What is eyelid squamous cell carcinoma?
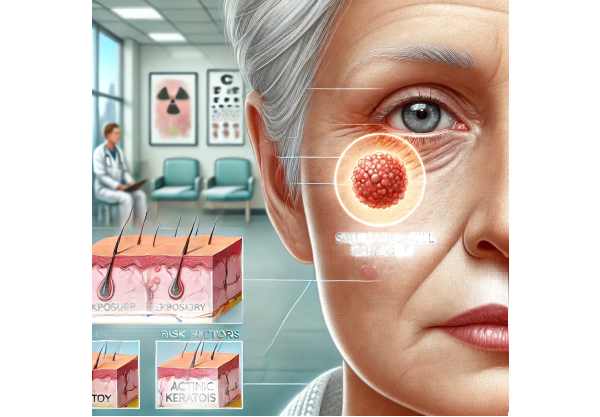
Eyelid squamous cell carcinoma (SCC) is a skin cancer that develops from squamous cells in the epidermis, the skin’s outermost layer. It is the second most common malignant tumor on the eyelid, after basal cell carcinoma. Eyelid SCC can occur on any part of the eyelid, but it is most common on the lower eyelid due to increased exposure to ultraviolet (UV) radiation. This condition is locally aggressive and has the potential to metastasize if not treated immediately. Early detection and intervention are critical for preventing serious complications and preserving ocular function and appearance.
Comprehensive Examination of Eyelid Squamous Cell Carcinoma
Epidemiology
Squamous cell carcinoma of the eyelid is uncommon, but it accounts for a significant proportion of eyelid malignancies. It primarily affects older adults, especially those with fair skin and a history of prolonged sun exposure. The incidence of eyelid SCC rises with age, and men are more commonly affected than women. Chronic UV exposure, immunosuppression, and history of radiation therapy are all risk factors. Furthermore, people who have had actinic keratosis or human papillomavirus (HPV) infection are more likely to develop the condition.
Pathophysiology
Eyelid SCC develops from the epidermis’ squamous epithelial cells. Chronic UV radiation exposure damages DNA, resulting in mutations in tumor suppressor genes and oncogenes, which promote uncontrolled cell proliferation. Actinic keratosis and Bowen’s disease are two examples of precursor lesions that can lead to this cancer. The tumor spreads locally and can invade surrounding structures such as the orbit, conjunctiva, and even the globe. The risk of metastasis to regional lymph nodes and distant organs rises with tumor size and depth of invasion.
Clinical Presentation
The clinical presentation of eyelid SCC varies greatly, making early detection difficult. Common features include:
- Nodular Lesions:
- The most common appearance is a firm, nodular mass with a rough, scaly texture. The lesion may ulcerate and bleed.
- **Ulcerative Lesion:
- Some patients present with a persistent, non-healing ulcer with raised, rolled edges. This form is frequently mistaken for benign conditions like chronic blepharitis or chalazion.
- Plaque-like Lesion:
- SCC can also appear as a flat, reddish, scaly plaque that resembles eczema or psoriasis.
- Papillomatous Lesion:
- In some cases, the tumor presents as a wart-like growth with a verrucous surface.
- Local invasion:
- Advanced tumors can invade surrounding tissues, resulting in significant eyelid deformity, eyelash loss (madarosis), and functional impairment.
- Symptoms:
Symptoms may include itching, pain, and irritation. Some patients report having a foreign body in their eye or experiencing increased tearing.
Differential Diagnosis
The wide variety of presentations necessitates differentiation from other conditions:
- basal cell carcinoma:
- The most common type of eyelid cancer, characterized by a pearly nodule, telangiectasias, and a central ulcer. It grows slowly and rarely metastasises.
- Sebaceous Gland Carcinoma:
- A rare but aggressive tumor of the sebaceous glands that frequently manifests as recurring chalazia or diffuse eyelid thickening.
- Actinic Keratosis:
- A precancerous lesion caused by sun damage that appears as a rough, scaly patch in sun-exposed areas.
- Keratoacanthoma:
- A benign, rapidly growing lesion that may resemble SCC. It usually resolves spontaneously, but it can be difficult to distinguish clinically from SCC.
- Chronic blepharitis:
- Eyelid margin inflammation, which is frequently misdiagnosed as early SCC due to the similar symptoms of redness, swelling, and irritation.
Risk Factors
There are several risk factors that contribute to the development of eyelid SCC.
- UV Radiation:*
- The most significant risk factor is prolonged exposure to UV radiation. UV rays cause DNA damage and mutations, which lead to cancer.
- Fair skin:
- People with fair skin, light hair, and blue or green eyes are more vulnerable due to lower levels of melanin, which provides some protection against UV radiation.
- Age:
- The risk rises with age, indicating cumulative UV exposure and DNA damage over time.
- Immunosuppression:
- Conditions such as HIV/AIDS, organ transplantation, and long-term use of immunosuppressive medications raise the risk.
- Previous Radiation Treatment:
- Radiation therapy for other cancers may increase the risk of developing SCC in the treated area.
- Human Papillomavirus (HPV) infection:
- Certain HPV strains are associated with a higher risk of developing SCC.
Complications
Untreated or advanced eyelid SCC can result in a variety of complications:
- Local Tissue Destruction
- The tumor has the potential to invade adjacent structures, including the orbit, resulting in significant tissue destruction and functional impairment.
- Metastasis:
- SCC can spread to regional lymph nodes and distant organs such as the lungs, liver, and bones. Metastasis dramatically worsens the prognosis.
- Recurrence:
- Even after treatment, SCC has a high risk of recurrence, necessitating ongoing follow-up and monitoring.
- Cosmetic and Functional Impairments:
- Extensive surgical resection may be required, potentially resulting in cosmetic deformity and impaired eyelid function, compromising vision and eye protection.
Prognosis
The prognosis of eyelid SCC is determined by a number of factors, including tumor size, depth of invasion, metastasis, and treatment efficacy. Early-stage tumors treated promptly have a good prognosis and a high cure rate. However, advanced tumors with regional or distant metastasis have a poorer prognosis. Regular follow-up is required to monitor for recurrence and promptly address any complications.
Eyelid squamous cell carcinoma Diagnostic methods
Clinical Examination
The first step in diagnosing eyelid SCC is to conduct a thorough clinical examination with an ophthalmologist or dermatologist.
- Visual inspection:
- The eyelid is carefully examined to determine the lesion’s size, shape, color, and surface characteristics. Any indications of ulceration, bleeding, or induration are closely monitored.
- Palpation:
- The lesion is gently palpated to assess its consistency and look for any underlying masses or fixation to deeper tissues. To rule out lymphadenopathy, regional lymph nodes are palpated as well.
- Slit Lamp Examination:
- A slit-lamp microscope is used to examine the lesion in greater detail, including the eyelid margins, conjunctiva, and cornea. This examination can aid in detecting any involvement of adjacent ocular structures.
Biopsy and Histological Examination
A biopsy and histopathological examination are necessary to make a definitive diagnosis of SCC.
- Incisional biopsy:
- For larger lesions, an incisional biopsy is performed by removing a portion of the tumor for microscopic examination. This helps to confirm the diagnosis and evaluate the tumor’s histological characteristics.
- Excisional biopsy:
- For smaller lesions, an excisional biopsy involves removing the entire tumor, which provides a definitive diagnosis and is frequently used as a therapeutic procedure.
- Histopathologic Features:
- The biopsy sample is examined under a microscope for SCC-specific characteristics such as atypical squamous cells, keratin pearls, and invasive growth patterns. Immunohistochemical staining can be used to distinguish SCC from other cancers.
Imaging Studies
Imaging studies are used to assess the extent of the tumor and detect any metastasis.
- CT Scans:
- A CT scan of the orbit and head provides detailed images of the bony structures, allowing for the assessment of any invasion into the orbit or adjacent tissues. It is also effective at detecting regional lymphadenopathy.
- MRI:
- MRI is especially useful for determining soft tissue involvement and distinguishing the tumor from nearby structures. It is recommended for determining orbital and intracranial extension.
- Ultrasound:
- High-frequency ultrasound can produce detailed images of the anterior segment, allowing for the assessment of tumor size, depth, and involvement of surrounding structures.
Lymph Node Assessment
Assessing regional lymph nodes is critical for staging and treatment planning.
- Fine Needle Aspiration Biopsy(FNAB):
- In FNAB, cells are extracted from an enlarged lymph node using a thin needle for cytological examination. This helps to determine whether the cancer has spread to the lymph nodes.
- The Sentinel Lymph Node Biopsy:
- In this procedure, a tracer is injected near the tumor to identify the sentinel lymph node, which is the first place cancer cells are likely to spread. The sentinel lymph node is then extracted and examined for the presence of cancer cells.
Lab Tests
Laboratory tests may be performed to assess the patient’s overall health and aid in the diagnosis.
- Complete Blood Count(CBC):
- A complete blood count (CBC) can help identify signs of infection or underlying conditions that may impact treatment.
- Liver and Kidney Function Testing:
- These tests evaluate the patient’s overall health and organ function, which is useful when planning treatment.
Eyelid squamous cell carcinoma Treatment
- Surgical excision:
- Eyelid squamous cell carcinoma (SCC) is treated primarily through surgical excision with clear margins. The goal is to completely remove the tumor while retaining as much eyelid structure and function as possible. Mohs micrographic surgery is frequently preferred due to its high cure rate and tissue sparing benefits. This technique entails gradually removing and microscopically examining tissue until no cancer cells remain, resulting in complete tumor removal with minimal loss of healthy tissue.
- Cryotherapy:
- Cryotherapy is the use of extreme cold to eliminate cancer cells. This method can be used in conjunction with surgical excision, especially for tumors that have spread diffusely or superficially. Cryotherapy can help reduce the risk of local recurrence.
- Radiation Therapy:
- Radiation therapy is an option for patients who are not good candidates for surgery due to medical conditions or tumor location. External beam radiation can be used to control local disease as a primary treatment or as an adjuvant therapy after surgery. Brachytherapy, which involves placing radioactive sources close to the tumor, offers targeted treatment while causing minimal damage to surrounding tissues.
- Topical Chemotherapy:*
Topical chemotherapy agents like 5-fluorouracil (5-FU) or imiquimod can be used to treat superficial lesions or SCC in situ. These medications are administered directly to the tumor in order to destroy cancerous cells. This non-invasive treatment is especially beneficial for patients who cannot have surgery. - Systematic Chemotherapy:
- Systemic chemotherapy is typically used for metastatic or recurring SCC. Agents like cisplatin and 5-FU can help control disease spread. Chemotherapy is typically used in conjunction with other treatment options, such as surgery or radiation.
Innovative and Emerging Therapies
- Target Therapy:
- Targeted therapy refers to drugs that specifically target molecular pathways involved in tumor growth and progression. Agents that target the epidermal growth factor receptor (EGFR), such as cetuximab, have shown promise in treating SCC by reducing cancer cell proliferation and survival.
- Immunotherapy:
- Immunotherapy uses the body’s immune system to identify and eliminate cancer cells. Checkpoint inhibitors such as pembrolizumab and nivolumab, which target the PD-1/PD-L1 pathway, are being studied for their efficacy in SCC. These therapies are especially beneficial for tumors that do not respond to standard treatments.
- Photodynamic Treatment (PDT):
- Photodynamic therapy (PDT) uses photosensitizing agents and light exposure to produce reactive oxygen species that selectively kill cancer cells. This minimally invasive treatment may be effective for superficial SCC and early-stage lesions.
- Genetic Therapy:
- The goal of gene therapy is to correct the genetic defects that contribute to cancer development. Clinical trials are being conducted to investigate techniques for delivering normal copies of genes, such as tumor suppressor genes, or silencing oncogenes. This approach shows promise for more personalized cancer treatment.
- Stem Cell Treatment:
- Stem cell therapy research focuses on the regeneration of damaged tissues and the restoration of normal function following extensive surgical resection. This approach is still in the experimental stages, but it shows promise for future applications.
Multidisciplinary Approach
Eyelid SCC is frequently treated using a multidisciplinary approach that includes ophthalmologists, oncologists, dermatologists, and reconstructive surgeons. This collaboration provides comprehensive care, addressing both oncologic and cosmetic aspects of treatment to improve patient outcomes.
Best Practices for Avoiding Eyelid Squamous Cell Carcinoma
- Apply Sun Protection:
- Wear broad-spectrum sunscreen with an SPF of at least 30 on your face, including your eyelids, whenever you go outside. Wear UV-protective sunglasses and a wide-brimmed hat to protect your face from direct sunlight.
- Avoid tanning beds.
- Avoid using tanning beds, which emit concentrated UV radiation and significantly increase the risk of developing skin cancers, including SCC.
- Regular Skin Examination:
- Conduct regular self-examinations of your skin, including the eyelids, to detect new or changing lesions early. Schedule an annual skin check with a dermatologist for professional evaluation.
- Avoiding Chronic Irritation:
- Avoid dust, chemicals, and other irritants to keep your eyes from becoming chronically irritated. Wear protective eyewear in situations where exposure is unavoidable.
- Lead a Healthy Lifestyle:
- Live a healthy lifestyle that includes a balanced diet high in antioxidants, regular physical activity, and no smoking. These practices improve overall skin health and immune function.
- Monitor and treat precancerous lesions.
- Monitor any precancerous lesions, such as actinic keratosis. Seek prompt treatment for these lesions to avoid progression to SCC.
- Educate Yourself.
- Be aware of the risk factors and early signs of eyelid SCC. Knowledge enables you to take preventive measures and, if necessary, seek medical advice right away.
Trusted Resources
Books
- “Clinical Ophthalmic Oncology: Eyelid and Conjunctival Tumors” by Arun D. Singh
- “Ocular Surface Disease: Cornea, Conjunctiva and Tear Film” by Edward J. Holland
- “The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease” by Nika Bagheri, Charles Calvo, Alia Durrani
- “Comprehensive Ophthalmology” by AK Khurana










