What is recurrent corneal erosion?
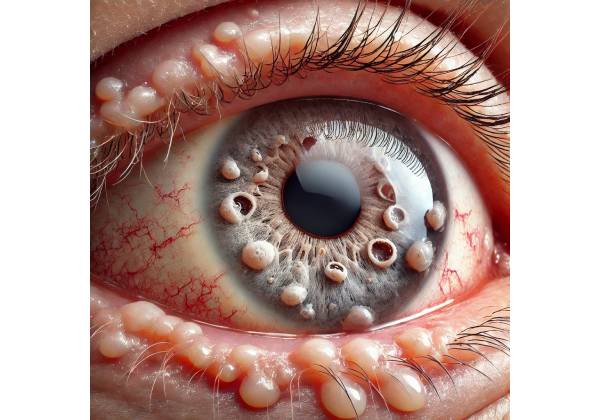
Recurrent corneal erosion (RCE) is a painful and often debilitating ocular condition characterized by repeated breakdown or detachment of the corneal epithelium, the cornea’s outermost layer. The cornea is the eye’s transparent, dome-shaped surface that covers the iris and pupil and is essential for focusing vision. The corneal epithelium serves as a barrier against infection, injury, and foreign particles. When this layer is compromised, as in RCE, it can cause severe discomfort, visual disturbances, and an increased risk of infection.
Understanding The Corneal Structure
To fully understand the nature of recurrent corneal erosion, one must first understand the structure of the cornea. The cornea consists of five distinct layers, each of which serves a specific function:
- Epithelium: The outermost layer is a thin, protective barrier that regenerates rapidly. It consists of several layers of cells that are tightly bound together.
- Bowman’s Layer: A tough, acellular layer beneath the epithelium that provides structural support and protection from injury.
- Stroma: The cornea’s thickest layer, composed of collagen fibers and keratocytes. It gives the cornea its strength, shape, and transparency.
- Descemet’s Membrane is a thin but strong layer that serves as the endothelial basement membrane.
- Endothelium: The cornea’s innermost layer, which regulates fluid levels to keep it hydrated.
RCE primarily affects the epithelial layer, where cells do not properly adhere to the underlying Bowman’s layer. This detachment can occur spontaneously, most commonly during sleep, or as a result of minor trauma. The condition’s recurrent nature is due to incomplete healing or poor epithelium adherence to the Bowman’s layer, resulting in repeated episodes of erosion.
Causes and Risk Factors
Recurrent corneal erosion can be caused by a variety of factors, which are broadly classified as traumatic, dystrophic, or idiopathic.
Traumatic RCE
Traumatic causes are the most common source of RCE. These occur when an injury, such as a scratch, abrasion, or foreign body impact, damages the corneal epithelium. Even after the initial wound has healed, the epithelium may not completely reattach to the underlying layers, leaving it vulnerable to recurrent erosions. Fingernails, makeup applicators, tree branches, and contact lenses are all potential sources of such injuries. The initial trauma disrupts the natural bond between the epithelium and the Bowman’s layer, paving the way for recurring episodes.
Dystrophic RCE
Dystrophic causes of RCE include genetic or inherited corneal disorders such as epithelial basement membrane dystrophy (EBMD), also known as map-dot-fingerprint dystrophy. In EBMD, abnormalities in the basement membrane (the structure that supports the epithelium) cause poor adhesion between the epithelial cells and the Bowman’s layer. This dystrophy can cause the epithelium to loosen and detach more easily, resulting in recurring erosions. Other dystrophic conditions that can cause RCE include Meesmann corneal dystrophy and lattice corneal dystrophy, though they are less common.
Idiopathic RCE
RCE can occur without a clear cause, which is known as idiopathic. Patients with idiopathic RCE may have recurrent episodes with no prior trauma or underlying corneal disease. The exact mechanisms underlying idiopathic RCE are unknown, but it is believed that subtle abnormalities in epithelial cells or their attachment structures may play a role.
Symptoms of Recurrent Corneal Erosion
Sudden, sharp eye pain, often described as a stabbing or burning sensation, is the hallmark symptom of recurring corneal erosion. This pain usually occurs when you wake up, as the eyelids open and pull away from the compromised epithelial layer. Pain can range from mild discomfort to severe, incapacitating pain that limits daily activities. The episodes can last a few minutes or several hours.
In addition to pain, patients with RCE may have the following symptoms:
- Blurry Vision: During and after an erosion episode, vision may become blurry due to disruption of the corneal surface, which is critical for focusing light.
- Sensitivity to Light (Photophobia): A damaged cornea may become more sensitive to light, causing discomfort in bright environments.
- Tearing: In response to corneal irritation, the body produces more tears in an attempt to flush out any perceived irritants.
- Foreign Body Sensation: Patients frequently report feeling as if something is stuck in their eye due to the roughened corneal surface.
- Redness: The affected eye may appear red or bloodshot, particularly if the erosion is associated with inflammation.
The Recurrence Cycle
One of the defining characteristics of recurrent corneal erosion is its cyclical nature. Following an initial episode of erosion, the cornea may heal within a few days, and the symptoms may disappear. However, the underlying issue—poor epithelial adhesion—is unresolved, increasing the likelihood of recurrence. Some patients may have frequent episodes, whereas others may have long periods of remission in between. Dry eyes, sleeping in a low-humidity environment, and rubbing the eyes can all exacerbate the condition and trigger new episodes.
Complications of Recurrent Corneal Erosion
While RCE is not life-threatening, it can cause a variety of complications if not treated or managed properly. The complications include:
- Corneal Scarring: Repeated episodes of erosion can cause corneal scarring, which can result in permanent vision impairment if the central visual axis is compromised.
- Secondary Infection: The compromised epithelial barrier raises the risk of bacterial infections like bacterial keratitis, which can be blinding if not treated right away.
- Chronic Pain: Persistent or frequent episodes of RCE can cause chronic ocular pain, lowering the patient’s quality of life.
Effects on Quality of Life
Recurrent corneal erosion can have a significant impact on a patient’s quality of life because it is unpredictable and the symptoms are severe. The fear of waking up in severe pain can cause anxiety and sleep disturbances. Furthermore, the need to avoid triggers, such as dry environments or certain activities, can limit daily life and negatively impact overall well-being. Patients with RCE may also feel frustrated because of the condition’s chronic nature and the possibility of recurring episodes despite treatment.
Diagnostic Techniques for Recurrent Corneal Erosion
The diagnosis of recurrent corneal erosion requires a combination of patient history, clinical examination, and specialized diagnostic tools. Accurate diagnosis is critical for developing an effective treatment plan that is tailored to the patient’s specific requirements.
Patient History
The diagnostic process begins with a detailed patient history, in which the clinician inquires about the onset, frequency, and nature of the symptoms. Important factors to consider include:
- Symptom Pattern: Knowing when symptoms appear (e.g., upon waking) and how frequently they reoccur can provide useful information. The clinician will also inquire about the severity and duration of the pain, as well as any accompanying symptoms such as blurred vision or photophobia.
- Previous Ocular Trauma: A history of previous eye injuries, particularly corneal abrasions, is critical in diagnosing RCE. Patients who have sustained a traumatic corneal injury are more likely to develop RCE later.
- Family History: Because some forms of RCE are associated with genetic conditions such as epithelial basement membrane dystrophy, a family history of similar symptoms or corneal dystrophies may be relevant.
- Environmental Factors: The clinician may inquire about the patient’s sleeping environment, contact lens use, and exposure to dry or windy conditions, all of which can influence the recurrence of erosion.
Clinical Examination
A thorough clinical examination is required to diagnose RCE. The exam typically includes:
- Slit-Lamp Biomicroscopy: This is the primary method for examining the cornea in detail. Using a slit lamp, the clinician examines the corneal surface for epithelial defects, microcysts, or Bowman’s layer irregularities. Fluorescein dye is frequently applied to the eye, which stains areas of epithelial disruption and makes them more visible in blue light.
- Eversion of the Eyelids: The clinician may also examine the inner surface of the eyelids for any abnormalities, such as papillae, that could contribute to recurrent corneal trauma.
Additional Diagnostic Tools
In some cases, additional diagnostic tools may be used to confirm the diagnosis or determine the extent of corneal involvement:
- Anterior Segment Optical Coherence Tomography (OCT): OCT is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the cornea. It can detect subtle abnormalities in the corneal layers that a slit lamp may miss.
- Corneal Topography: This imaging technique maps the curvature of the cornea’s surface, revealing irregularities that may contribute to RCE, especially in cases involving corneal dystrophies.
Recurrent Corneal Erosion Management
Managing recurrent corneal erosion (RCE) necessitates a multifaceted approach that addresses both the immediate symptoms and the root causes of the condition. Treatment options range from conservative medical management to advanced surgical interventions, depending on the severity and frequency of the episodes. The goal of treatment is to promote corneal epithelial healing, lower the risk of recurrence, and relieve the patient’s discomfort.
Conservative Medical Management
For many patients, conservative treatments can effectively manage RCE, especially in mild cases or when episodes are infrequent.
- Lubrication: The use of lubricating eye drops or ointments is an essential component of conservative treatment. These products help keep moisture on the ocular surface, which reduces friction between the eyelid and the cornea, a common cause of epithelial disruption. Patients are frequently advised to apply lubricating ointment before going to bed to keep their eyes moist overnight and prevent the eyelids from sticking to the cornea when they wake up.
- Hypertonic Saline Drops and Ointments: Hypertonic saline (5%) drops and ointments can be used to draw fluid out of the corneal epithelium, thereby reducing epithelial edema and improving epithelial cell adhesion to the underlying Bowman’s layer. These are typically applied before going to bed and when you wake up.
- Bandage Contact Lenses: When conservative treatment is insufficient, a therapeutic bandage contact lens may be prescribed. These soft lenses protect the corneal surface by forming a barrier between the eyelid and the cornea, allowing the epithelium to heal more efficiently. Bandage lenses are typically used alongside antibiotic eye drops to prevent infection during the healing process.
- Oral Medications: In some cases, oral tetracyclines (such as doxycycline) may be prescribed due to their anti-inflammatory properties and ability to inhibit matrix metalloproteinases (MMPs), enzymes that can degrade the corneal epithelium and exacerbate erosion. Additionally, oral vitamin C (ascorbic acid) supplements may be recommended to aid in collagen formation and corneal healing.
Surgical and Procedural Interventions
Patients who do not respond well to conservative treatments or have frequent recurrences may require surgical or procedural interventions.
- Anterior Stromal Puncture: This minimally invasive procedure involves making tiny punctures in the cornea’s anterior stroma with a fine needle or laser. The goal is to strengthen the corneal epithelium’s adhesion to the underlying layers by encouraging scar tissue formation at the erosion site. This procedure is usually done under topical anesthesia and has been shown to reduce the number of recurrent erosions.
- Phototherapeutic Keratectomy (PTK): PTK is a laser procedure that removes the superficial corneal layers, including the irregular epithelium and Bowman’s layer, using an excimer laser. This technique can smooth the corneal surface and eliminate any underlying irregularities that cause poor epithelial adhesion. PTK is especially effective in RCE patients with corneal dystrophies such as epithelial basement membrane dystrophy (EBMD).
- Debridement: In severe cases, manual debridement of the loose or irregular epithelium may be required. This entails gently scraping away damaged epithelial cells to allow for the formation of a new, more securely attached epithelium. Debridement is frequently combined with other treatments, such as the use of a bandage contact lens or PTK, to improve healing and prevent recurrence.
- Amniotic Membrane Transplantation: When other treatments fail, amniotic membrane transplantation may be considered. The amniotic membrane, which has anti-inflammatory and anti-scarring properties, is applied to the cornea to promote healing and reduce the likelihood of recurrence. This procedure is typically reserved for severe or refractory cases of RCE.
Long-term Management and Prevention
Long-term management of RCE focuses on preventing recurrences and preserving ocular surface integrity. Even after the symptoms have subsided, patients are frequently advised to continue using lubricating eye drops or ointments, especially before going to bed. Regular follow-up appointments with an ophthalmologist are required to monitor the condition and adjust the treatment plan as necessary.
For patients with underlying conditions like epithelial basement membrane dystrophy, managing the dystrophy is critical to avoiding future episodes of RCE. This may entail the ongoing use of hypertonic saline drops, lubricants, and periodic evaluations for potential surgical intervention.
Most patients with recurrent corneal erosion can achieve significant symptom relief and reduce the frequency of erosive episodes by combining medical, surgical, and preventive strategies, ultimately improving their quality of life.
Trusted Resources and Support
Books
- “Corneal Erosions and Dystrophies: Clinical and Therapeutic Approaches” by J. Bradley Randleman – A comprehensive guide on the diagnosis and treatment of corneal erosions, including recurrent cases.
- “Corneal Disorders: Clinical Diagnosis and Management” by Stephen J. Tuft and Mark J. Mannis – A detailed resource covering various corneal conditions, with a focus on management strategies.
Organizations
- American Academy of Ophthalmology (AAO) – Provides resources, guidelines, and patient education materials on corneal conditions, including recurrent corneal erosion.
- The Cornea Society – A professional organization dedicated to the advancement of knowledge and treatment of corneal diseases, offering support and information for both patients and practitioners.










