What is photophobia?
Photophobia, which comes from the Greek words “photo” (light) and “phobia” (fear), is an ocular condition characterized by an abnormal sensitivity to light. Individuals with photophobia feel discomfort or pain when exposed to light, which can range from mild irritation to severe distress. This increased sensitivity can have an impact on one’s quality of life by limiting their ability to function in bright environments and, in some cases, indoors under artificial lighting.
Understanding Photophobia
Photophobia is a symptom of a number of underlying conditions, rather than a disease in and of itself. It’s a common complaint in ophthalmology and neurology. The severity and triggers of photophobia vary greatly between individuals, making it a difficult and multifaceted issue to address.
Pathophysiology
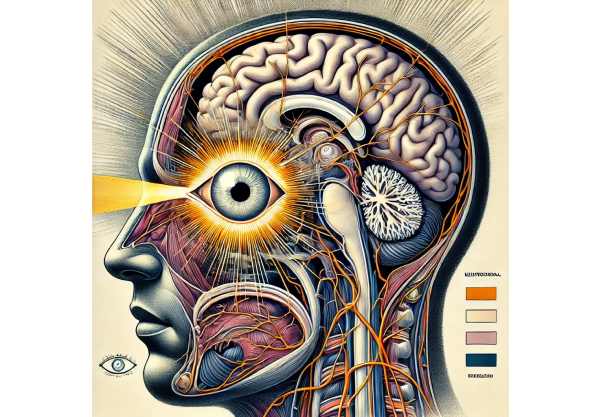
The exact mechanisms underlying photophobia are not fully understood, but they are thought to include both ocular and neurological components. Here are some important aspects of its pathophysiology:
Ocular Component: The eyes have photoreceptors that detect light. In people with photophobia, photoreceptors, particularly rod and cone cells in the retina, may become overly sensitive to light stimuli. This hyper-responsiveness can send excessive signals to the brain, causing discomfort or pain.
Neurological Component: The trigeminal nerve, which innervates the eye and surrounding structures, is essential in photophobia. When exposed to light, the trigeminal nerve sends signals to the brain. In people with photophobia, this pathway may become sensitized, resulting in an exaggerated response to light exposure.
Central Processing: The brain’s thalamus and visual cortex process visual information. Abnormalities or increased activity in these areas may contribute to the development of photophobia. Migraines and other neurological disorders can increase this sensitivity.
Common Causes
Photophobia is associated with a variety of ocular and systemic conditions. Some of the most common causes are:
Ocular Condition:
- Conjunctivitis: Inflammation of the conjunctiva, often caused by infections or allergies, can cause light sensitivity.
- Corneal Abrasions and Ulcers: Corneal damage can cause the eye to become extremely light sensitive.
- Uveitis: Inflammation of the uvea (the middle layer of the eye) can result in severe photophobia.
- Cataracts: Clouding of the eye’s lens can scatter light into the eye, increasing sensitivity.
- Dry Eye Syndrome: Insufficient tear production can cause discomfort and increased light sensitivity.
Neurological Condition:
- Migraines: Photophobia is a common migraine symptom that usually appears before or during the headache.
- Meningitis: Inflammation of the protective membranes that surround the brain and spinal cord can result in extreme light sensitivity.
- Intracranial Pressure: Conditions that raise pressure inside the skull, such as brain tumors or hydrocephalus, can cause photophobia.
- Trigeminal Neuralgia is a chronic pain condition that affects the trigeminal nerve and can cause light-induced pain.
Systemic Condition:
- Albinism: Decreased pigmentation in the eyes can cause increased light sensitivity.
- Aniridia: The partial or complete absence of the iris allows uncontrolled light to enter the eye.
- Lupus and Other Autoimmune Disorders: Systemic inflammation can damage the eyes and cause photophobia.
- Medications: Some medications, such as those used in chemotherapy or to treat tuberculosis, can cause light sensitivity as a side effect.
Psychological Impact
Photophobia’s chronic discomfort can have a negative impact on a person’s mental health. Persistent light sensitivity can cause anxiety, depression, and social isolation. The need to avoid bright environments can limit daily activities, including work, school, and social interactions. Understanding and addressing photophobia’s psychological impact is critical for effective treatment.
Symptom Variability
Photophobia symptoms can vary greatly between people, depending on the underlying cause, the intensity of light exposure, and the individual’s overall health. Common symptoms include:
Discomfort or Pain: When exposed to light, people who suffer from photophobia frequently experience sharp, burning, or throbbing pain. This pain may be localized to the eyes or manifest as a headache.
Squinting or Closing the Eyes: To reduce light exposure, people can squint, wear sunglasses indoors, or close their eyes in bright environments.
Tearing and Redness: Exposure to light can cause tearing and redness in the eyes, adding to discomfort.
Visual Disturbances: Some people have visual disturbances like glare, halos, or blurred vision, which can aggravate light sensitivity.
Nausea: In severe cases, photophobia can cause nausea and vomiting, especially in people with migraines or other neurological conditions.
Differential Diagnosis
Differentiating photophobia from other conditions with similar symptoms is critical for proper diagnosis and treatment. Conditions to consider in the differential diagnosis are:
Epilepsy: Some types of epilepsy, particularly photosensitive epilepsy, can result in light-induced seizures rather than photophobia.
Cluster Headaches: These severe headaches can cause light sensitivity, but the pain is usually more intense and limited to one eye.
Psychogenic Photophobia: Psychological factors, such as anxiety or somatic symptom disorders, can cause perceived light sensitivity in the absence of a physiological cause.
Post-Concussion Syndrome: People with a history of head injury may experience photophobia as part of a larger set of post-concussion symptoms.
Impact on Daily Life
Photophobia can have a significant impact on a person’s daily life and overall well-being. The need to avoid bright environments may lead to:
Work Limitations: Individuals may struggle to work in brightly lit offices or environments with extensive screen use.
Educational Challenges: Photophobic students may struggle in brightly lit classrooms or during outdoor activities.
Social Isolation: The desire to avoid bright social settings, such as outdoor gatherings or events with bright lighting, can result in social withdrawal.
Reduced Outdoor Activities: Photophobia can limit participation in outdoor activities, resulting in a sedentary lifestyle and potential health risks.
Importance of Comprehensive Management
Addressing photophobia requires a comprehensive approach that takes into account the underlying cause, the severity of symptoms, and the individual’s overall health. Collaboration among healthcare providers, such as ophthalmologists, neurologists, and mental health professionals, is critical for successful management. Understanding the multifaceted nature of photophobia allows healthcare providers to create individualized treatment plans that address both the physical and psychological aspects of the condition.
Diagnostic Approaches for Photophobia
A healthcare provider must conduct a thorough evaluation to determine the underlying cause and extent of light sensitivity when diagnosing photophobia. This evaluation typically consists of a patient history, clinical examination, and specialized tests. Here are the main diagnostic methods used:
Patient History
Detailed History: Obtaining a complete patient history is the first step in diagnosing photophobia. The healthcare provider will inquire about the onset, duration, and severity of the symptoms, as well as any possible triggers or exacerbating factors. Information on recent eye trauma, surgeries, or infections is critical.
Associated Symptoms: Other symptoms, such as headaches, nausea, eye redness, or vision changes, can help determine the underlying cause of photophobia.
Medication Review: Examining current and past medications can help identify any drugs that may cause light sensitivity as a side effect.
Clinical Examination
Visual Acuity Test: Measuring visual acuity helps determine whether photophobia is affecting vision. This test determines how well a person sees at various distances.
Slit Lamp Examination: A slit lamp examination enables the healthcare provider to examine the anterior segment of the eye, which includes the cornea, iris, and lens. This test can detect abnormalities such as corneal abrasions, uveitis, or cataracts that may cause photophobia.
Fundoscopy: An examination of the retina and optic nerve with an ophthalmoscope aids in the detection of retinal or optic nerve conditions that may cause photophobia.
Intraocular Pressure Measurement: Measuring intraocular pressure helps rule out glaucoma, which can cause light sensitivity.
Specialized Tests
Corneal Staining: Fluorescein staining is the process of applying a special dye to the surface of the eye to highlight any corneal abrasions, ulcers, or other abnormalities. This test is especially useful for determining the causes of photophobia due to corneal damage.
Tear Film Analysis: Assessing the quality and quantity of the tear film can aid in the diagnosis of dry eye syndrome, a common cause of photophobia. Commonly used tests include the Schirmer test and tear break-up time (TBUT).
Neurological Examination: Patients suspected of having photophobia should have a thorough neurological examination. This exam may include tests for cranial nerve function, motor and sensory function, and reflexes.
Imaging Studies: When intracranial pathology is suspected, imaging studies such as magnetic resonance imaging (MRI) or computed tomography (CT) scans may be required to diagnose conditions such as brain tumors, meningitis, or increased intracranial pressure.
Electroretinography (ERG) measures the retina’s electrical responses to light stimuli. This test can assist in diagnosing retinal conditions that may cause photophobia.
Lab Tests
Blood Tests: Blood tests can detect systemic conditions that may cause photophobia, such as autoimmune disorders, infections, or metabolic abnormalities.
Lumbar Puncture: If meningitis or other central nervous system infections are suspected, a lumbar puncture may be used to examine cerebrospinal fluid (CSF) for signs of infection or inflammation.
Effective Treatments for Photophobia
The treatment of photophobia focuses on identifying the underlying cause, managing symptoms, and improving the patient’s quality of life. Given the wide variety of conditions associated with photophobia, a tailored approach is required. Here are the main treatment strategies:
Addressing Underlying Causes
Treating Eye Conditions:
- Conjunctivitis: Bacterial conjunctivitis requires antibiotic eye drops or ointments. Viral conjunctivitis usually resolves on its own, but lubricating eye drops can help relieve symptoms.
- Corneal Abrasions and Ulcers: Treatment involves using antibiotic eye drops to prevent infection and promote healing. Lubricating eye drops or ointments can help relieve pain.
- Uveitis: Anti-inflammatory medications, such as corticosteroid eye drops, are used to relieve inflammation. In severe cases, oral corticosteroids or immunosuppressive medications may be required.
- Cataracts: The only definitive treatment for cataracts is surgical removal. This procedure replaces the cloudy lens with a clear artificial lens.
Manage Neurological Conditions:
- Migraines: Preventive medications like beta-blockers, antiepileptics, and antidepressants can help reduce the frequency and severity of migraines. Triptans and nonsteroidal anti-inflammatory drugs (NSAIDs) are common acute treatments.
- Meningitis: Prompt treatment with appropriate antibiotics or antivirals is critical. Corticosteroids can also be used to reduce inflammation.
- Increased Intracranial Pressure: Management is dependent on the underlying cause. Medication to reduce pressure, surgical interventions, and shunts to drain excess cerebrospinal fluid are all options for treatment.
- Trigeminal Neuralgia: Anticonvulsant medications, such as carbamazepine, are frequently prescribed. Refractory cases may warrant surgical intervention, such as microvascular decompression.
Symptom Relief
Light Sensitivity Management:
- Sunglasses and Tinted Lenses: Wearing UV-protective sunglasses or tinted lenses can help reduce light exposure and discomfort. Some patients benefit from lenses made specifically for photophobia, such as FL-41 tinted lenses.
- Hats and Visors: Wearing wide-brimmed hats or visors outside can help protect against bright light.
Environmental modifications:
- Adjusting Indoor Lighting: Controlling indoor lighting with dimmer switches, curtains, and blinds can help to create a more comfortable atmosphere. Replacing fluorescent bulbs with incandescent or LED bulbs that emit softer light can also help.
- Screen Filters: Installing anti-glare screens on computer monitors and using blue light filters can help reduce digital eye strain and light sensitivity.
Medications:
- Lubricating Eye Drops: Artificial tears can help treat dry eye syndrome, a common cause of photophobia. These drops help keep moisture on the eye’s surface, which reduces irritation and sensitivity.
- Analgesics and Anti-inflammatory Medications: Over-the-counter pain relievers like acetaminophen or ibuprofen can alleviate mild discomfort. In severe cases of pain, prescription medications may be required.
Behavioral Therapy:
- Cognitive Behavioral Therapy (CBT): CBT can help patients with photophobia who are anxious or have other psychological issues develop coping strategies and reduce light sensitivity.
- Biofeedback: This technique can assist patients in gaining control over their physiological responses to light exposure, potentially alleviating symptoms.
Regular Monitoring and Follow-up
Routine Eye Exams: Regular visits to an ophthalmologist are required to monitor the condition and adjust treatment as needed. These exams can aid in the detection of changes in eye health and the effective management of the underlying cause of photophobia.
Collaborative Care: For patients with systemic or neurological causes of photophobia, ophthalmologists, neurologists, and primary care physicians must work together to provide comprehensive care.
Frequently Asked Questions about Photophobia
What Causes Photophobia?
Photophobia can be caused by a variety of conditions that affect the eyes, nervous system, and overall health. Common causes include ocular conditions like conjunctivitis and uveitis, neurological conditions like migraines and meningitis, and systemic conditions like albinism and autoimmune disorders.
How is Photophobia Diagnosed?
A thorough evaluation is required for diagnosis, which includes a detailed patient history, clinical examination, and specialized tests. Visual acuity tests, slit lamp examinations, fundoscopy, corneal staining, and neurological assessments are all useful diagnostic tools. Imaging studies and lab tests may also be required.
Is it possible to cure photophobia?
The treatment of photophobia is dependent on identifying the underlying cause. While some conditions, such as conjunctivitis or migraines, can be effectively managed or resolved, others may necessitate ongoing treatment and lifestyle changes to manage symptoms.
How do I manage photophobia at home?
Managing photophobia at home entails wearing sunglasses or tinted lenses, adjusting indoor lighting, installing anti-glare screens on electronic devices, and applying lubricating eye drops. Wearing hats or visors and setting up a comfortable environment with controlled lighting can also help.
Are there special sunglasses for photophobia?
Yes, sunglasses with UV protection and polarized lenses can help reduce glare and alleviate light sensitivity. FL-41 tinted lenses are designed to filter specific wavelengths of light and have been shown to help some people with photophobia.
Can Medications Cause Photophobia?
Yes, certain medications, including antibiotics, chemotherapy drugs, and tuberculosis treatments, can cause light sensitivity as a side effect. If you suspect your medication is causing photophobia, talk to your doctor about other options.
Is photophobia indicative of a serious condition?
Photophobia can be a sign of both mild and serious conditions. While it frequently occurs alongside less serious issues such as dry eye syndrome or migraines, it can also indicate more serious conditions such as meningitis or increased intracranial pressure. It is critical to seek medical attention to determine the root cause.
Can kids develop photophobia?
Yes, children can develop photophobia for a variety of reasons, including infections, congenital conditions, and neurological problems. Early diagnosis and treatment are critical for avoiding complications and managing symptoms effectively.
How does photophobia impact daily life?
Photophobia can significantly disrupt daily life, making it difficult to work, study, or participate in social activities. It can cause social isolation, anxiety, and difficulty completing tasks in bright environments. Effective management and environmental changes can help mitigate these effects.
Which specialists treat photophobia?
Typically, ophthalmologists, neurologists, and primary care physicians are involved in diagnosing and treating photophobia. In some cases, comprehensive care may require consultation with dermatologists, infectious disease specialists, or mental health professionals.
Trusted Resources and Support
Books and Organizations
Books:
- Anthony Pane, Neil Miller, and Jane Lees wrote “The Neuro-Ophthalmology Survival Guide”.
- “Ocular Inflammation and Uveitis” by Jack J. Kanski and Carlos E. Pavesio.
Organizations:
- American Academy of Ophthalmology (AAO): Offers extensive information on ocular conditions, including photophobia, to patients and healthcare professionals.
- The American Migraine Foundation (AMF) provides information and support to people suffering from migraines and related symptoms such as photophobia.
- National Eye Institute (NEI): An extensive source of information on eye health and related conditions, including photophobia.
Financial Aid Options
Insurance Coverage: Most health insurance plans cover the diagnosis and treatment of photophobia, as well as the underlying causes. Patients should check with their insurance providers to learn about the specifics of their coverage, such as co-pays and deductibles.
Patient Assistance Programs: Pharmaceutical companies and non-profit organizations frequently provide patient assistance programs to help with the cost of medications and treatments. Programs such as RxAssist provide information about available resources.
Non-Profit Organizations: Organizations like the HealthWell Foundation and the Patient Advocate Foundation help patients pay for medical expenses, including treatments for photophobia-related conditions.
Government Programs: Medicaid, Medicare, and the Children’s Health Insurance Program (CHIP) provide coverage to eligible individuals. These programs can help cover the costs of photophobia treatment and care, ensuring that patients receive the medical attention they require regardless of their financial situation.






