What is Multiple Sclerosis Ocular Issues?
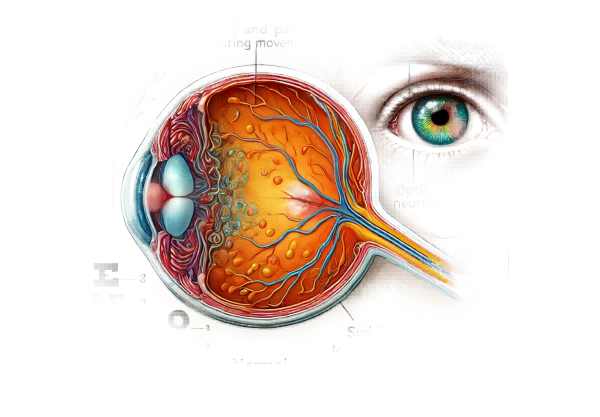
Multiple sclerosis (MS) is a chronic autoimmune disease affecting the central nervous system, resulting in a variety of neurological symptoms. Ocular issues are among the most common and can have a significant impact on a patient’s quality of life. Ocular manifestations of MS include optic neuritis, internuclear ophthalmoplegia, and nystagmus. These conditions can cause symptoms like blurred vision, double vision, and involuntary eye movements, which can range in severity and duration. Early detection and treatment are critical for reducing these visual impairments and maintaining overall eye health.
Detailed Investigation of Multiple Sclerosis Ocular Issues
Optic Neuritis
Optic neuritis is among the most common ocular manifestations of Multiple Sclerosis. It is characterized by optic nerve inflammation, which can result in a sudden loss of vision, eye movement pain, and color vision deficits. Optic neuritis is often the first symptom of MS and, if not treated properly, can result in temporary or permanent vision loss.
Pathophysiology
Optic neuritis causes inflammation due to an autoimmune attack on the myelin sheath that surrounds the optic nerve. This demyelination interrupts the transmission of visual information from the eye to the brain, resulting in visual impairment. Repeated episodes of inflammation can result in cumulative damage to the optic nerve.
Symptoms
- Vision Loss: Patients usually experience a sudden onset of vision loss in one eye, ranging from mild blurriness to total blindness.
- Eye Pain: Pain, particularly during eye movement, is a common symptom.
- Color Vision Changes: Affected individuals frequently report a decrease in color perception, particularly the appearance of washed-out colors.
Internuclear Ophthalmoplegia (INO)
Another ocular complication associated with MS is internuclear ophthalmoplegia, which is defined as impaired horizontal eye movement. Lesions in the medial longitudinal fasciculus (MLF), a nerve tract that coordinates eye movements, cause it.
Pathophysiology
Lesions in the MLF disrupt communication between the cranial nerves that control the lateral and medial rectus muscles, which coordinate horizontal eye movements. The affected eye fails to move inward when looking to the side, resulting in double vision.
Symptoms
- Diplopia (Double Vision): Patients frequently report double vision, especially when looking to the side.
- Convergence Weakness: Difficulty getting the eyes to focus on nearby objects.
- Nystagmus in the Abducting Eye: The eye that moves outward may have jerky movements, known as nystagmus.
Nystagmus
Nystagmus is an involuntary, rhythmic oscillation of the eyes that is also a common ocular issue in MS. It has the potential to significantly impair vision while also affecting balance and coordination.
Pathophysiology
Demyelination of neural pathways involved in eye movement control is usually the cause of nystagmus in MS. This demyelination disrupts normal signaling, resulting in abnormal and involuntary eye movements.
Symptoms
- Rhythmic Eye Movements: Patients may notice slow, drifting eye movements followed by quick, corrective saccades.
- Vision Impairment: Continuous movement can result in blurred or unstable vision.
- Vertigo and Dizziness: Due to the disruption in visual and vestibular coordination, patients may experience balance problems.
Uveitis
Uveitis, while less common than optic neuritis, can affect MS patients. Uveitis is an inflammatory condition affecting the uveal tract, which includes the iris, ciliary body, and choroid.
Pathophysiology
Although the exact mechanism linking uveitis to MS is unknown, it is thought to be another manifestation of MS’s autoimmune inflammatory process. This inflammation can cause a variety of complications, including cataracts and glaucoma.
Symptoms
- Eye Redness: Redness and inflammation in the eyes.
- Pain: Eye aches and discomfort.
- Photophobia: sensitivity to light.
- Blurred Vision: A result of inflammation and associated complications.
Ocular Myasthenia
MS patients may also experience ocular myasthenia, a muscle weakness that affects eye movements and eyelids. It can cause symptoms like ptosis (drooping eyelids) and diplopia.
Pathophysiology
Ocular myasthenia occurs when the immune system produces antibodies that interfere with nerve-muscle communication, resulting in muscle weakness. This can have an impact on both the muscles that control eye movements and those that lift the eyelids.
Symptoms
- Ptosis is drooping of one or both eyelids.
- Diplopia: Eye misalignment causes double vision.
- Eye Fatigue: Increased muscle fatigue in the eyes after use.
Visually evoked potentials (VEP)
Visual Evoked Potentials (VEP) are not symptoms, but rather a diagnostic tool for detecting abnormalities in the visual pathways that may indicate MS.
Pathophysiology
VEP tests measure the brain’s electrical response to visual stimuli. In MS, demyelination can slow or disrupt the transmission of visual information from the eyes to the brain, resulting in delayed or abnormal VEP results.
Symptoms
- None: VEP is a diagnostic tool that does not cause symptoms but can help diagnose and understand the extent of visual pathway involvement in MS.
Diagnostic methods
The accurate diagnosis of ocular issues in MS requires a combination of clinical evaluation, imaging studies, and specialized tests to assess visual function and neurological health.
Clinical Evaluation
A thorough clinical evaluation by an ophthalmologist or neurologist is required. This includes a thorough patient history that focuses on the onset and progression of symptoms, prior neurological issues, and any other systemic conditions. A thorough eye exam evaluates visual acuity, color vision, eye movements, and pupil reactions.
Optical Coherence Tomography(OCT)
Optical Coherence Tomography (OCT) is a non-invasive imaging technique that generates high-resolution cross-sections of the retina and optic nerve head. OCT can detect thinning of the retinal nerve fiber layer, a sign of optic nerve damage in MS.
Magnetic Resonance Imaging (MRI)
MRI of the brain and orbits is essential for diagnosing MS and its ocular symptoms. MRI can detect demyelinating lesions in the optic nerves, brainstem, and other areas of the central nervous system. The presence of these lesions aids in the diagnosis of MS and determines the extent of disease involvement.
Visually evoked potentials (VEP)
VEP tests measure the brain’s electrical activity in response to visual stimuli. The test uses electrodes on the scalp to record the brain’s response to visual patterns. Delays in the VEP response may indicate demyelination in the optic nerve pathways, confirming the presence of optic neuritis or other visual pathway involvement in MS.
Fundus Examination
A fundus examination with an ophthalmoscope allows for direct visualization of the optic disc and retina. This can aid in detecting symptoms of optic neuritis, such as optic disc swelling or pallor, as well as other retinal abnormalities associated with MS.
Eye Movement Tests
Specialized tests that assess eye movements and alignment are critical for diagnosing conditions such as internuclear ophthalmoplegia and nystagmus. These tests may include prism and cover tests to evaluate eye coordination and alignment.
Multiple Sclerosis Ocular Issues Treatment
The treatment of ocular issues in Multiple Sclerosis (MS) focuses on symptom management, inflammation reduction, and complications prevention. Given the wide range of MS-related ocular conditions, treatments are tailored to specific manifestations such as optic neuritis, internuclear ophthalmoplegia, and nystagmus.
Optical Neuritis Treatment
- Corticosteroids: The primary treatment for acute optic neuritis is high-dose intravenous corticosteroids like methylprednisolone, followed by a tapering course of oral prednisone. This treatment helps to reduce inflammation and speed up the recovery of visual function. However, it has no effect on the long-term prognosis for vision.
- Plasma Exchange (PLEX): If corticosteroids do not work to treat severe cases of optic neuritis, plasma exchange therapy may be considered. PLEX entails removing the patient’s plasma and replacing it with donor plasma to eliminate inflammatory factors.
Internuclear Ophthalmoplegia Treatment
- Symptomatic Management: Internuclear ophthalmoplegia usually resolves on its own with time. In the acute phase, symptomatic treatment with prism glasses can help relieve double vision. These glasses correct the alignment of visual images, reducing diplopia.
- Physical Therapy: Eye movement exercises and physical therapy can help improve coordination and alleviate INO symptoms over time.
Nystagmus Treatment
- Medications: Baclofen, gabapentin, and memantine are three medications that can help manage nystagmus by reducing the frequency and severity of involuntary eye movements.
- Vision Aids: Wearing special glasses or contact lenses designed to reduce the effects of nystagmus on vision can be beneficial.
- Botulinum Toxin Injections: In some cases, injecting botulinum toxin into the eye muscles may help control severe nystagmus by reducing muscle activity.
Uveitis Treatment
- Corticosteroids: Uveitis inflammation can be managed with topical, periocular, or systemic corticosteroids. The severity and location of the inflammation determine the appropriate administration.
- Immunosuppressive Agents: Immunosuppressive medications like methotrexate, cyclosporine, or azathioprine can help control the autoimmune response in chronic or refractory uveitis.
Emerging Therapies
- Monoclonal Antibodies: New treatments based on monoclonal antibodies, such as ocrelizumab and natalizumab, have shown promise in treating MS and its ocular manifestations by targeting specific immune system components.
- Stem Cell Therapy: Research into stem cell therapy is currently underway, with the goal of regenerating damaged optic nerve tissue and restoring vision in MS patients.
- Neuroprotective Agents: Researchers are looking into drugs that protect nerve cells from damage and promote regeneration in order to treat MS-related optic neuritis and other ocular issues.
- Gene Therapy: Advances in gene therapy have the potential to treat genetic components of MS, resulting in targeted and long-term relief from MS symptoms, including ocular issues.
Supportive Care
- Rehabilitation: Vision rehabilitation services, such as low-vision aids and adaptive technologies, can help patients manage their visual impairment and improve their quality of life.
- Counseling and Support Groups: Psychological support and counseling can assist patients in coping with the emotional and psychological effects of vision loss and other MS-related difficulties.
Effective Ways to Improve and Prevent Multiple Sclerosis Ocular Issues
- Regular Eye Exams: Seek regular eye exams from an ophthalmologist to monitor ocular health and detect early signs of MS-related eye conditions.
- Prompt Treatment: If you notice any sudden changes in your vision, such as blurriness, double vision, or eye pain, seek medical attention right away to ensure timely intervention and management.
- Manage MS: Follow the prescribed MS treatments and medications to reduce overall disease activity and the risk of ocular complications.
- Healthy Lifestyle: Eat a well-balanced diet, exercise regularly, and avoid smoking to improve overall health and reduce inflammation.
- Protect Your Eyes: Wear protective eyewear to avoid eye injuries that can worsen MS-related ocular problems.
- Manage Stress: Use stress-reduction techniques like mindfulness, meditation, or yoga to help manage stress, which can lead to MS flare-ups.
- Stay Informed: Learn more about MS and its ocular symptoms. Understanding the symptoms and treatment options allows you to take an active role in your own health care.
- Follow-Up Care: Keep scheduled follow-up appointments and monitoring plans with your healthcare providers to ensure ongoing management and treatment adjustments as needed.
- Vaccinations: Stay up to date on vaccinations to avoid infections that can cause MS relapses and harm ocular health.
- Collaborative Care: Collaborate with a multidisciplinary healthcare team, including neurologists, ophthalmologists, and physical therapists, to manage MS and its ocular complications holistically.
Trusted Resources
Books – “Multiple Sclerosis: A Guide for the Newly Diagnosed” by Nancy J. Holland and T. Jock Murray.
Read “Optic Nerve Disorders: Diagnosis and Management” by Jane W. Chan and “The Multiple Sclerosis Manifesto: Action to Take, Principles to Live By” by Julie Stachowiak.
Online Resources.
The National Multiple Sclerosis Society (NMSS)(https://www.nationalmssociety.org)
- American Academy of Neurology (AAN).
- [The Multiple Sclerosis Foundation].(https://msfocus.org)






