What is Peter’s Anomaly?
Peters anomaly is a rare congenital eye disorder that causes abnormalities in the development of the eye’s anterior segment. It is named for Dr. Albert Peters, who first described the condition in 1906. This condition primarily affects the cornea, the clear, dome-shaped surface that covers the front of the eye, and can cause severe visual impairment. The anomaly is usually present from birth and can affect one or both eyes.
Pathophysiology
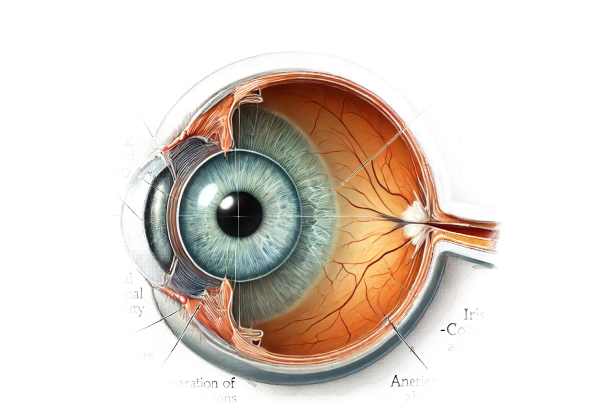
Peters anomaly is a developmental defect in the anterior segment of the eye that primarily affects the cornea and the structures surrounding it. The main features of Peters anomaly are central corneal opacity (leukoma), iris-corneal adhesions, and anterior chamber abnormalities. These characteristics arise from the incomplete separation of the cornea and iris during embryonic development.
Corneal Opacity: One of the distinguishing features of Peters anomaly is the presence of central corneal opacity. This opacity is typically located in the center of the cornea and can vary in size and density. The opacity results from a failure in the normal development and differentiation of the corneal endothelium and Descemet’s membranes.
Iridocorneal Adhesions: Another distinguishing feature is the existence of adhesions between the iris and the cornea. These adhesions obstruct the normal flow of aqueous humor, posing risks such as increased intraocular pressure and glaucoma.
Anterior Chamber Abnormalities: The anterior chamber, the fluid-filled space between the cornea and the iris, can be shallow or irregularly shaped. This abnormality can exacerbate the fluid dynamics within the eye, contributing to the development of glaucoma.
Causes and Risk Factors
Although the exact cause of Peters anomaly is unknown, it is thought to be caused by disruptions in the normal development of the anterior segment of the eye during embryogenesis. Both genetic and environmental factors may contribute to the development of the condition.
Genetic Factors: There have been several genetic mutations and syndromes linked to Peters anomaly. Mutations in genes PAX6, PITX2, FOXC1, and CYP1B1 have been linked to the condition. These genes contribute to the development and differentiation of the eye’s anterior segment structures. Furthermore, Peters anomaly can be associated with a variety of genetic syndromes, including Axenfeld-Rieger syndrome, which is defined by anterior segment abnormalities as well as other systemic anomalies.
Environmental Factors: Although genetics play an important role, environmental factors during pregnancy may also contribute to the development of Peters anomaly. These factors may include maternal infections, teratogen exposure (substances that can cause congenital abnormalities), and nutritional deficiencies.
Symptoms
The symptoms and clinical presentation of Peter’s anomaly vary greatly depending on the severity of the condition. Common indications and symptoms include:
Leukocoria: One of the most noticeable symptoms of Peters anomaly is leukocoria, also known as a white pupillary reflex. This is due to a central corneal opacity, which appears as a white spot in the pupil when light enters the eye.
Vision Impairment: The size and density of the corneal opacity, as well as the presence of other ocular abnormalities, determine the extent of vision impairment. In severe cases, significant vision loss or blindness may occur.
Strabismus: Eye misalignment, or strabismus, is common in children with Peters anomaly. Poor visual input can lead to a lack of proper binocular vision development.
Nystagmus: Involuntary, rhythmic eye movements, or nystagmus, may be present, especially if the condition has severely impaired vision from a young age.
Another common symptom is sensitivity to light, also known as photophobia. This can occur as a result of corneal irregularities and the scattering of light entering the eye.
Impact on Vision
The impact of Peters anomaly on vision is significant and depends on a number of factors, including the severity of the corneal opacity, the presence of other anterior segment abnormalities, and the efficacy of any treatments used. Mild cases of visual impairment may be treatable with corrective lenses and supportive treatments. However, in severe cases, the condition can cause profound vision loss or blindness.
Unilateral vs. Bilateral: Peter’s anomaly can affect either one or both eyes. Bilateral involvement typically causes more severe visual impairment and poses greater management and treatment challenges.
Amblyopia: Also known as “lazy eye,” amblyopia can occur in the affected eye as a result of inadequate visual input during the critical period of visual development. If not treated early, amblyopia can result in permanent vision loss.
Glaucoma: Iridocorneal adhesions and abnormalities in the anterior chamber can cause increased intraocular pressure and glaucoma. This is a serious complication that can damage the optic nerve and worsen vision loss.
Psychological and Social Implications
Living with the Peters anomaly can have significant psychological and social consequences, particularly for children. Visible abnormalities such as leukocoria and strabismus can have an impact on self-esteem and social relationships. Vision impairment can have an impact on learning and development, making it difficult for children to keep up academically and socially. Early intervention and support are critical for assisting children and their families in dealing with the challenges posed by Peters anomaly.
Complications
If left untreated, Peters anomaly can cause a number of serious complications, including:
Corneal Ulceration: The presence of corneal opacity and structural abnormalities can predispose the cornea to ulceration and infection, further impairing vision.
Glaucoma: Iridocorneal adhesions can cause increased intraocular pressure, which can lead to secondary glaucoma and vision loss if left untreated.
Retinal Detachment: Although uncommon, retinal detachment can occur in severe cases of Peters anomaly due to structural abnormalities and increased intraocular pressures.
Cataracts: Anterior segment anomalies can cause cataract formation, which contributes to vision impairment.
Amblyopia: As previously stated, amblyopia can develop in the affected eye due to inadequate visual input, resulting in permanent vision impairment if not treated promptly.
Prognosis
The prognosis for Peters anomaly is variable, depending on the severity of the condition and the efficacy of treatment. Early diagnosis and management are critical for improving visual outcomes and avoiding complications. Many people with Peters anomaly can have functional vision and live fulfilling lives if they receive timely and effective treatment.
Methods for Diagnosing Peters Anomaly
A comprehensive evaluation by an ophthalmologist is required to diagnose Peters anomaly, which includes clinical examination, imaging techniques, and genetic testing to confirm the condition’s presence and severity. Here are the main diagnostic methods used:
Clinical Examination
Ophthalmic Examination: Diagnosing Peters anomaly begins with a thorough ophthalmic examination. This includes evaluating visual acuity, examining the anterior segment with a slit lamp, and performing a dilated fundus examination to see the posterior segment structures.
Slit Lamp Biomicroscopy: Slit lamp biomicroscopy is required to diagnose corneal opacity, iridocorneal adhesions, and other anterior segment abnormalities. This examination reveals the precise location, size, and extent of the corneal opacity.
Tonometry: Measuring intraocular pressure is critical for detecting glaucoma, a common complication of Peter’s anomaly. Elevated intraocular pressure may indicate the need for additional evaluation and treatment.
Imaging Techniques
Ultrasound Biomicroscopy (UBM): UBM is an excellent imaging tool for examining anterior segment structures. It aids in detecting abnormalities such as persistent tunica vasculosa lentis, elongated ciliary processes, and shallow anterior chambers.
B-Scan Ultrasound: B-scan ultrasonography generates cross-sectional images of the eye, allowing for the detection of vitreous and retinal abnormalities. It is especially useful in cases where the medium is opaque, such as dense corneal opacities.
Optical Coherence Tomography (OCT): OCT can produce high-resolution cross-sectional images of the retina and optic nerve. It is effective at detecting retinal and optic nerve abnormalities that may be associated with Peters anomaly.
Anterior Segment OCT: This type of OCT focuses on the anterior segment structures, capturing detailed images of the cornea, anterior chamber, and iris. It is useful for determining the severity of iridocorneal adhesions and other anterior segment abnormalities.
Genetic Testing
Molecular Genetic Testing: Genetic testing can be performed if Peters anomaly is suspected to be part of a genetic syndrome or if the patient has a family history of similar conditions. This aids in identifying specific genetic mutations associated with Peters anomaly and can provide useful information for genetic counseling.
Differential Diagnosis
Congenital Cataracts: One of the most difficult conditions to distinguish from Peters anomaly is congenital cataracts, which can also be associated with leukocoria. Imaging and clinical characteristics aid in distinguishing the two conditions.
Axenfeld-Rieger Syndrome: This condition causes abnormalities in the anterior segment and can present with symptoms similar to Peters anomaly. Genetic testing and clinical examination assist in differentiation.
Sclerocornea: This condition is characterized by abnormal development of the corneal stroma, which results in corneal scleralization. It can present with similar findings to Peters anomaly, but can be distinguished by a thorough clinical examination and imaging.
Peter’s Anomaly Treatment
Treatment for Peters anomaly aims to address the anterior segment’s structural abnormalities, improve visual acuity, and prevent complications. The treatment approach varies according to the severity of the condition, the specific ocular structures involved, and the patient’s overall health. Here are the main treatment options:
Surgical Intervention
Corneal Transplantation (Keratoplasty): When significant corneal opacities severely impair vision, corneal transplantation may be required. Penetrating keratoplasty (full-thickness corneal transplant) and lamellar keratoplasty (partial-thickness corneal transplant) can both restore corneal clarity and improve vision. The severity of the underlying abnormalities and the presence of other ocular issues determine the procedure’s success.
Iridocorneal Adhesion Release: Surgically removing adhesions between the iris and cornea can improve aqueous humor flow and lower intraocular pressure, thereby preventing or managing glaucoma.
Glaucoma Surgery: If secondary glaucoma occurs, surgical intervention may be required to control intraocular pressure. Trabeculectomy and the placement of glaucoma drainage devices are two procedures that can help manage glaucoma and protect the optic nerve.
Lens Surgery: When cataracts are present, cataract extraction may be necessary. This may include removing the opaque lens and, if possible, implanting an intraocular lens (IOL) to restore visual function.
Combined Procedures: In some cases, a combination of the aforementioned surgeries may be required to address multiple issues simultaneously. This multidisciplinary approach can improve visual outcomes while reducing the need for multiple surgical interventions.
Non-surgical Management
Observation: In mild cases where the corneal opacity and other abnormalities do not significantly impair vision, careful observation and regular monitoring may be adequate. This approach ensures that any progression of the condition is addressed as soon as possible.
Correction of Refractive Errors: Children with Peters anomaly frequently develop refractive errors due to structural abnormalities in the eye. Prescription glasses or contact lenses can help correct these errors by increasing visual acuity and lowering the risk of amblyopia.
Visual Rehabilitation
Amblyopia Treatment: If amblyopia (lazy eye) develops, prompt treatment is essential. Patching the unaffected eye to encourage the use of the affected eye is one treatment option, as is using atropine drops in the stronger eye to temporarily blur vision. These treatments help to strengthen the weaker eye while also improving overall visual function.
Low Vision Aids: For patients with severe visual impairment, low vision aids such as magnifying glasses, telescopic lenses, and other assistive devices can improve visual abilities and quality of life.
Supportive Care
Parental Education: It is critical to educate parents about Peters anomaly, its potential complications, and the importance of keeping treatment and follow-up appointments on schedule. Parents play an important role in the successful treatment of the condition.
Psychological Support: Addressing the psychological impact of Peters’ anomaly on both the patient and their family is critical. Counseling and support groups can assist families in dealing with the emotional and social challenges presented by the condition.
Frequently Asked Questions About Peter’s Anomaly
What causes the Peters anomaly?
During embryogenesis, developmental defects in the anterior segment of the eye cause Peters anomaly. Gene mutations in PAX6, PITX2, FOXC1, and CYP1B1 have been linked. Infections and teratogen exposure during pregnancy may also play a role.
How is the Peters anomaly diagnosed?
A thorough ophthalmic examination, including slit lamp biomicroscopy, is required to diagnose corneal opacity and iridocorneal adhesions. Ultrasound biomicroscopy, B-scan ultrasound, and optical coherence tomography (OCT) are imaging techniques used to visualize ocular structures. Genetic testing may be performed if a hereditary component is suspected.
Can the Peters anomaly affect both eyes?
Yes, Peters anomaly can affect either one or both eyes (unilateral or bilateral). Bilateral involvement typically causes more severe visual impairment and poses greater management and treatment challenges.
Is surgery always required for Peter’s anomaly?
Not every case necessitates surgery. The severity of the condition and the presence of complications such as cataracts, glaucoma, or significant corneal opacity determine the need for surgical intervention. Non-surgical treatments and regular monitoring can help manage mild cases.
What are the potential complications of Peter’s anomaly?
Complications may include corneal ulceration, secondary glaucoma, retinal detachment, cataracts, and amblyopia. Early detection and appropriate treatment are critical for managing these complications and maintaining vision.
How does the Peters anomaly affect vision?
The effect on vision varies according to severity and the specific structures involved. Mild cases may result in manageable visual impairment, whereas severe cases can cause significant vision loss or blindness. Early intervention and appropriate management are critical for achieving optimal visual outcomes.
Is it possible to prevent Peters anomaly?
There is no known way to prevent Peters anomaly, which is a congenital condition caused by developmental anomalies. Early detection and treatment are critical for managing the condition and preventing complications.
What role do parents have in managing Peter’s anomaly?
Parents play an important role in ensuring their children follow treatment plans, attend regular follow-up appointments, and use prescribed visual aids or corrective lenses. Parental education and support are critical to successful management.
Are there any support groups for families affected by Peters anomaly?
Yes, several organizations and support groups offer resources and assistance to families dealing with Peters anomaly and other congenital eye conditions. These groups provide useful information, emotional support, and practical advice.
Can children with the Peters anomaly live normal lives?
Many children with Peters anomaly can live normal, fulfilling lives if diagnosed early, treated appropriately, and managed on an ongoing basis. Visual rehabilitation and supportive care can help them overcome obstacles and realize their full potential.
Trusted Resources and Support
Books and Organizations
Books:
- “Pediatric Ophthalmology: Current Thought and A Practical Guide”* by Edward M. Wilson and Richard Saunders.
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski and Brad Bowling.
Organizations:
- The American Association for Pediatric Ophthalmology and Strabismus (AAPOS): Offers resources and support to families dealing with pediatric eye conditions, including Peters anomaly.
- The National Eye Institute (NEI) provides comprehensive information on eye health and congenital eye conditions.
- The Vision of Children Foundation: funds research and offers resources to families affected by genetic and congenital vision disorders.
Financial Aid Options
Insurance Coverage: Most health insurance policies cover the diagnosis and treatment of Peters anomaly. Patients should speak with their insurance provider about the specifics of their coverage, such as co-pays and deductibles.
Patient Assistance Programs: Pharmaceutical companies and non-profit organizations may provide patient assistance programs to help with the cost of medications and treatment. Programs such as RxAssist provide information about available resources.
Non-Profit Organizations: Organizations such as the HealthWell Foundation and the Patient Advocate Foundation provide financial assistance to patients for medical expenses, including treatments for congenital conditions like Peter’s anomaly.
Government Programs: Medicaid and the Children’s Health Insurance Program (CHIP) offer coverage to low-income families. These programs can help cover the costs of treating and caring for Peters anomaly, ensuring that children receive the medical attention they require regardless of their family’s financial situation.






