Introduction
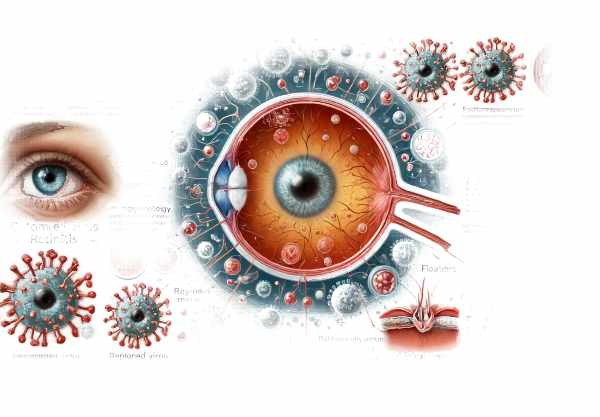
Cytomegalovirus (CMV) retinitis is a serious viral infection of the retina that primarily affects people with weakened immune systems, such as those with HIV/AIDS, organ transplant recipients, or patients receiving immunosuppressive therapy. The condition is caused by the cytomegalovirus, a common virus that can remain dormant in the body and reactivate when the immune system is weakened. CMV retinitis causes inflammation and damage to the retinal tissues, resulting in symptoms such as blurred vision, floaters, and, if left untreated, significant vision loss or blindness. Prompt recognition and treatment are critical to preventing irreversible retinal damage and preserving vision.
CMV Retinitis Insights
Cytomegalovirus (CMV) retinitis is a complicated condition that has serious consequences for those who suffer from it, especially those with weakened immunity. Understanding its pathophysiology, risk factors, epidemiology, clinical manifestations, and potential complications is critical for successful management.
Pathophysiology
CMV retinitis is caused by the reactivation of latent cytomegalovirus in people with weakened immune systems. The virus infects retinal cells and causes inflammation, necrosis, and tissue damage. The retina, as a highly vascular and sensitive tissue, is especially susceptible to the virus’s destructive effects. If left untreated, the infection usually starts on the retina’s periphery and can spread centrally to the macula and optic nerve.
Risk Factors
Several factors contribute to the risk of developing CMV retinitis, including
- HIV/AIDS: People with advanced HIV infection and low CD4+ T-cell counts (less than 50 cells/µL) have a higher risk of CMV retinitis. It is classified as an AIDS-defining illness.
- Immunosuppressive Therapy: Patients receiving immunosuppressive treatments, such as chemotherapy or corticosteroids, are at higher risk.
- Organ Transplantation: Organ transplant recipients, particularly those undergoing bone marrow transplants, are vulnerable due to the immunosuppressive medications required to prevent organ rejection.
- Congenital Infection: In rare cases, newborns can contract CMV retinitis from their mothers.
Epidemiology
CMV retinitis was more common prior to the introduction of highly active antiretroviral therapy (HAART) for HIV/AIDS. The prevalence of CMV retinitis has decreased dramatically as HAART has become more widely used. However, it remains a concern in areas with limited access to HIV treatment and among people who do not follow their antiretroviral therapy. CMV retinitis remains a major risk for transplant recipients and other immunocompromised patients.
Clinical Manifestations
The symptoms of CMV retinitis vary according to the severity and location of the retinal involvement. Common symptoms include:
- Blurred Vision: Patients frequently describe the gradual or sudden onset of blurred vision, which can affect one or both eyes.
- Floaters: One common complaint is the presence of floaters, which are small dark spots that move across the visual field.
- Photophobia: Inflammation of the retina can cause light sensitivity.
- Scotomas: Patients may develop blind spots or areas of reduced vision in their visual field.
- Vision Loss: In severe cases, CMV retinitis can result in significant vision loss or blindness, especially if the infection affects the macula or optic nerve.
Potential Complications
If not treated promptly, CMV retinitis can cause a number of serious complications:
- Retinal Detachment: CMV-induced inflammation and necrosis can weaken retinal tissue, resulting in tears and detachments.
- Macular Involvement: Damage to the macula, the central part of the retina responsible for sharp vision, can lead to severe central vision loss.
- Optic Neuritis: The infection can spread to the optic nerve, resulting in inflammation and potentially permanent nerve damage.
- Immune Recovery Uveitis: When HIV patients begin HAART, they may experience a paradoxical worsening of retinal inflammation known as immune recovery uveitis. This occurs when the immune system begins to recover and attack CMV-infected cells.
Effects on Quality of Life
CMV retinitis has a significant impact on the quality of life of those affected. Vision loss can impair daily activities, reduce independence, and increase the likelihood of accidents and injuries. The psychological toll of a chronic, sight-threatening condition can result in anxiety, depression, and a lower overall quality of life.
Challenges of Management
Managing CMV retinitis presents several challenges.
- Early Detection: Early detection is critical for avoiding irreversible damage, but symptoms can be subtle or develop slowly, delaying diagnosis.
- Access to Care: Limited access to healthcare, especially in resource-constrained settings, can impede timely diagnosis and treatment.
- Adherence to Therapy: In HIV patients, adherence to antiretroviral therapy is critical for preventing CMV reactivation. Noncompliance can result in reactivation and progression of retinitis.
- Treatment-Related Complications: Long-term use of antivirals can result in drug resistance and other side effects, complicating treatment.
Prevention Tips
- Adherence to antiretroviral therapy: For HIV patients, taking antiretroviral medications exactly as prescribed is critical to maintaining a strong immune system and preventing CMV reactivation.
- Immunocompromised individuals require regular comprehensive eye exams to detect early signs of CMV retinitis and other ocular complications.
- Immune System Monitoring: Regularly monitoring immune status, especially CD4+ T-cell counts in HIV patients, helps assess the risk of CMV retinitis and the need for preventive measures.
- Prophylactic Antiviral Therapy: – High-risk patients, such as those with low CD4+ counts or transplant recipients, may require prophylactic antiviral therapy to prevent CMV infection and retinitis.
- Healthy Lifestyle Choices: – A balanced diet, regular exercise, and avoiding smoking and excessive alcohol consumption promote immune health.
- Early and effective treatment of opportunistic infections can prevent immune system weakening and lower the risk of CMV reactivation.
- Education and Awareness: – Educating at-risk populations on CMV retinitis symptoms, regular eye exams, and therapy adherence can help detect and treat it early.
- Access to Healthcare: Providing comprehensive healthcare services, including ophthalmologic care, is crucial for early detection and management of CMV retinitis in immunocompromised individuals.
Diagnostic methods
Cytomegalovirus (CMV) retinitis is diagnosed using a combination of clinical examination, imaging techniques, and laboratory tests to confirm the virus’s presence and determine the extent of retinal damage.
Clinical Examination
- Visual Acuity Test: This test uses an eye chart to determine vision clarity. It aids in determining the severity of CMV retinitis-related vision loss.
- Fundus Examination: – A thorough examination of the retina with an ophthalmoscope enables the ophthalmologist to detect characteristic signs of CMV retinitis, such as retinal hemorrhages, exudates, and necrosis. This direct visualization is critical to diagnosis.
Imaging Techniques
- Optical Coherence Tomography (OCT):
- OCT generates high-resolution cross-sectional images of the retina, allowing for the detection of retinal thickening, structural changes, and the extent of retinal involvement. It is particularly useful for tracking the disease’s progression and response to treatment.
- fluorescein angiography (FA):
- In FA, a fluorescent dye is injected into the bloodstream and photographs of the retina are taken as it circulates. This technique aids in the identification of retinal leakage, ischemia, and abnormal blood vessels, all of which are signs of CMV retinitis.
- Indocyanine Green Angiogram (ICGA):
- Indocyanine green dye is used in ICGA to produce detailed images of choroidal circulation. It is useful for detecting choroidal neovascularization and other vascular abnormalities associated with CMV retinitis.
Lab Tests
- Polymerase Chain Reaction (PCR): – PCR testing of blood, aqueous humor, or vitreous samples can detect CMV DNA and confirm the diagnosis. This test is extremely sensitive and specific, making it an excellent diagnostic tool.
- Serological Tests: – Blood tests can detect CMV-specific antibodies (IgM and IgG), indicating current or previous infection. However, serological tests are less specific than PCR in detecting active retinitis.
Advanced Diagnostic Techniques
- Ultra-Widefield Imaging: This imaging technique produces detailed, wide-angle images of the retina, allowing for a thorough examination of peripheral retinal involvement, which is common in CMV retinitis. It aids in detecting early symptoms of the disease and tracking its progression.
- Adaptive Optics (AO): – AO captures ultra-high-resolution images of retinal microstructure. It can detect individual cells and fine details, allowing researchers to assess the impact of CMV retinitis on retinal architecture.
- Electroretinography (ERG) measures the retina’s electrical responses to light stimuli. It can detect functional changes in retinal cells infected with CMV retinitis, providing information about the extent of retinal damage.
Clinical Guidelines
- Immunocompromised individuals require regular retinal examinations and immune status monitoring, such as CD4+ T-cell counts in HIV patients, to detect and manage CMV retinitis early on.
Treatment
- Antiviral Medication: – Ganciclovir Ganciclovir, administered intravenously or as an intravitreal implant, is the first-line treatment for CMV retinitis. It inhibits viral DNA replication, thereby controlling the infection and minimizing retinal damage.
- valganciclovir: Valganciclovir, an oral prodrug of ganciclovir, provides a convenient long-term management option, particularly for maintenance therapy following initial treatment with intravenous ganciclovir.
- Foscarnet is an intravenous antiviral agent used to treat CMV retinitis. It is especially useful when ganciclovir is either ineffective or poorly tolerated.
- Cidofovir: – Cidofovir, administered intravenously, is an option for patients who do not respond to or are unable to tolerate other antivirals. It has a longer dosing interval, which may be beneficial for certain patients.
Innovative and Emerging Therapies
- Intravitreal Injections: – Antiviral injections, such as ganciclovir or foscarnet, deliver high concentrations directly to the retina, resulting in rapid infection control. This method is particularly effective for sight-threatening lesions.
- Combination Therapy: – Combining antiviral agents or immunomodulatory therapies can improve treatment efficacy and reduce drug resistance. This strategy is being tested to improve outcomes in refractory cases.
- Gene Therapy: – Gene therapy involves introducing or modifying genes within retinal cells to increase resistance to CMV infection. Although still in the experimental stage, this approach has the potential to improve long-term control and prevention of CMV retinitis.
- Immune Modulation: Immune modulators or cytokine therapy may improve CMV infection control and reduce the need for long-term antiviral drugs.
Supportive Treatments
- Corticosteroids: – Corticosteroids can control inflammation and prevent further retinal damage in cases of immune recovery uveitis.
- Laser Therapy: – Laser photocoagulation can treat complications such as retinal detachment and neovascularization caused by CMV retinitis.
Long-Term Management.
- Regular follow-up through eye exams and imaging studies is crucial for detecting recurrences early and adjusting treatment protocols accordingly.
- Adherence to Antiretroviral Therapy: – HIV patients must strictly adhere to antiretroviral therapy to maintain immune function and prevent CMV reactivation.
- Multidisciplinary Care: Collaboration among ophthalmologists, infectious disease specialists, and primary care providers ensures comprehensive management of CMV retinitis and associated conditions.
Trusted Resources
Books
- “Retina” by Stephen J. Ryan
- “The Retina Atlas” by Lawrence A. Yannuzzi
- “Ocular Infection” by T. V. Paul










