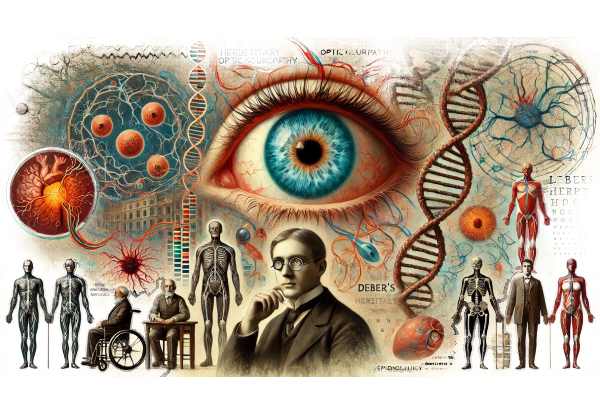
What causes Leber’s Hereditary Optic Neuropathy?
Leber’s hereditary optic neuropathy (LHON) is a rare inherited mitochondrial disorder that causes acute or subacute loss of central vision. This condition primarily affects young adults and is caused by mitochondrial DNA mutations that impair optic nerve function. LHON-related vision loss usually starts in one eye and spreads to the other, resulting in severe central vision impairment. LHON is genetic in nature, so genetic counseling and family history are important components of diagnosis and management.
Detailed Investigation of Leber’s Hereditary Optic Neuropathy
Leber’s hereditary optic neuropathy (LHON) is named for Dr. Theodor Leber, who first described the condition in 1871. LHON is unique among mitochondrial disorders in that it involves mutations in mitochondrial DNA rather than nuclear DNA. This section delves into the genetic basis, pathophysiology, clinical presentation, epidemiology, and how LHON affects patients’ lives.
Genetic Basis and Pathophysiology
LHON is primarily caused by mitochondrial DNA mutations that are inherited from the mother. The three most common mutations associated with LHON include:
- MT-ND1 (G3460A) 2. MT-ND4 (G11778A) 3. MT-ND6 (T14484C)
These mutations affect the complex I subunit of the mitochondrial respiratory chain, resulting in reduced cellular energy production. The optic nerve is especially susceptible to mitochondrial dysfunction due to its high energy demands. Defective energy production causes increased oxidative stress and subsequent degeneration of retinal ganglion cells and axons, which leads to optic neuropathy.
Clinical Presentation
LHON typically affects young adults, with the peak onset occurring between the ages of 15 and 35. However, cases have been reported in people of different ages. LHON has three distinct clinical phases: preclinical, acute, and chronic.
- Preclinical Phase: During this stage, people with LHON mutations may be asymptomatic. Some may have subclinical abnormalities detectable by specialized tests such as optical coherence tomography (OCT) or electrophysiological studies.
- Acute Phase: This phase is distinguished by the sudden onset of painless, central vision loss in one eye, followed by involvement of the second eye within weeks or months. The distinguishing features during this phase include:
- Central Scotoma: A central blind spot that reduces the ability to see fine detail.
- Dyschromatopsia: Difficulty discriminating colors, especially red-green color defects.
- Optic Disc Hyperemia: Fundoscopic examination reveals swelling and redness of the optic disc.
- Chronic Phase: Over time, the acute phase gives way to the chronic phase, in which the vision loss stabilizes. The loss of retinal ganglion cells causes the optic discs to atrophize and appear pale. Visual acuity remains significantly reduced, rendering the affected individuals legally blind.
Epidemiology
LHON is a rare condition, with an estimated prevalence of one in every 50,000 people. It affects men more than women, with a male-to-female ratio of roughly 4:1. Despite having the same mutation, not all people develop the disease, a condition known as incomplete penetrance. Environmental factors, genetic modifiers, and hormonal differences are thought to influence LHON expression.
Effects on Quality of Life
LHON causes sudden and severe vision loss, which has serious consequences for affected individuals and their families. Key challenges include:
- Educational and Occupational Limitations: Central vision loss severely impairs reading, writing, and other tasks that require fine visual acuity, affecting academic performance and job opportunities.
- Psychosocial Impact: A sudden onset of vision loss can cause emotional distress, depression, and anxiety. Support from mental health professionals and patient advocacy groups is critical.
- Dependency and Mobility Issues: People with LHON frequently struggle with daily activities and may require assistance or adaptive technologies to remain independent.
Differential Diagnosis
Several other conditions can cause similar symptoms, so an accurate diagnosis is essential. Differential diagnoses to consider are:
- Optic Neuritis: Often associated with multiple sclerosis, optic neuritis causes acute vision loss and pain with eye movement.
- Dominant Optic Atrophy: A hereditary condition characterized by progressive vision loss and optic atrophy that typically begins in childhood.
- Toxic or Nutritional Optic Neuropathy: These conditions, caused by toxins (e.g., methanol) or deficiencies (e.g., vitamin B12), can resemble the symptoms of LHON.
Diagnostic Techniques for Leber’s Hereditary Optic Neuropathy
Leber’s hereditary optic neuropathy (LHON) is diagnosed using a combination of clinical, genetic, and advanced imaging techniques. Early and accurate diagnosis is critical for managing the condition and offering appropriate genetic counseling.
Clinical Evaluation
- Ophthalmic Examination: The first step in diagnosing LHON is to have a comprehensive eye exam by an ophthalmologist. Key components are:
- Visual Acuity Testing: Assessing vision clarity in order to detect central vision loss.
- Fundus Examination: Using an ophthalmoscope, examine the optic disc for signs of hyperemia (acute phase) or atrophy (chronic phase).
- Color Vision Testing: Assessing color discrimination, specifically red-green defects.
- Visual Field Testing: Automated perimetry maps visual field defects, which typically reveal central or cecocentral scotomas in people with LHON.
Genetic Testing
Genetic testing is required to confirm the diagnosis of LHON and determine the specific mitochondrial DNA mutation. Methods include:
- Mitochondrial DNA Sequencing: This test sequences the entire mitochondrial genome to detect known mutations associated with LHON, such as MT-ND1, MT-ND4, and MT-ND6. 2. Targeted Mutation Analysis: For individuals with a known family history of LHON, targeted testing for specific mutations can provide a fast and accurate diagnosis.
Advanced Imaging Techniques
Advanced imaging technologies provide detailed views of the optic nerve and retinal structures, which aid in the diagnosis of LHON.
- Optical Coherence Tomography (OCT): OCT produces high-resolution cross-sectional images of the retina, allowing for the detection of retinal nerve fiber layer (RNFL) thinning and optic nerve head changes associated with LHON.
- Fundus Fluorescein Angiography (FFA): FFA can detect abnormalities in the optic disc and retinal vasculature, thereby providing additional diagnostic information.
Electrophysiological tests
Electrophysiological testing evaluates the functional integrity of the optic nerve and visual pathways.
- Visual Evoked Potentials (VEP): VEP measures the electrical response of the brain to visual stimuli, which is typically impaired in LHON due to impaired optic nerve function.
- Electroretinography (ERG): ERG can help rule out other retinal disorders by measuring the retina’s electrical responses.
Differential Diagnosis
Given the overlap in symptoms with other optic neuropathies, it is important to distinguish LHON from conditions such as:
- Optic Neuritis: Optic neuritis is characterized by pain with eye movement and is frequently associated with multiple sclerosis. It can mimic the acute presentation of LHON.
- Dominant Optic Atrophy: A hereditary condition characterized by progressive vision loss and optic atrophy, but with a later onset and a distinct genetic basis.
- Toxic or Nutritional Optic Neuropathy: Toxins such as methanol, as well as nutritional deficiencies (for example, vitamin B12 deficiency), can cause optic neuropathy with LHON-like clinical features.
Leber’s Hereditary Optic Neuropathy Treatment
Treatment for Leber’s hereditary optic neuropathy (LHON) focuses on symptom management, slowing the progression of vision loss, and investigating potential restorative therapies. Although there is no cure for LHON, there are several approaches that can help reduce its effects.
Pharmacologic Treatments
- Idebenone: Idebenone, an antioxidant, has shown promise in clinical trials for LHON. It is thought to enhance mitochondrial function and reduce oxidative stress in retinal ganglion cells. According to studies, idebenone can help some patients achieve partial vision recovery, especially if treated early in the disease course.
- EPI-743: Another antioxidant, EPI-743, is being studied for its ability to treat mitochondrial diseases, including LHON. Early clinical trials indicate that it may improve visual function by increasing cellular energy production and reducing oxidative damage.
Nutritional Supplements
Nutritional support can help manage LHON. Supplements containing vitamins B1, B2, B12, folic acid, and coenzyme Q10 may aid in mitochondrial function. While not a cure, these supplements can help to support the body’s overall metabolic health.
Genetic Therapy
Gene therapy is a new treatment approach for LHON that aims to target the underlying genetic mutations that cause the disease. Clinical trials are looking into the effectiveness of introducing functional copies of mutated genes into retinal cells to restore normal mitochondrial function. One notable example is GS010 (Lenadogene nolparvovec), a gene therapy that targets the ND4 mutation. Preliminary trial results indicate some improvement in visual acuity and contrast sensitivity.
Supportive Treatments
- Visual Aids: Low-vision aids such as magnifiers, specialized glasses, and electronic devices can help people with LHON make the most of their remaining vision.
- Orientation and Mobility Training: This training teaches patients how to navigate their environment safely and independently, often using tools such as white canes or guide dogs.
- Occupational Therapy: Occupational therapists can help people with LHON adjust their daily activities to accommodate vision loss, allowing them to maintain independence and quality of life.
Emerging Therapies
Research into LHON continues to explore new treatment avenues.
- Mitochondrial Replacement Therapy (MRT): This experimental approach involves replacing defective mitochondria with healthy ones from a donor, which may correct the mitochondrial dysfunction at the root of LHON.
- Optogenetics: This novel field entails genetically modifying retinal cells to become light-sensitive, potentially restoring some visual function by bypassing damaged photoreceptors.
- Stem Cell Therapy: Researchers are looking into the ability of stem cells to regenerate damaged retinal cells and restore vision. Although still in the experimental stage, this approach holds promise for future treatments.
Lifestyle Modifications
Modifying one’s lifestyle can also help manage LHON.
- Avoiding Smoking and Alcohol: Individuals with LHON should avoid smoking and excessive alcohol consumption, as both can exacerbate mitochondrial dysfunction.
- Regular Eye Examinations: Monitoring eye health on a regular basis can help detect changes early and adjust treatment plans accordingly.
Effective Ways to Improve and Prevent Leber’s Hereditary Optic Neuropathy
- Genetic Counseling: Families with a history of LHON should seek genetic counseling to understand their risk of passing the condition down to children and make informed reproductive decisions.
- Avoiding Tobacco and Alcohol: Both smoking and drinking have been linked to worsening mitochondrial dysfunction. Avoiding these substances can help reduce the likelihood of triggering or exacerbating LHON symptoms.
- Regular Monitoring: People with a family history of LHON should have regular eye exams to detect early signs of the disease. Early intervention can help manage symptoms and slow progression.
- Nutritional Support: A diet high in vitamins and antioxidants can benefit overall eye health. Nutritional supplements containing vitamins B1, B2, B12, folic acid, and coenzyme Q10 may aid in mitochondrial function.
- Avoiding Environmental Toxins: It is best to limit your exposure to environmental toxins and chemicals that can impair mitochondrial function.
- Stress Management: Stress management techniques such as meditation, yoga, or therapy can help maintain overall health and possibly reduce the impact of LHON.
- Healthy Lifestyle: Regular exercise, a balanced diet, and adequate sleep promote overall well-being and mitochondrial health.
- Education and Support: Staying informed about LHON and connecting with support groups and organizations can provide valuable resources and emotional support as you manage the condition.
- Early Intervention: For people who have known mitochondrial mutations, early treatment with idebenone or other emerging therapies can help improve outcomes.
Trusted Resources
Books
- “Inherited Neuropathies: A Handbook for Clinicians” by Mary M. Reilly
- “Mitochondrial Disorders: Biochemical and Molecular Basis of Disease” by Amy Goldstein and Sumit Parikh
- “Principles and Practice of Ophthalmology” by Daniel M. Albert and Frederick A. Jakobiec
Online Resources
- National Eye Institute (NEI) – nei.nih.gov
- LHON.org – lhon.org
- United Mitochondrial Disease Foundation (UMDF) – umdf.org
- Genetics Home Reference – LHON – ghr.nlm.nih.gov






