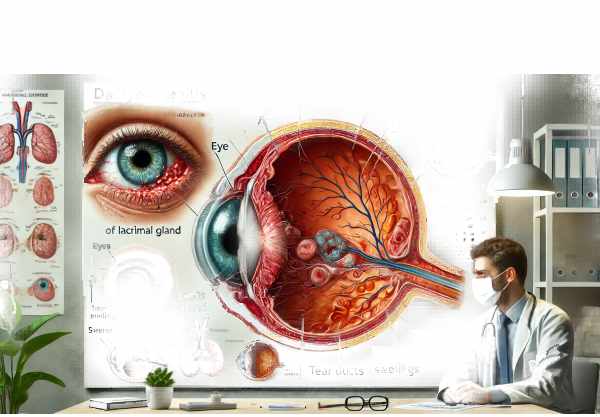
Introduction to Dacryoadenitis
Dacryoadenitis is an inflammation of the lacrimal gland, which produces tears. This condition, which can be acute or chronic, is distinguished by swelling, pain, redness, and, in some cases, fever in the upper eyelid region containing the gland. Acute dacryoadenitis is frequently caused by viral or bacterial infections, whereas chronic dacryoadenitis is more commonly linked to systemic inflammatory conditions like sarcoidosis, tuberculosis, and autoimmune diseases. Prompt diagnosis and treatment are critical for preventing complications and maintaining ocular health. Understanding the underlying causes and clinical manifestations of dacryoadenitis is critical for successful treatment.
Dacryoadenitis insights
Dacryoadenitis, or inflammation of the lacrimal gland, can have a significant impact on ocular health and patient well-being. Its causes are varied, ranging from infections to systemic inflammatory disorders. Here, we will look at the pathophysiology, risk factors, epidemiology, clinical manifestations, and potential complications of dacryoadenitis.
Pathophysiology
The lacrimal gland, located in the upper outer region of the orbit, is responsible for keeping the ocular surface healthy by producing tears. When this gland becomes inflamed, it inhibits tear secretion, resulting in a variety of ocular symptoms. The pathophysiology of dacryoadenitis can be classified as acute or chronic.
- Acute Dacryoadenitis can lead to infections. Acute dacryoadenitis is commonly caused by viral infections like mumps, Epstein-Barr virus, and influenza, as well as bacterial infections like Staphylococcus aureus and Streptococcus species. The infection causes acute inflammation, which is characterized by the sudden onset of symptoms such as pain, swelling, and redness.
- Chronic Dacryoadenitis is associated with inflammatory diseases. Chronic dacryoadenitis is often linked to systemic inflammatory diseases like sarcoidosis, Sjögren’s syndrome, and tuberculosis. These conditions cause chronic inflammation of the lacrimal gland, resulting in long-term symptoms and possible glandular dysfunction.
Risk Factors
Several factors raise the risk of developing dacryoadenitis.
- Infectious Agents: Exposure to viral or bacterial pathogens can result in acute dacryoadenitis.
- Systemic Inflammatory Diseases: Individuals with sarcoidosis, tuberculosis, or autoimmune diseases are more likely to develop chronic dacryoadenitis.
- Immunocompromised States: Patients with weakened immune systems, such as those with HIV/AIDS or on immunosuppressive therapy, are more vulnerable to infections that cause dacryoadenitis.
- Trauma: Injuries to the lacrimal gland or surrounding tissues may cause secondary inflammation.
Epidemiology
Dacryoadenitis is rare in comparison to other ocular conditions. Acute dacryoadenitis is more common in children and young adults, owing to higher rates of viral infections. Chronic dacryoadenitis is more common in adults and frequently associated with systemic diseases. The incidence and prevalence of dacryoadenitis vary geographically, depending on the prevalence of underlying conditions such as tuberculosis in each region.
Clinical Manifestations
The symptoms of dacryoadenitis differ depending on whether it is acute or chronic.
- Acute Dacryoadenitis causes sudden pain in the upper outer region of the eyelid, near the lacrimal gland.
- Swelling and Redness: The affected area swells, turns red, and is tender to the touch.
- Fever: Systemic symptoms such as fever and malaise may occur alongside local ocular symptoms.
- Proptosis: In severe cases, inflammation may cause the eye to protrude slightly.
- Purulent Discharge: If the cause is bacterial, the eye may discharge pus.
- Chronic Dacryoadenitis: – Persistent Swelling: Chronic dacryoadenitis causes less severe and longer-lasting swelling than acute dacryoadenitis.
- Dry Eyes: Chronic inflammation can interfere with tear production, causing symptoms such as irritation, burning, and a foreign body sensation.
- Mild Discomfort: The pain is usually less severe than in acute dacryoadenitis.
- Systemic Symptoms: Patients with chronic dacryoadenitis frequently experience systemic symptoms associated with the underlying disease, such as joint pain, respiratory problems, or general fatigue.
Potential Complications
If left untreated, dacryoadenitis can cause a number of complications:
- Abscess Formation: Severe bacterial infections can cause an abscess in the lacrimal gland, requiring surgical drainage.
- Chronic Inflammation: Acute infections that are not treated properly can lead to chronic dacryoadenitis.
- Tear Film Dysfunction: Prolonged inflammation of the lacrimal gland can result in chronic dry eye syndrome due to insufficient tear production.
- Orbital Cellulitis: The infection can spread to the surrounding orbital tissues, resulting in a more serious condition called orbital cellulitis, which necessitates immediate medical attention.
- Vision Impairment: Severe or prolonged inflammation can harm the lacrimal gland and its surrounding structures, potentially resulting in visual impairment.
Effects on Quality of Life
Dacryoadenitis has a significant impact on a patient’s quality of life. Acute forms cause significant discomfort and can disrupt daily activities. Chronic dacryoadenitis, particularly when combined with systemic diseases, can cause persistent symptoms that impair both ocular and general health. Managing the underlying systemic condition is often critical for relieving ocular symptoms and improving overall health.
Dacryoadenitis Prevention Methods
- Maintain Good Hygiene: – Washing hands regularly and avoiding eye contact can lower the risk of infections that can cause dacryoadenitis.
- Manage Underlying Health Conditions: – Treating systemic inflammatory diseases like sarcoidosis and Sjögren’s syndrome can help prevent chronic dacryoadenitis. Adherence to treatment plans and regular check-ins with healthcare providers are critical.
- Protect the Eyes: – Wearing protective eyewear in areas with high exposure to dust, debris, or potential trauma can prevent injury and inflammation of the lacrimal gland.
- Limit contact with infected individuals to reduce the risk of acute dacryoadenitis. Examples of viral infections include mumps and influenza.
- Immunizations: – Regular vaccinations, especially for mumps and influenza, can prevent viral infections that cause dacryoadenitis.
- Early and appropriate treatment of eye infections, such as conjunctivitis, can prevent infection spreading to the lacrimal gland.
- Regular Eye Examinations: – Early detection of inflammation or ocular issues can lead to timely intervention.
- Healthy Lifestyle Choices: – Eating a healthy diet, exercising regularly, and avoiding smoking can boost immunity and lower the risk of infections and inflammation.
Diagnostic methods
Dacryoadenitis is diagnosed using a combination of clinical evaluation, laboratory tests, and imaging techniques to determine the underlying cause and extent of inflammation.
Clinical Evaluation
- Patient History: Identify any recent infections, systemic diseases, or trauma that could cause dacryoadenitis. The clinician will inquire about the onset, duration, and severity of the symptoms.
- Physical Examination: A thorough examination of the eye and surrounding structures is performed. This includes inspecting the upper eyelid for swelling, redness, and tenderness, as well as looking for discharge or proptosis.
- Ophthalmic Examination: A slit-lamp examination assesses the anterior segment of the eye and detects conjunctivitis or keratitis. The lacrimal gland is palpated to determine the consistency and presence of any masses or abscesses.
Lab Tests
- Blood Tests: – A complete blood count (CBC) may show increased white blood cell counts, indicating an infection. Other blood tests may reveal markers for systemic inflammatory diseases, such as erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP).
- Microbiological Tests: – If bacterial infection is suspected, a sample of eye discharge can be collected for culture and sensitivity testing to identify the causative organism and guide antibiotic therapy.
- Serological Tests: – Tests for viruses such as mumps and Epstein.Acute dacryoadenitis can be caused by viruses, and the Barr virus can help diagnose this.
Imaging Techniques
- Ultrasound: – Orbital ultrasound is a non-invasive imaging technique used to assess the lacrimal gland’s size, shape, and internal structure. It aids in detecting abscesses, masses, and the severity of inflammation.
- CT Scan: – A CT scan of the orbits can yield detailed images of the lacrimal gland and its surrounding tissues. It is especially useful for detecting abscesses, tumors, and the severity of the inflammatory response.
- Magnetic Resonance Imaging(MRI):
- MRI is used to obtain high-resolution images of the soft tissues within and around the orbit. It is especially useful for distinguishing between different types of lesions and determining the role of the lacrimal gland in systemic diseases.
Advanced Diagnostic Techniques
- Biopsy: – In cases of chronic dacryoadenitis or when a malignancy is suspected, a lacrimal gland biopsy may be performed. A histopathological examination can provide definitive information about the nature of the inflammation and rule out neoplastic conditions.
- Tear Film Analysis: Analysis of tear film composition can detect changes linked to chronic dacryoadenitis, such as decreased tear production and elevated inflammatory markers.
- Fluorescein Dye Testing: – Fluorescein dye can assess tear film and drainage system integrity, which may be affected by lacrimal gland inflammation.
Dacryoadenitis Treatment Options
- Antibiotics: For bacterial dacryoadenitis, oral or intravenous antibiotics are prescribed based on infection severity and culture results. Amoxicillin-clavulanate, cephalosporins, and fluoroquinolones are among the most commonly prescribed antibiotics.
- Antiviral Medications: For viral dacryoadenitis caused by mumps or Epstein-Barr virus, antiviral medications may be prescribed alongside supportive care.
- Anti-inflammatory Medications: – NSAIDs or corticosteroids are used to alleviate inflammation and pain. Corticosteroids are especially effective in treating chronic dacryoadenitis associated with systemic inflammatory diseases.
- Warm Compresses: – Applying warm compresses to the affected eye can reduce pain and swelling by improving blood flow and facilitating drainage of discharge.
Surgical Interventions
- Incision and Drainage: – If an abscess develops in the lacrimal gland, surgical drainage may be required to remove pus and relieve pressure. This procedure is typically done with local anesthesia.
- Lacrimal Gland Biopsy: In cases of chronic inflammation or a mass, a biopsy may be performed to obtain tissue samples for histopathological examination. This aids in the diagnosis of underlying conditions like sarcoidosis, tuberculosis, or cancer.
Innovative and Emerging Therapies
- Biologic Agents: – Biologic agents targeting specific inflammatory pathways, such as tumor necrosis factor (TNF) inhibitors, are being investigated for treating chronic dacryoadenitis linked to autoimmune diseases.
- Immunomodulatory Therapy: In refractory cases, medications like methotrexate or azathioprine can control chronic inflammation by modulating the immune response.
- Gene Therapy: While still in the experimental stage, gene therapy has the potential to treat chronic inflammatory conditions affecting the lacrimal gland by targeting specific genetic factors involved in the inflammatory process.
Supportive Treatments
- Artificial Tears: For patients with chronic dacryoadenitis and dry eye symptoms, artificial tears and lubricating eye drops can help maintain surface moisture and comfort.
- Patient Education: Encouraging patients to adhere to treatment regimens and attend follow-up appointments is crucial for managing chronic dacryoadenitis and avoiding complications.
Long-Term Management.
- Regular monitoring with an ophthalmologist is necessary to track disease progression and adjust treatment plans as needed.
- Managing Underlying Conditions: Controlling chronic dacryoadenitis requires effective management of systemic diseases like sarcoidosis and Sjögren’s syndrome.
Trusted Resources
Books
- “The Lacrimal System: Diagnosis, Management, and Surgery” by Jeffrey J. Hurwitz
- “Ophthalmic Inflammation and Infection” by James J. Reidy
- “Duke-Elder’s Practice of Refraction” by David Abrams










