Introduction
Chronic Progressive External Ophthalmoplegia (CPEO) is a rare mitochondrial disorder marked by gradual weakness of the muscles that control eye movements. This condition usually manifests in adulthood, but symptoms can appear in childhood or adolescence. CPEO causes progressive difficulty moving the eyes and eyelids, resulting in symptoms like drooping eyelids (ptosis) and limited eye movements. Over time, the condition can have a significant impact on visual function and quality of life. Understanding CPEO entails investigating its genetic basis, clinical presentation, and potential complications, which are critical for effective management and support.
Chronic Progressive External Ophthalmoplegia Insights
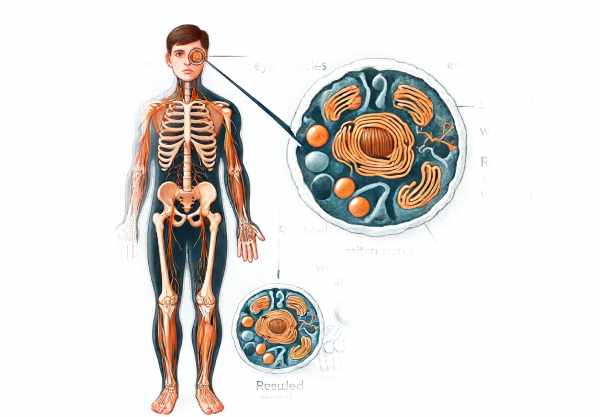
Chronic Progressive External Ophthalmoplegia (CPEO) is a complicated and multifaceted condition that affects the muscles that control eye movements and, to a lesser extent, other skeletal muscles. CPEO is a mitochondrial disorder caused by defects in the mitochondria, which are the energy-producing structures found within cells. These defects reduce cellular energy production, resulting in muscle weakness and other systemic symptoms.
Genetic Basis and Pathophysiology
CPEO is primarily caused by mutations in mitochondrial DNA (mtDNA) or nuclear DNA (nDNA), which impair mitochondrial function. Mitochondrial DNA mutations are passed down from mother to child, whereas nuclear DNA mutations can be inherited in a variety of ways, including autosomal dominant, autosomal recessive, or sporadic.
The most common mtDNA mutations associated with CPEO are single large-scale deletions and point mutations. These genetic changes disrupt the production of proteins required for the mitochondrial respiratory chain, reducing the cell’s ability to produce adenosine triphosphate (ATP), the cell’s primary energy currency. As a result, tissues with high energy demands, such as muscle and nerve tissue, are especially vulnerable.
Clinical Manifestations
CPEO causes a variety of symptoms, primarily affecting the ocular muscles but frequently extending to other muscle groups and organ systems. The hallmark symptoms include:
- Ptosis: One of the first and most noticeable symptoms of CPEO is bilateral ptosis, or drooping of the eyelids. This is due to progressive weakness of the levator palpebrae muscles.
- Ophthalmoplegia: Patients gradually lose the ability to move their eyes in all directions due to extraocular muscle weakness. This causes difficulty tracking objects, double vision (diplopia), and a distinctive fixed gaze.
- Facial Weakness: Some people may have weakness in their facial muscles, resulting in a mask-like expression.
- Systemic Involvement: While CPEO primarily affects ocular muscles, it may also affect skeletal muscles and other systems. In severe cases, symptoms can include mild proximal muscle weakness, exercise intolerance, dysphagia (difficulty swallowing), and involvement of respiratory muscles.
Differential Diagnosis
Diagnosing CPEO requires distinguishing it from other conditions that may cause similar symptoms. Differential diagnosis includes:
- Myasthenia Gravis is an autoimmune disorder that affects the neuromuscular junction, causing fluctuating muscle weakness, particularly in the ocular and facial muscles.
- Oculopharyngeal Muscular Dystrophy is a genetic disorder characterized by progressive ptosis, dysphagia, and proximal muscle weakness.
- Kearns-Sayre Syndrome is a mitochondrial disorder characterized by CPEO, pigmentary retinopathy, and cardiac conduction defects.
- Thyroid Eye Disease is an autoimmune condition linked to thyroid dysfunction that causes inflammation and swelling of the eye muscles, resulting in similar ocular symptoms.
Pathology and Progression
CPEO’s pathogenesis involves a progressive decline in mitochondrial function caused by accumulated mutations in mtDNA or nDNA. As the disease progresses, the energy deficit in muscle cells causes fiber atrophy, fibrosis, and eventually muscle failure.
- Mitochondrial Dysfunction: The primary defect in CPEO is an impaired mitochondrial respiratory chain. This reduces ATP production and increases the production of reactive oxygen species (ROS), resulting in oxidative damage to cellular components.
- Muscle Fiber Changes: Histological examination of affected muscles frequently reveals ragged red fibers, which indicate abnormal mitochondrial proliferation. These fibers exhibit defective oxidative phosphorylation, which contributes to muscle weakness.
- Progression: The progression of CPEO is usually slow but steady. Symptoms worsen over years and decades, resulting in significant disability. However, the rate of progression and severity of symptoms can differ greatly between individuals.
Complications
CPEO can cause a variety of complications, primarily due to its progressive nature and systemic involvement.
- Visual Impairment: Severe ophthalmoplegia can cause significant visual disturbances, including diplopia and a limited visual field due to ptosis.
- Respiratory Issues: In severe cases, respiratory muscle involvement can cause breathing difficulties and increase the risk of respiratory infections.
- Cardiac Involvement: Some patients may develop cardiac conduction defects or cardiomyopathy, necessitating monitoring and treatment.
- Quality of Life: The chronic and progressive nature of CPEO can have a significant impact on one’s quality of life, resulting in physical limitations, social isolation, and psychological distress.
Impact on Daily Life
The effects of CPEO on daily life are profound. Patients frequently have to adapt to progressive visual and muscular limitations. Simple tasks such as reading, driving, and maintaining eye contact can be difficult due to ptosis and ophthalmoplegia. Muscle weakness may require the use of mobility aids or assistive devices during daily activities.
Social and psychological factors are also significantly impacted. Ptosis’ visible symptoms, including facial weakness, can cause self-consciousness and social withdrawal. The disease’s chronic nature, combined with the lack of a definitive cure, can exacerbate anxiety and depression.
Understanding the multifaceted nature of chronic progressive external ophthalmoplegia is critical for developing effective management strategies and assisting patients in dealing with the condition. Continued research into the genetic and molecular mechanisms underlying CPEO shows promise for future therapeutic advances.
Prevention Tips
Chronic Progressive External Ophthalmoplegia prevention strategies include early detection, risk factor mitigation, and overall health promotion. While genetic factors cannot be changed, certain measures can help to better manage the condition.
- Genetic counseling:
- Families with a history of CPEO should seek genetic counseling to better understand the risks and inheritance patterns. This can help you make informed reproductive decisions.
- Regular Medical Check-Ups:
- Routine medical examinations, including ophthalmologic evaluations, are critical for early detection and monitoring of symptoms. Regular check-ups can aid in managing complications and slowing disease progression.
- A Healthy Lifestyle:
- Eat a well-balanced, antioxidant-rich diet to promote mitochondrial health. Regular physical activity, when tolerated, can help to maintain muscle strength and overall health.
- Preventing Mitochondrial Toxins:
- Limit your exposure to known mitochondrial toxins, such as certain medications (e.g., aminoglycoside antibiotics) and environmental toxins that can exacerbate mitochondrial dysfunction.
- Managing coexisting conditions:
- Manage other medical conditions that can impair mitochondrial health, such as diabetes and thyroid problems. Effective management of these conditions can reduce the extra strain on the mitochondria.
- Eye protection:
- Wear protective eyewear to keep your eyes safe from injury or excessive strain. This can help to maintain remaining eye function and avoid further complications.
- Psychological support:
- Seek psychological counseling or support groups to address the emotional and psychological difficulties associated with CPEO. Mental health support is essential for dealing with chronic illnesses.
- Research Participation:
- Consider taking part in clinical trials or research studies on mitochondrial diseases. This can help to advance our understanding of and treatment for CPEO while also providing access to emerging therapies.
Diagnostic methods
Chronic Progressive External Ophthalmoplegia (CPEO) is diagnosed using a combination of clinical evaluation, genetic testing, and advanced imaging techniques to accurately identify the condition and underlying causes.
Clinical Evaluation
A neurologist or ophthalmologist will typically conduct a thorough clinical evaluation to begin the diagnostic process. The key components of this evaluation are:
- Patient History: Provide a detailed history of symptoms, including the onset and progression of ptosis and ophthalmoplegia, as well as any family history of these conditions.
- Physical Examination: A thorough examination that focuses on ocular motility, eyelid function, and muscular strength. Ptosis, restricted eye movements, and other indications of muscle weakness are observed.
Genetic Testing
Genetic testing is critical for confirming the diagnosis of CPEO and determining the specific genetic mutations involved. This testing may include:
- Mitochondrial DNA Analysis: Detection of common mtDNA deletions and point mutations associated with CPEO. These mutations are identified using techniques like polymerase chain reaction (PCR) and next-generation sequencing (NGS).
- Nuclear DNA Testing: If mtDNA mutations are not detected, nuclear DNA testing can be used to identify mutations in nuclear genes involved in mitochondrial function.
Muscle Biopsy
A muscle biopsy can help diagnose CPEO. A small piece of muscle tissue, usually from the biceps or quadriceps, is collected for histological analysis during a biopsy. The key findings in CPEO include:
- Ragged Red Fibers: These abnormal muscle fibers, visible under special staining techniques, indicate mitochondrial proliferation and dysfunction.
- Cyclic Nucleotide Staining can reveal abnormal oxidative phosphorylation in muscle fibers.
Imaging Techniques
Advanced imaging techniques can help with the diagnosis and evaluation of CPEO.
- Magnetic Resonance Imaging (MRI): An MRI of the brain and orbits can rule out other neurological causes of ophthalmoplegia and determine the involvement of other cranial nerves.
- Electromyography (EMG): EMG measures electrical activity in muscles and can help distinguish between myopathic and neurogenic causes of muscle weakness.
Other Diagnostic Tools
Additional diagnostic tools that can help with the diagnosis of CPEO are:
- Lactic Acid Testing: High blood lactate levels may indicate mitochondrial dysfunction, as seen in CPEO.
- Electrocardiography (ECG): To detect cardiac conduction defects, which can occur in some cases of mitochondrial disease.
By combining these diagnostic methods, healthcare providers can accurately diagnose CPEO, assess its severity, and identify the underlying genetic causes, allowing for personalized treatment strategies.
Treating Chronic Progressive Ophthalmoplegia
atment for Chronic Progressive External Ophthalmoplegia (CPEO) focuses on symptom management, slowing disease progression, and improving quality of life. While there is no cure for CPEO, several treatments can help with symptoms and complications.
Medical Management
Medical management aims to alleviate symptoms and support mitochondrial function.
- Corticosteroids: Corticosteroids may be used in some cases to reduce inflammation and improve muscle strength, but their effectiveness varies.
- Vitamin and Coenzyme Supplements: Supplements containing coenzyme Q10 (CoQ10), riboflavin (vitamin B2), and other antioxidants may improve mitochondrial function and reduce oxidative stress.
Surgical Interventions
Surgical interventions can address specific symptoms related to CPEO:
- Ptosis surgery can improve vision and appearance. Common procedures include levator resection and frontalis suspension.
- Strabismus Surgery: Strabismus surgery can help patients with significant ophthalmoplegia who have misaligned their eyes and reduce double vision.
Physical Therapy
Physical therapy and rehabilitation are crucial in maintaining muscle strength and function.
- Oculomotor Exercises: Exercises that improve eye movement and coordination can be useful.
- General Physical Therapy: Customized exercise programs help maintain overall muscle strength and endurance, thereby mitigating the effects of systemic muscle weakness.
Innovative and Emerging Therapies
Research into mitochondrial diseases has resulted in the development of novel therapies that hold promise for CPEO:
- Gene Therapy: Experimental gene therapy approaches seek to correct specific genetic mutations that cause CPEO. This involves delivering healthy copies of genes to affected cells in order to restore normal mitochondrial function.
- Mitochondrial Replacement Therapy: This technique involves replacing damaged mitochondria with healthy ones from a donor egg, and it has shown promise in preclinical trials.
- Pharmacological Agents: New drugs that target mitochondrial biogenesis and function are being investigated. Elamipretide (MTP-131) is being investigated for its ability to improve mitochondrial function and muscle strength.
Supportive Measures
Patients with CPEO require supportive measures to manage symptoms and improve their quality of life.
- Assistive Devices: Eyeglasses with prism lenses can help manage double vision, and mobility aids can help with ambulation.
- Nutritional Support: Adequate nutrition and hydration are critical, particularly for patients with dysphagia or other gastrointestinal symptoms.
By combining these treatment strategies, healthcare providers can effectively manage CPEO symptoms, slow disease progression, and improve affected individuals’ quality of life.
Trusted Resources
Books
- Mitochondrial Medicine by Patrick F. Chinnery and Michelangelo Mancuso
- Mitochondrial Disorders in Neurology by Elsevier Health Sciences
- Understanding Mitochondrial Myopathies by Hans Spelbrink and Laurence Bindoff






