute CSR cases resolve spontaneously within a few months, resulting in significant improvement in visual acuity. However, the recurrence rate is high, with approximately 30-50% of patients having multiple episodes. Chronic CSR presents a greater challenge because it can cause permanent retinal damage and persistent visual impairment.
Central Serous Retinopathy Prevention Tips
- Stress Management – Use stress-reduction techniques like mindfulness, meditation, and yoga to reduce overall stress. Regular exercise, adequate sleep, and a healthy work-life balance can all help you manage stress better.
- Cautious Steroid Use – Consult a healthcare professional before using corticosteroids. If you are taking steroids for a chronic condition, talk to your doctor about alternative treatments to reduce the risk of CSR.
- Schedule regular comprehensive eye exams, especially if you have a high risk of CSR from stress or steroid use. Early detection can aid in managing the condition before it causes significant vision loss.
- Maintain a healthy lifestyle through a balanced diet, regular exercise, and avoiding smoking. These habits improve overall vascular health and lower the risk of ocular conditions like CSR.
- Monitor Vision Changes – Be aware of any sudden changes in vision, such as blurriness, distortion, or dark spots. If you experience any of these symptoms, seek medical attention right away because early intervention can improve outcomes.
- Manage Medical Conditions – Control chronic conditions like hypertension and sleep apnea through treatment and lifestyle modifications. Proper management of these conditions can lower the risk of CSR.
- Avoid high stress situations. If possible, avoid stressful environments or situations. Learn how to cope with unavoidable stressors effectively.
- Educate Yourself: Stay informed about CSR and its risk factors. Understanding the condition allows you to take proactive measures to prevent its occurrence and effectively manage it if it does develop.
Diagnostic methods
Central serous retinopathy (CSR) is diagnosed using a combination of patient history, clinical examination, and advanced imaging techniques. The following diagnostic methods are widely used:
Fundus examination
A thorough fundus examination with a slit-lamp biomicroscope and fundus lens is required. The ophthalmologist looks for subretinal fluid, which is visible as a raised area of the retina. A round, well-defined serous detachment of the retina is a characteristic of CSR.
Optical coherence tomography (OCT)
OCT is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the retina. It is considered the gold standard for diagnosing CSR. OCT allows for the visualization of the serous detachment, measurement of its height and extent, and evaluation of any retinal pigment epithelium (RPE) changes. Enhanced depth imaging OCT (EDI-OCT) is especially useful for determining choroidal thickness and identifying choroidal abnormalities linked to CSR.
fluorescein angiography (FA)
In fluorescein angiography, a fluorescent dye is injected into the bloodstream and photographed as it travels through the retinal vessels. FA aids in determining the point of leakage from the choroidal circulation into the subretinal space. The classic “smokestack” or “inkblot” pattern of dye leakage on FA is typical of CSR.
Indocyanine green angiography (ICGA)
ICGA visualizes the choroidal vasculature with indocyanine green dye. This technique is especially useful in chronic or recurring cases of CSR because it detects areas of choroidal hyperpermeability and distinguishes CSR from other conditions like polypoidal choroidal vasculopathy (PCV).
Fundus Autofluorescence(FAF)
FAF imaging detects areas of abnormal autofluorescence, which aids in assessing the health of the RPE. In CSR, hyperautofluorescence corresponds to damaged RPE, which can provide information about the condition’s chronicity and severity.
Multi-modal Imaging
Combining different imaging modalities can provide a more complete assessment of CSR. Multimodal imaging, which includes OCT, FA, ICGA, and FAF, provides detailed information about retinal and choroidal changes, allowing for more accurate diagnosis and management planning.
These diagnostic methods, which range from clinical examination to advanced imaging techniques, allow ophthalmologists to accurately diagnose CSR, track its progression, and tailor treatment strategies effectively.
Central Serous Retinopathy Treatment Methods
The treatment of Central Serous Retinopathy (CSR) aims to reduce subretinal fluid, improve visual acuity, and prevent recurrences. Standard treatments and emerging therapies include the following:
Observation
In many cases of acute CSR, observation is the preferred method. Approximately 80-90% of acute CSR cases resolve spontaneously in three to six months. During this time, patients are monitored on a regular basis to assess subretinal fluid resolution and visual acuity recovery.
Laser photocoagulation
Laser photocoagulation may be used in cases where the condition does not resolve spontaneously or in patients with recurrent CSR. This treatment entails applying a focused laser to the leakage site identified on FA. Laser photocoagulation helps to seal the leak and reduce subretinal fluid accumulation. However, this method can result in permanent scarring and is usually reserved for extrafoveal leakage to avoid central vision loss.
Photodynamic therapy (PDT)
PDT with verteporfin is a successful treatment for chronic or recurring CSR. PDT involves injecting verteporfin, a photosensitizing agent, into the bloodstream, which is then activated by a low-energy laser. This treatment focuses on abnormal choroidal vessels, reducing choroidal hyperpermeability and subretinal fluid. PDT is especially useful for treating CSR with subfoveal leakage, which reduces damage to the surrounding retina.
Anti-VEGF Therapies
Although anti-VEGF (vascular endothelial growth factor) therapy is commonly used to treat conditions such as age-related macular degeneration, it has also been investigated as a treatment for CSR. Anti-VEGF injections, such as bevacizumab and ranibizumab, can help reduce choroidal vascular permeability and subretinal fluid. However, the efficacy of anti-VEGF therapy in CSR is still being investigated, and it is not yet considered standard treatment.
Oral medications
Oral mineralocorticoid receptor antagonists, such as spironolactone and eplerenone, have shown promise in the treatment of CSR. These drugs reduce choroidal vascular permeability and fluid leakage by blocking cortisol’s effects on the choroidal vessels. Clinical trials have shown that these medications improve visual acuity and reduce subretinal fluid levels.
Stress management
Because psychological stress is a known risk factor for CSR, stress management techniques are an important component of treatment. Patients are encouraged to practice stress-reduction techniques like mindfulness, meditation, and regular exercise. In some cases, counseling or therapy may be suggested to address underlying stressors.
Emerging Therapies
Research into new CSR treatments is ongoing. Potential treatments include:
- Riboflavin Phototherapy: This experimental treatment combines riboflavin (vitamin B2) and ultraviolet light to reduce choroidal permeability and subretinal fluid.
- Gene Therapy: Gene therapy approaches seek to alter the expression of genes implicated in choroidal hyperpermeability and RPE dysfunction.
- Stem Cell Therapy: Stem cell transplantation is being researched for its ability to regenerate damaged retinal tissue and restore function in cases of chronic CSR.
To summarize, the treatment of CSR consists of observation, laser photocoagulation, PDT, anti-VEGF therapy, oral medications, stress management, and emerging therapies. Early intervention and regular monitoring are critical for improving visual outcomes and avoiding recurrence.
Trusted Resources
Books
- “Retinal Vascular Disease” by A.M. Joussen, T.W. Gardner, B. Kirchhof, S.J. Ryan
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski
- “Retina” by Stephen J. Ryan, SriniVas R. Sadda






