Introduction
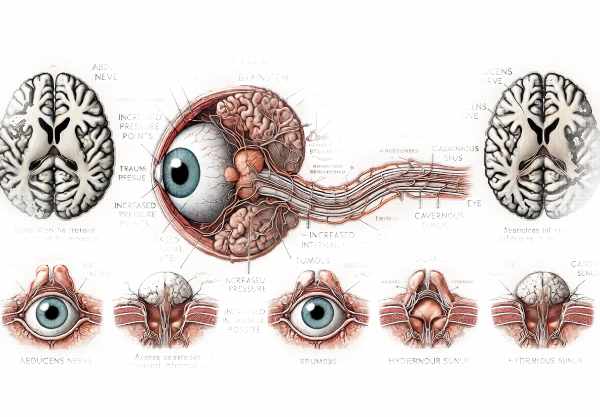
Cranial Nerve VI Palsy, also known as abducens nerve palsy, is a neurological condition caused by dysfunction of the sixth cranial nerve. This nerve controls the lateral rectus muscle, which moves the eye outwards. When the sixth cranial nerve is compromised, patients experience horizontal diplopia (double vision) and are unable to move the affected eye outward. This condition can be caused by a variety of factors, including trauma, vascular disorders, infections, and tumors. Cranial Nerve VI Palsy can have a significant impact on a person’s vision and quality of life, so it’s important to understand the pathophysiology, associated symptoms, and potential risk factors.
Cranial Nerve VI Palsy: Insights
Cranial Nerve VI Palsy is a rare disorder that has serious consequences for patients who develop it. The sixth cranial nerve, also known as the abducens nerve, originates in the brainstem’s pons, specifically the abducens nucleus. This nerve has a long intracranial course before innervating the lateral rectus muscle, making it prone to injury and pathology.
Pathophysiology
The abducens nerve’s long journey from the brainstem to the eye makes it susceptible to damage at various points along the way. This nerve can be affected by any condition that raises intracranial pressure, such as trauma, tumors, or hydrocephalus. Increased intracranial pressure can stretch the nerve, causing dysfunction. Furthermore, the abducens nerve travels through the cavernous sinus, a large vein at the base of the skull. Conditions of the cavernous sinus, such as thrombosis or infection, can have a direct impact on the nerve.
Etiology
The causes of Cranial Nerve VI Palsy can be divided into several categories:
- Vascular Causes: – Ischemic Stroke: Small vessel ischemic disease, commonly linked to diabetes and hypertension, can harm the nerve.
- Aneurysms, particularly those in the internal carotid artery, can compress the nerve.
- Trauma: – Head Injury: Blunt trauma to the head may stretch or compress the nerve.
- Surgical Complications: Cranial surgeries, particularly those involving the brainstem or base of the skull, can injure the nerve.
- Infectious Causes: – Meningitis: Inflammation of the meninges can harm cranial nerves, including the abducens nerve.
- Lyme Disease: This tick-borne illness may cause cranial nerve inflammation.
- Neoplastic Causes: – Brain Tumors: Tumors, particularly in the posterior fossa, can compress or infiltrate the nerve.
- Metastases: Cancer that has spread to the brain can damage the nerve.
- Idiopathic Causes: – Cranial Nerve VI Palsy’s exact cause is often unknown.
Clinical Presentation
Patients with Cranial Nerve VI Palsy commonly have:
- Horizontal Diplopia: Double vision is a defining symptom, which worsens when looking to the affected side.
- Esotropia: The affected eye may turn inward because the lateral rectus muscle is not working properly.
- Limited Abduction: The eye’s outward movement is noticeably restricted.
- Head Turn: To compensate for double vision, patients can turn their head to the affected side.
Epidemiology
Cranial Nerve VI Palsy can happen at any age, but it is more common in adults, especially those with risk factors like diabetes and hypertension. Pediatric cases are uncommon but can be associated with congenital malformations or infections.
Complications
If left untreated, Cranial Nerve VI Palsy can result in persistent diplopia and the development of compensatory head postures, which can cause neck pain and muscular strain. In severe cases, underlying conditions like tumors or aneurysms can be fatal if not treated promptly.
Prognosis
The prognosis for Cranial Nerve VI Palsy is largely determined by the underlying cause. Cases of microvascular ischemia, such as those seen in diabetic patients, typically resolve spontaneously within three to six months. However, palsy caused by tumors, trauma, or infections may have a more uncertain prognosis and necessitate surgical intervention or long-term management.
Differential Diagnosis
It is critical to distinguish Cranial Nerve VI Palsy from other conditions that may produce similar symptoms, such as myasthenia gravis, thyroid eye disease, and other cranial neuropathies. Misdiagnosis can lead to ineffective treatments and a worsening of the patient’s condition.
Prevention Tips
- Manage Chronic Conditions: – Monitor and control chronic diseases such as diabetes and hypertension to prevent vascular causes of Cranial Nerve VI Palsy.
- Protect Against Trauma: – Use appropriate safety equipment, such as helmets, for activities that may cause head injury.
- Implement safety precautions to prevent falls, particularly in the elderly.
- Infection Control: – Maintain vaccinations to avoid infections that could harm the cranial nerves, such as meningitis.
- Maintain proper hygiene to reduce the risk of Lyme disease and other infectious diseases.
- Schedule regular medical check-ups with healthcare providers to identify early signs of systemic diseases that may cause Cranial Nerve VI Palsy.
- Early detection of conditions such as tumors or aneurysms allows for faster treatment and prevents nerve damage.
- Healthy Lifestyle: – Maintain a balanced diet, engage in regular exercise, and avoid smoking to improve vascular health and lower the risk of ischemic causes.
- Awareness and Education: – Educate yourself and others about the symptoms and risks of Cranial Nerve VI Palsy to ensure early detection and medical intervention.
Diagnostic methods
Cranial Nerve VI Palsy is diagnosed using a comprehensive approach that combines clinical evaluation and advanced imaging techniques. The primary goal is to determine the underlying cause of nerve dysfunction.
Clinical Evaluation
- Patient History: A complete medical history is required, including any recent head trauma, infections, or chronic conditions like diabetes or hypertension. Detailed questions about the onset and progression of symptoms, particularly double vision and eye movement limitations, are essential.
- Physical Examination: – Ocular Examination: Assessing eye movements for abduction deficits and esotropia. The Hirschberg test and the cover-uncover test are frequently used.
- Neurological Examination: A thorough neurological examination can rule out other cranial nerve involvements or systemic neurological conditions.
Imaging Studies
- MRI: – Brain MRI It is the preferred imaging modality for assessing the brainstem, where the abducens nucleus is located, and the path of the abducens nerve. It is particularly effective at detecting tumors, multiple sclerosis plaques, and brainstem infarctions.
• Magnetic Resonance Angiography (MRA): This can be used in conjunction with an MRI to evaluate vascular structures and identify aneurysms or vascular malformations that may compress the nerve. - Computed Tomography (CT) Scan: – CT Head: Detects bone fractures, hemorrhages, and calcified lesions that may affect the abducens nerve.
- CT Angiography: This procedure, like MRA, aids in the visualization of vascular abnormalities.
- Lumbar Puncture: If an infectious or inflammatory cause is suspected, cerebrospinal fluid (CSF) analysis through a lumbar puncture can provide crucial information.
Electrophysiological Studies
- EMG: – While not commonly used for Cranial Nerve VI Palsy, EMG can aid in assessing muscle function and nerve conduction in more complex cases.
Lab Tests
- Blood Tests: – Comprehensive blood tests can identify systemic conditions like diabetes, infections, and autoimmune disorders that may cause palsy.
- Based on the patient’s medical history and clinical symptoms, specific Lyme disease or syphilis tests may be recommended.
Advanced Diagnostic Techniques
- High-Resolution MRI: – Advanced MRI technology, including high-resolution and functional MRI, enhances diagnostic accuracy by providing detailed images of cranial nerves and surrounding structures.
- Diffusion Tensor Imaging (DTI) is a type of MRI that can map nerve pathways and detect subtle abnormalities in the abducens nerve.
Treatment
- Observation: – Cranial Nerve VI Palsy caused by microvascular ischemia, especially in diabetic or hypertensive patients, typically resolves spontaneously within a few months. Regular follow-ups are required to monitor recovery.
- Prism Glasses: – Temporary prism glasses can correct double vision by redirecting light and improving alignment.
- Eye Patching: – Acute diplopia can be managed with alternating eye patching, which covers one eye to prevent double vision.
- Botulinum Toxin (Botox) Injections: – Injecting Botox into the affected eye’s medial rectus muscle temporarily relieves esotropia by weakening the overacting muscle.
Innovative and Emerging Therapies
- Surgical Interventions: – Strabismus Surgery: Adjusting the muscles controlling eye movement can realign the eyes in persistent cases. Procedures such as lateral rectus resection or medial rectus recession are frequently performed.
- Transposition Procedures: When direct lateral rectus surgery is not possible, vertical recti transposition surgeries can be used to restore abduction.
- Advanced Botulinum Toxin Applications: Ongoing research aims to improve outcomes and reduce side effects of Botox injections through more precise and controlled injection techniques.
- Neuroprotective Agents: These emerging therapies aim to improve nerve recovery and function. These include medications that stimulate nerve growth and regeneration.
- Rehabilitative Therapies: – Vision Therapy: Programs to improve eye coordination and reduce diplopia are being developed.
- Neuromuscular Stimulation: Methods for electrically stimulating the lateral rectus muscle, promoting strength and functionality, are being investigated.
- Gene Therapy: – While still in experimental stages, gene therapy has the potential to treat Cranial Nerve VI Palsy by targeting genetic causes and promoting nerve regeneration.
Trusted Resources
Books
- “Neuro-Ophthalmology: Diagnosis and Management” by Grant T. Liu, Nicholas J. Volpe, Steven L. Galetta
- “Clinical Neuro-Ophthalmology: A Practical Guide” by Ambar Chakraborty, Andrew G. Lee
- “Ophthalmology” by Myron Yanoff, Jay S. Duker










