Introduction to Coats Disease
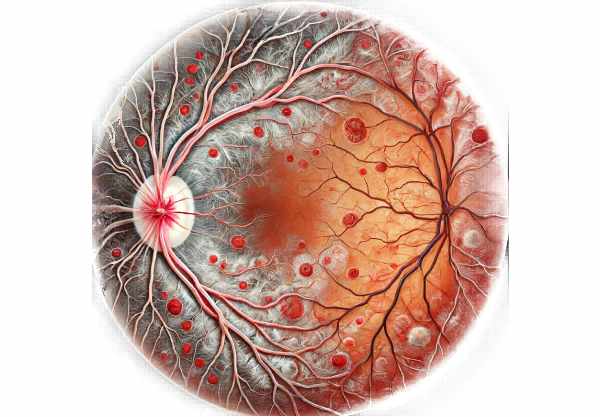
Coats Disease is a rare, non-hereditary eye disorder characterized by abnormal blood vessel development and leakage in the retina, resulting in retinal detachment and vision loss. This condition, which primarily affects young males, can cause unilateral vision impairment and is most commonly diagnosed in childhood or adolescence. Coat’s Disease is named after Scottish ophthalmologist George Coats, who first described it in 1908. The disease progresses through several stages, each with its own set of clinical features. Understanding the ocular manifestations of Coat’s Disease is critical for early detection and effective treatment, which aims to preserve vision and prevent complications.
Coat’s disease insights
Coat’s Disease, also called exudative retinitis or retinal telangiectasis, is a progressive retinal disorder that has serious consequences for vision and overall ocular health. This condition primarily affects the retina’s vascular system, causing a series of pathological changes that can seriously impair visual function.
Pathology and Etiology
Coat’s disease is characterized by abnormal development and dilation of retinal blood vessels, which results in telangiectasia (dilated capillaries) and aneurysms. These abnormal vessels are prone to leakage, which causes an accumulation of lipoproteinaceous exudates in the retina and subretinal space. This leakage can eventually cause retinal detachment, a serious complication that jeopardizes vision.
The exact etiology of Coat’s Disease is unknown, but it is thought to be idiopathic, which means it develops spontaneously without any known cause. Unlike many retinal disorders, Coat’s Disease has no genetic basis and is not linked to systemic diseases. Its sporadic nature implies that a combination of environmental and possibly unknown genetic factors may play a role in its development.
Clinical Stages and Manifestations
Coat’s Disease develops in stages, each with distinct clinical features and varying degrees of retinal involvement. The classification of these stages aids in understanding the severity and progression of the illness.
- Stage 1: Retinal Telangiectasia
- The presence of dilated retinal capillaries (telangiectasia) without significant exudation characterizes the early stages. Patients may be asymptomatic or exhibit mild visual disturbances.
- Stage 2 – Telangiectasia and Exudation:
- At this point, the abnormal vessels begin to leak, causing an accumulation of exudates in the retina. This exudation can thicken the retina and result in the formation of hard exudates, which are yellowish deposits made up of lipid-laden macrophages.
- Stage 3: Exudative Retinal Detachment
- Progressive leakage and fluid accumulation can result in retinal detachment. This stage is distinguished by the separation of the neurosensory retina from the underlying retinal pigment epithelium (RPE), which causes significant visual impairment.
- Stage 4—Total Retinal Detachment:
- In severe cases, the exudative process can result in total retinal detachment. At this point, patients may experience severe vision loss or blindness in the affected eye.
- Stage 5: Advanced End-Stage Disease
- The final stage of Coat’s disease is distinguished by chronic retinal detachment, retinal atrophy, and subretinal fibrosis. Chronic inflammation and scarring can cause the eye to appear phthisical (shrunken and nonfunctional).
Symptoms and Signs
The symptoms of Coat’s Disease differ depending on the stage and severity of the illness. Early stages may be asymptomatic or present with subtle visual changes, whereas advanced stages can result in significant visual impairment. Common symptoms include:
- Visual Disturbances: Patients may have blurred vision, decreased visual acuity, or metamorphopsia (distorted vision).
- Strabismus: Eye misalignment, also known as “crossed eyes,” can result from impaired vision in one eye.
- Leukocoria: A white or yellowish reflex in the pupil, also known as the “cat’s eye reflex,” is frequently an indicator of advanced disease with significant exudation or retinal detachment.
- Patients may experience floaters (small, dark shapes floating in their field of vision) and photopsia (flashes of light) as a result of vitreous traction and retinal changes.
Complications
Coat’s Disease can cause a variety of complications if not diagnosed and treated promptly. The most significant complications are:
- Retinal Detachment: The most serious complication, retinal detachment, can cause permanent vision loss if not treated immediately.
- Neovascular Glaucoma: Chronic exudation and retinal detachment can result in neovascularization, which leads to secondary glaucoma. This type of glaucoma is difficult to control and can lead to further vision loss.
- Phthisis Bulbi: End-stage disease can cause phthisis bulbi, a condition in which the eye shrinks and becomes inoperable due to chronic inflammation and scarring.
- Cataract Formation: Chronic inflammation and retinal changes can raise the risk of cataract formation, further limiting vision.
Differential Diagnosis
Several ocular conditions can mimic the clinical features of Coat’s Disease, making a differential diagnosis critical for effective treatment. Conditions to consider are:
- Retinoblastoma: A malignant tumour of the retina that can cause leukocoria and retinal detachment. Because of the significant differences in treatment and prognosis, retinoblastoma and Coat’s Disease must be distinguished.
- Retinal Capillary Hemangioma: A benign vascular tumor of the retina that can result in similar exudative changes and retinal detachment.
- Familial Exudative Vitreoretinopathy (FEVR) is a genetic disorder characterized by abnormal retinal vascular development, which causes exudation and retinal detachment. FEVR can present similarly to Coat’s Disease, but it has a different genetic basis.
- Persistent Fetal Vasculature (PFV) is a congenital anomaly in which remnants of the fetal hyaloid vascular system remain, resulting in retinal detachment and leukocoria.
Pathology and Progression
Coat’s Disease pathogenesis is complex, involving vascular abnormalities and inflammatory responses. The primary event is the development of retinal telangiectasia, which increases vascular permeability and allows blood components to leak into the retina. The accumulation of lipoproteinaceous material and fluid in the retina and subretinal space causes an inflammatory response, which further damages retinal structures.
Coat’s Disease progression is variable and can be influenced by factors such as telangiectasia extent, exudation severity, and the patient’s overall health. Early intervention and appropriate management are critical in slowing the progression of the disease and avoiding complications.
Understanding the specific pathophysiology and clinical manifestations of Coat’s Disease is critical for developing effective diagnostic and treatment strategies. Continued research into the underlying mechanisms and potential treatment targets shows promise for improving patient outcomes in this difficult condition.
Coat’s Disease Prevention Strategies
le Coat’s Disease cannot be completely avoided due to its idiopathic nature, certain precautions can aid in early detection and management, lowering the risk of serious complications.
- Regular Eye Examination:
- Schedule regular eye exams for children and adolescents. Early detection of abnormal retinal findings can result in faster intervention and better outcomes.
- Awareness of symptoms:
- Inform parents and caregivers about the early symptoms of Coat’s Disease, including leukocoria (white reflex in the pupil), strabismus (crossed eyes), and visual disturbances. Prompt medical attention for these symptoms is critical.
- Protective eyewear:
- Encourage the use of protective eyewear during sports and recreational activities to avoid eye injuries that may worsen retinal conditions.
- A Healthy Lifestyle:
- Maintain a healthy lifestyle that includes a balanced diet high in antioxidants and omega-3 fatty acids to improve overall eye health. Encourage regular physical activity while avoiding smoking.
- Monitor high-risk individuals:
- Pay special attention to people who have a family history of retinal disease or other ocular conditions. Regular monitoring and early intervention can help manage potential problems before they worsen.
- Educate about eye health:
- Increase awareness of the importance of eye health and the need for regular eye examinations. Educational programs in schools and communities can aid in the early detection of vision problems.
- **Collaborate with Healthcare Providers:
- Collaborate with pediatricians, family doctors, and optometrists to provide comprehensive eye care for children and adolescents. A multidisciplinary approach can help with early diagnosis and management.
Diagnostic methods
Coat’s Disease is diagnosed using a combination of clinical examination, imaging studies, and, in some cases, genetic testing to accurately assess the condition and determine the best management plan.
Clinical Examination
The first step in diagnosing Coat’s Disease is to conduct a thorough clinical examination with an ophthalmologist. This includes:
- Visual Acuity Test: Determines the extent of vision loss in the affected eye.
- Fundoscopy is a detailed examination of the retina with an ophthalmoscope to detect telangiectasia, exudates, and signs of retinal detachment. Fundoscopy is required to visualize the characteristic retinal changes associated with Coat’s Disease.
Imaging Techniques
Advanced imaging techniques are essential for a thorough evaluation of the retina and informing treatment decisions.
- Fluorescein Angiography (FA) is an imaging technique that involves injecting a fluorescent dye into the bloodstream and photographing the retina. FA aids in determining the location of leaking blood vessels, the extent of exudation, and retinal detachment. It produces detailed images of the retinal vasculature, which are critical for diagnosing and tracking the progression of Coat’s disease.
- Optical Coherence Tomography (OCT): OCT is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the retina. It is particularly useful for determining retinal thickness, subretinal fluid levels, and the presence of macular edema. OCT is useful in quantifying retinal changes and guiding treatment.
- Ultrasound B-Scan: When retinal detachment is suspected but not easily visible with fundoscopy, an ultrasound B-scan can provide detailed images of the eye’s posterior segment. This technique is useful for determining the extent and nature of retinal detachment, as well as detecting any associated vitreous abnormalities.
Genetic Testing
Although Coat’s Disease is not usually associated with a genetic basis, genetic testing may be considered in cases with unusual symptoms or when there is a suspicion of underlying genetic syndromes that may mimic Coat’s Disease.
- Molecular Genetic Testing: This can help rule out other inherited retinal diseases that share clinical symptoms, such as familial exudative vitreoretinopathy (FEVR) or retinoblastoma. Genetic testing yields useful information for differential diagnosis and family counseling.
Differential Diagnosis
To accurately diagnose Coat’s Disease, it must be distinguished from other conditions that have similar clinical presentations. This includes:
- Retinoblastoma: It is critical to distinguish Coat’s Disease from retinoblastoma, a malignant retinal tumor, because treatment and prognosis differ significantly.
- Retinal Capillary Hemangioma: This benign vascular tumor has similar exudative changes but differs in clinical and imaging characteristics.
- Persistent Fetal Vasculature (PFV): PFV can result in similar retinal findings but is linked to congenital eye abnormalities.
By combining these diagnostic methods, healthcare providers can accurately diagnose Coat’s Disease, track its progression, and tailor treatment plans to each patient’s specific needs.
Effective Treatments for Coat’s Disease
Coat’s Disease treatment aims to manage retinal vascular abnormalities, reduce exudation, and avoid complications like retinal detachment. Treatment plans are tailored to the stage of the disease and the severity of the symptoms.
Laser Photocoagulation
Laser photocoagulation is a standard treatment for Coat’s Disease, especially in its early stages. The procedure uses laser energy to coagulate and seal the leaking retinal blood vessels. This helps to reduce exudation and prevent future leaks. Laser photocoagulation can be performed as an outpatient procedure and is effective in stabilizing the condition while preserving vision.
Cryotherapy
Cryotherapy involves applying extreme cold to abnormal retinal vessels in order to cause coagulation and reduce exudation. This treatment is especially effective for peripheral lesions that are difficult to access with laser therapy. Cryotherapy is effective in managing retinal telangiectasia and preventing it from progressing to more severe forms.
Anti-VEGF Therapies
Off-label treatments for Coat’s disease include intravitreal injections of anti-vascular endothelial growth factor (anti-VEGF) agents such as bevacizumab (Avastin) or ranibizumab (Lucentis). Anti-VEGF therapy reduces vascular permeability and exudation by preventing the formation of abnormal blood vessels. This treatment is especially effective for macular edema and exudative retinal detachment.
Vitrectomy
Vitrectomy is a surgical procedure used in the advanced stages of Coat’s Disease with exudative or tractional retinal detachment. The vitreous gel, as well as any scar tissue or exudates that may be contributing to retinal detachment, are removed during the procedure. Vitrectomy can help reattach the retina and improve visual outcomes in severe cases.
Corticosteroids
Corticosteroid injections, either intravitreal or periocular, can be used to reduce inflammation and exudation in Coat’s Disease. Steroids help to maintain the blood-retinal barrier and reduce fluid leakage. However, corticosteroids must be used with caution due to potential side effects such as increased intraocular pressure and cataract formation.
Emerging Therapies
Research into the treatment of Coat’s Disease is ongoing, and several emerging therapies show promise:
- Gene Therapy: Although still in the experimental stage, gene therapy seeks to correct underlying genetic abnormalities in retinal diseases. This approach has the potential to provide a long-term solution for managing Coat’s Disease.
- Novel Anti-Inflammatory Agents: New drugs that target specific inflammatory pathways are being studied for their ability to reduce exudation and retinal damage in Coat’s Disease.
Supportive Care
In addition to specific treatments, supportive care plays an important role in managing Coat’s Disease.
- Visual Aids: Patients with severe vision loss may benefit from low-vision devices and rehabilitation services to improve their quality of life.
- Regular Monitoring: Continuous monitoring, including regular eye examinations and imaging studies, is required to detect disease progression and adjust treatment as necessary.
By combining these treatment strategies, healthcare providers can effectively manage Coat’s Disease, preserve vision, and improve outcomes for patients.
Trusted Resources
Books
- Retinal Vascular Disease by J. Fernando Arevalo
- Retina by Stephen J. Ryan
- Retinal Imaging by Lawrence A. Yannuzzi










