What is Chlamydial Conjunctivitis?
Chlamydial conjunctivitis, or inclusion conjunctivitis, is an eye infection caused by the bacterium Chlamydia trachomatis. This condition can affect people of any age, but it is especially common in neonates and sexually active adults. Chlamydial conjunctivitis is spread by direct contact with infectious secretions from the eyes or genitals. If the mother has a genital chlamydia infection, the infection is most likely to be acquired during childbirth. In adults, it is frequently associated with sexually transmitted infections (STIs).
Chlamydial conjunctivitis symptoms range from mild to severe and include redness, discharge, and eye irritation. If left untreated, this condition can result in corneal scarring and vision impairment. Understanding the causes, transmission, clinical manifestations, and potential complications of chlamydial conjunctivitis is critical for effective prevention and treatment.
Key Insights on Chlamydial Conjunctivitis
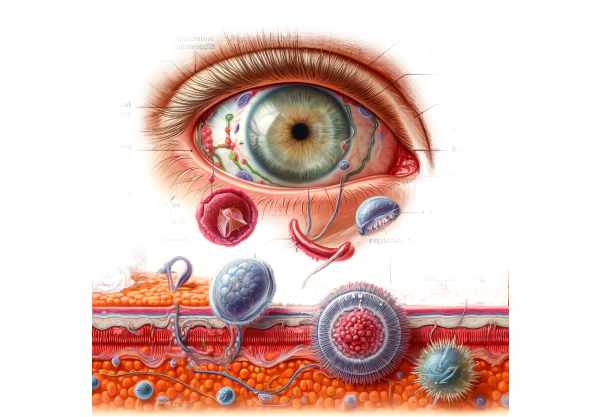
Chlamydial conjunctivitis is caused by the obligate intracellular bacterium Chlamydia trachomatis, which infects epithelial cells. This bacterium has a distinct biphasic lifecycle that includes an infectious elementary body (EB) and a replicative reticulate body (RB). The bacterium is transmitted by EBs, whereas RBs facilitate intracellular replication.
Epidemiology
Chlamydial conjunctivitis is a major public health concern worldwide. It is a frequent cause of neonatal conjunctivitis, also known as ophthalmia neonatorum. The prevalence of neonatal chlamydial conjunctivitis varies by region, with higher rates found in areas where genital chlamydia infections are common. The condition is more common in sexually active adults, especially those who have had multiple sexual partners or have a history of STIs.
Transmission
The primary mode of transmission of Chlamydia trachomatis causing conjunctivitis varies between neonates and adults. In neonates, the infection is usually acquired during the passage through the birth canal of an infected mother. This vertical transmission exposes the neonate’s eyes to the bacterium, which causes conjunctivitis within the first few weeks of life.
Chlamydial conjunctivitis in adults is frequently associated with genital infections. The bacterium can enter the eyes through direct contact with infected genital secretions, either by autoinoculation (self-infection) or sexual contact. Sharing contaminated towels or cosmetics can also help spread the infection.
Clinical Manifestations
The clinical presentation of chlamydial conjunctivitis varies depending on the age of the affected person and the severity of the infection. Common symptoms include:
- Redness and Irritation: Affected people frequently report redness, itching, and a gritty sensation in their eyes.
- Discharge: The eyes typically produce a mucopurulent (mucus and pus) discharge, which can cause the eyelids to stick together, particularly when awake.
- Swelling: The conjunctiva and eyelids are frequently swollen.
- Photophobia: In more severe cases, sensitivity to light may occur.
Chlamydial conjunctivitis in neonates usually appears within the first two weeks of life. The symptoms can range from mild conjunctival redness to severe inflammation with significant discharge. If left untreated, it can result in complications like pneumonia.
In adults, symptoms may appear more gradually. Chronic cases can develop if the infection is not adequately treated, resulting in recurring symptoms and potential complications such as conjunctival and corneal scarring.
Pathophysiology
Chlamydial conjunctivitis is caused by Chlamydia trachomatis invading conjunctival epithelial cells in the eye. When EBs enter epithelial cells, they differentiate into RBs, which replicate within the host cell. The RBs then convert back into EBs, which are released when the cell ruptures, infecting neighboring cells and perpetuating the cycle.
The immune response to infection helps to cause the disease’s clinical manifestations. Inflammatory mediators released by infected and immune cells cause the characteristic redness, swelling, and discharge associated with conjunctivitis. Chronic inflammation can cause scarring and other long-term effects.
Complications
Untreated chlamydial conjunctivitis can cause a variety of complications, some of which can have long-term implications for vision and ocular health. The complications include:
- Corneal Scarring: Chronic inflammation can cause scarring of the cornea, potentially impairing vision.
- Chronic Conjunctivitis: Poorly treated infections can become chronic, resulting in recurring symptoms and an increased risk of complications.
- Pneumonia in Neonates: Infants with chlamydial conjunctivitis are at risk of developing chlamydial pneumonia, which can be severe and necessitate immediate treatment.
- Trachoma: In endemic areas, multiple infections with Chlamydia trachomatis can result in trachoma, a chronic condition that can cause blindness.
Prognosis
Individuals with chlamydial conjunctivitis have a good prognosis if they receive appropriate treatment. Most cases are resolved without long-term complications, particularly when diagnosed and treated promptly. However, delayed or inadequate treatment can result in chronic infection and complications like corneal scarring and vision loss.
Essential Preventive Tips
Chlamydial conjunctivitis is prevented through strategies that reduce the risk of infection and transmission. Here are some important preventative measures:
- Pregnant Women Screening and Treatment: Regular Chlamydia trachomatis screening during prenatal care, as well as treatment for infected women, can significantly reduce the risk of neonatal chlamydial conjunctivitis.
- Safe Sexual Practices: Consistent and proper condom use during sexual activity can help prevent genital chlamydia infections, lowering the risk of autoinoculation to the eyes.
- Hygiene Practices: Good hygiene, such as frequent handwashing and not sharing towels, cosmetics, or contact lenses, can help prevent the infection from spreading.
- Prompt Treatment of STIs: Seeking early treatment for any suspected or confirmed STI can help to avoid complications and reduce the risk of spreading the infection to others.
- Education and Awareness: Raising public awareness of the dangers and spread of chlamydial infections can encourage preventive behaviors and early treatment.
- Ocular Hygiene for Neonates: Providing proper ocular hygiene and care to newborns, particularly those born to mothers with known chlamydial infections, can help prevent conjunctivitis.
Diagnostic methods
Chlamydial conjunctivitis is diagnosed using a combination of clinical and laboratory tests. Standard diagnostic techniques focus on detecting Chlamydia trachomatis in conjunctival specimens.
- Nucleic Acid Amplification Tests (NAAT): NAATs are regarded as the gold standard for detecting chlamydial infections due to their high sensitivity and specificity. These tests detect the genetic material of Chlamydia trachomatis in conjunctival swabs, allowing for precise and quick diagnosis.
- Culture: Despite its complexity and time requirements, culture is still a reliable method for diagnosing chlamydial conjunctivitis. Conjunctival swabs are placed on specialized media that promote the growth of Chlamydia trachomatis. Positive cultures indicate the presence of the bacterium, though the results may take several days.
- Direct Fluorescent Antibody (DFA) Staining: This method involves staining conjunctival smears with fluorescent antibodies specific to Chlamydia trachomatis. The bacterium’s presence can be seen using a fluorescence microscope. DFA staining is specific, but less sensitive than NAATs.
Innovative Diagnostic Techniques
- Point-of-Care Testing: Recent advances have resulted in the creation of rapid point-of-care tests for chlamydial infections. These tests, which can be performed in a clinical setting, yield results in minutes, allowing for prompt diagnosis and treatment.
- Multiplex PCR Assays: These tests can detect multiple pathogens, including Chlamydia trachomatis, in a single sample. Multiplex PCR assays improve diagnostic efficiency by detecting co-infections, which are important for proper management.
- Next-Generation Sequencing (NGS): NGS technologies provide comprehensive genomic analysis, allowing the detection of Chlamydia trachomatis and other potential pathogens. Though NGS is currently more common in research settings, it shows promise for future clinical applications.
Treatments for Chlamydial Conjunctivitis
Chlamydial conjunctivitis is treated with antimicrobials to eliminate the infection and prevent complications. Standard treatment regimens vary according to the patient’s age and the severity of the infection.
- Neonates: – Oral Erythromycin: For neonates with chlamydial conjunctivitis, oral erythromycin is often prescribed. The typical dosage is 50 mg/kg per day, divided into four doses over 14 days. This treatment effectively eliminates the infection and prevents associated pneumonia.
• Topical Antibiotics: Although oral antibiotics are preferred, topical antibiotics, such as erythromycin ointment, can be used as an adjunct to reduce ocular discharge and inflammation. - Adults: – Oral Azithromycin: A single dose of 1 gram is highly effective in treating chlamydial conjunctivitis in adults. This antibiotic is popular because of its simplicity and high compliance rate.
- Oral Doxycycline: Alternatively, oral doxycycline (100 mg twice daily for 7 days) may be used. Doxycycline is effective, but requires a longer treatment period and strict adherence to dosing schedules.
- Topical Antibiotics: Topical antibiotics, such as tetracycline or erythromycin ointment, can be used in conjunction with oral antibiotics to increase treatment efficacy.
Innovative and Emerging Therapies
- Azithromycin Gel: Azithromycin gel is currently being researched for topical use. This gel has the potential to deliver high local antibiotic concentrations while minimizing systemic absorption, potentially reducing side effects and improving patient compliance.
- Antimicrobial Peptides: In preclinical studies, these peptides demonstrated the ability to target and destroy bacterial membranes. As research advances, antimicrobial peptides may emerge as a new treatment option for chlamydial conjunctivitis.
- Probiotics: Emerging evidence suggests that probiotics may help boost the immune system and reduce inflammation in ocular infections. While still experimental, probiotics could be used as an adjunct treatment for chlamydial conjunctivitis.
- Vaccines: Research into vaccines for Chlamydia trachomatis is currently underway. A successful vaccine would mark a significant step forward in preventing not only genital chlamydia infections, but also related ocular conditions like chlamydial conjunctivitis.
Trusted Resources
Books
- “Ocular Infection: Diagnosis and Treatment” by William R. Freeman and Daniel M. Albert
- “Conjunctivitis: Symptoms, Diagnosis and Treatment” by Albert J. Augustin and Oliver Stange
- “Neonatal and Infant Ophthalmology” by Scott E. Olitsky and Leonard B. Nelson






