What is Compressive Optic Neuropathy?
Compressive optic neuropathy is a serious ocular condition in which external pressure causes damage to the optic nerve. This pressure can be caused by a variety of factors, including tumors, cysts, or vascular anomalies, which impair blood flow and result in nerve dysfunction. The optic nerve is responsible for transmitting visual information from the eye to the brain, and any damage to it can cause significant vision loss. To avoid permanent vision impairment, the underlying cause must be identified early on and managed appropriately. Understanding the causes, symptoms, and risk factors of compressive optic neuropathy is critical for successful treatment and vision preservation.
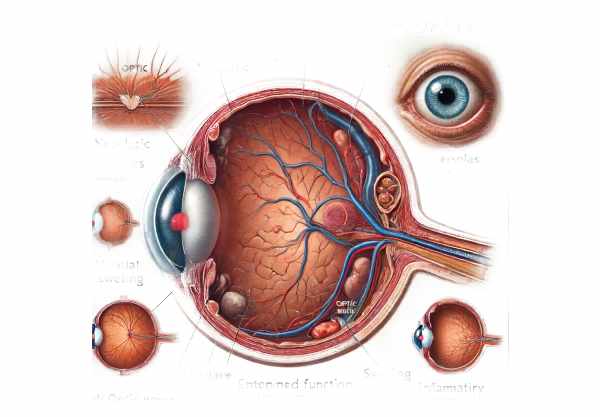
Compressive Optic Neuropathy Insights
Compressive optic neuropathy is caused by external pressure on the optic nerve, which results in impaired function and potential vision loss. The condition can have a variety of causes, including neoplastic, vascular, inflammatory, and traumatic. Each etiology presents unique challenges for diagnosis and management, necessitating a thorough understanding of the underlying mechanisms and clinical manifestations.
Etiology and Pathophysiology
The main causes of compressive optic neuropathy are:
- Neoplastic Causes: – Optic Nerve Glioma: A benign tumor formed by the optic nerve’s supporting glial cells. Common in children, these tumors can gradually compress the optic nerve.
- Meningioma: A tumor that develops from the meninges, the protective layers that surround the brain and optic nerve. Meningiomas can cause pressure on the optic nerve, resulting in progressive vision loss.
- Pituitary Adenoma: Pituitary gland tumors close to the optic chiasm can compress the optic nerve and optic chiasm, affecting both eyes.
- Vascular Causes: – Aneurysms: Abnormal dilation of blood vessels, especially the carotid artery, can compress the optic nerve.
- Carotid-Cavernous Fistula: An abnormal connection between the carotid artery and the cavernous sinus can cause increased pressure on the optic nerve.
- Inflammatory Causes: – Thyroid Eye Disease: An autoimmune condition linked to hyperthyroidism that causes inflammation and swelling in the eye muscles and tissues, potentially compressing the optic nerve.
Sarcoidosis is a systemic inflammatory disease that can cause granulomas to form in a variety of organs, including the optic nerve. - Traumatic Causes: – Orbital Fractures: Trauma to the orbit can cause bone fragments or swelling, compressing the optic nerve.
- Post-Surgical Changes: Surgical interventions around the optic nerve may cause scarring or swelling, resulting in compression.
Clinical Presentation
The clinical presentation of compressive optic neuropathy varies according to the underlying cause, degree of compression, and duration of the condition. Common symptoms include:
- Visual Field Defects: Patients often experience gradual loss of peripheral vision, resulting in a tunnel vision effect. Central vision may be preserved initially, but it can be compromised in advanced cases.
- Decreased Visual Acuity: Progressive compression of the optic nerve can reduce visual sharpness and clarity, affecting the ability to read and recognize faces.
- Color Vision Deficiency: – Affected individuals may experience a decrease in color perception, such as a washing out of colors, especially red and green.
- Ocular Pain: – Pain around the eye, especially during eye movements, can occur due to inflammatory causes such as thyroid eye disease.
- Proptosis: Proptosis, or forward displacement of the eye, is common in thyroid eye disease and other orbital tumors and indicates significant orbital involvement.
- Relative Afferent Pupillary Defect (RAPD): A relative afferent pupillary defect, also known as the Marcus Gunn pupil, is frequently observed, indicating asymmetric optic nerve function.
Risk Factors
Individuals are more likely to develop compressive optic neuropathy if they have certain risk factors.
- Genetic Predisposition: Neurofibromatosis type 1 and 2 increase the risk of developing optic nerve tumors, including gliomas and meningiomas.
- Autoimmune Disorders: Autoimmune conditions such as Graves’ disease increase the risk of developing thyroid eye disease, a leading cause of compressive optic neuropathy.
- Vascular Conditions: – Hypertension and other cardiovascular diseases can increase the risk of aneurysms and vascular anomalies that compress the optic nerve.
- Trauma: People with a history of orbital or head trauma are more likely to develop compressive optic neuropathy due to structural damage.
- Neoplastic Syndromes: Multiple endocrine neoplasia (MEN) may increase the risk of optic nerve tumors.
Complications
Untreated compressive optic neuropathy can cause serious complications:
- Permanent Vision Loss: Chronic compression can irreversibly damage optic nerve fibers, resulting in permanent blindness.
- Secondary Glaucoma: – Increased intraocular pressure from orbital masses can cause secondary glaucoma, compromising vision.
- Neurological Deficits: Extensive involvement of surrounding neural structures can result in additional neurological deficits, including cranial nerve palsies.
Prognosis
The prognosis for compressive optic neuropathy is determined by the underlying cause, the promptness of diagnosis, and the efficacy of treatment. Early detection and appropriate management are critical for maintaining vision and avoiding complications. In many cases, prompt intervention can result in significant restoration of visual function. However, the extent of recovery is also determined by the duration and severity of the compression prior to treatment.
Understanding compressive optic neuropathy necessitates a collaborative effort among ophthalmologists, neurologists, and other specialists to address the complex interplay of factors that contribute to optic nerve compression. Awareness of the condition, its risk factors, and potential complications is critical for early intervention and the best patient outcomes.
Prevention Tips
Preventing compressive optic neuropathy entails reducing risk factors and detecting conditions that may lead to optic nerve compression. Here are some important preventive measures and risk reduction tips:
- Schedule regular eye exams, particularly for those with risk factors like autoimmune disorders or a family history of neoplastic syndromes. Early detection of subtle changes can prevent serious complications.
- Effectively manage chronic conditions, such as hypertension and diabetes, which can lead to vascular anomalies and compressive optic neuropathy.
- Genetic Counseling: – Those with a family history of neurofibromatosis or multiple endocrine neoplasia should seek genetic counseling to assess their risk and implement proactive monitoring.
- Protective Eyewear: – Wear protective eyewear for activities that may cause orbital trauma, such as contact sports or hazardous work environments. Preventing trauma can lower the risk of compressive optic neuropathy.
- Early Intervention for Autoimmune Disorders: – Address autoimmune conditions such as Graves’ disease to avoid complications like thyroid eye disease, which can cause optic nerve compression.
- Monitor Symptoms: – Be alert for new symptoms like visual disturbances, ocular pain, or changes in color perception. Early medical consultation can result in timely diagnosis and treatment.
- Maintain a healthy lifestyle, including a balanced diet, regular exercise, and avoiding smoking, to reduce the risk of vascular conditions that can lead to compressive optic neuropathy.
- Regular Imaging for At-Risk Individuals: – Individuals with known risk factors should have regular imaging studies, such as MRI or CT scans, to monitor for tumors or vascular anomalies around the optic nerve.
- Awareness and Education: – Educate yourself and others on the risk factors and symptoms of compressive optic neuropathy. Awareness can result in earlier detection and better outcomes.
- Follow Medical Advice: – Follow medical advice and appointments, especially if you have underlying conditions that increase your risk of optic nerve compression. Regular monitoring and timely intervention are critical to avoiding serious complications.
Compressive Optic Neuropathy Diagnostic Techniques
Compressive optic neuropathy must be diagnosed using a comprehensive approach that includes clinical examination as well as advanced imaging techniques to determine the source and extent of optic nerve compression.
Clinical Examination
A comprehensive clinical examination by an ophthalmologist or neurologist is the first step in diagnosing compressive optic neuropathy. The key components of the clinical evaluation are:
- Visual Acuity Test: This test evaluates the patient’s vision clarity and can detect any decrease in visual acuity.
- Pupillary Response: Assessing the pupillary light reflex can aid in detecting a relative afferent pupillary defect (RAPD), which indicates asymmetric optic nerve function.
- Visual Field Testing: This test maps the patient’s field of vision and detects peripheral vision loss or central scotomas, which are signs of optic nerve damage.
Imaging Techniques
Advanced imaging techniques are critical for determining the cause of optic nerve compression and the extent of damage.
- Magnetic Resonance Imaging (MRI) is the gold standard for detecting compressive optic neuropathy. It generates detailed images of the optic nerve, optic chiasm, and surrounding structures, which aid in the detection of tumors, aneurysms, and inflammatory lesions.
- Computed Tomography (CT): CT scans can detect bony abnormalities like fractures or hyperostosis that could compress the optic nerve. They also help visualize calcified lesions more effectively than MRI.
- Orbital Ultrasound: Although less commonly used, this technique can be useful in detecting masses within the orbit, such as tumors or cysts, which may compress the optic nerve.
- Fundus Fluorescein Angiography (FFA): FFA examines the blood flow in the retina and optic nerve head to detect any vascular abnormalities that may contribute to optic nerve compression.
Electrophysiological Tests Electrophysiological tests evaluate the functioning of the optic nerve and can provide additional diagnostic information.
- Visual Evoked Potentials (VEP): VEP measures the brain’s electrical response to visual stimuli and can aid in detecting delayed conduction in the optic nerve due to compression.
- Electroretinography (ERG): ERG measures the electrical activity of the retina and can aid in distinguishing retinal from optic nerve causes of vision loss.
Biopsy and Histological Examination
When a neoplastic cause is suspected, a biopsy of the lesion may be performed to determine the compressive mass’s histopathology. This is especially important for guiding tumor treatment.
Compressive Optic Neuropathy Treatment Options
The treatment of compressive optic neuropathy focuses on relieving pressure on the optic nerve while also addressing the underlying cause to preserve or restore vision.
Medical Management
Medical treatment may be appropriate for inflammatory and neoplastic causes of optic nerve compression.
- Corticosteroids: Systemic corticosteroids are commonly used to reduce inflammation and edema in diseases such as thyroid eye disease and sarcoidosis.
- Radiotherapy: For some tumours, such as optic nerve gliomas or meningiomas, radiotherapy can shrink the tumour and relieve pressure on the optic nerve.
- Chemotherapy: In the case of malignant tumors, chemotherapy may be used in conjunction with other treatments to slow tumor growth.
Surgical Intervention
Surgical intervention is frequently required when the optic nerve is severely compressed or when medical treatment fails to improve the condition.
- Orbital Decompression Surgery: This procedure is commonly used in thyroid eye disease to relieve pressure on the optic nerve by removing a portion of the orbital bony structure or fat.
- Tumor Resection: Surgical removal of tumors, such as meningiomas or pituitary adenomas, can relieve compression and keep the optic nerve functioning. The surgical approach is determined by the size and location of the tumor.
- Endoscopic Endonasal Surgery: This minimally invasive technique is used to remove pituitary adenomas and other tumors located near the optic chiasm, lowering the risk of causing damage to nearby structures.
Innovative and Emerging Therapies
Emerging therapies for compressive optic neuropathy aim to improve outcomes and reduce complications.
- Gene Therapy: Researchers are working to correct genetic defects that cause tumor growth or optic nerve damage. While still in the experimental stage, this approach shows promise for treating hereditary conditions.
- Biologic Agents: New biologic agents that target specific inflammatory pathways are being developed to treat autoimmune causes of optic nerve compression, including thyroid eye disease.
- Neuroprotective Therapies: These therapies are intended to protect the optic nerve from further damage during the treatment of compressive lesions. Antioxidants and nerve regeneration-promoting drugs are examples of neuroprotective agents.
Trusted Resources
Books
- “Neuro-Ophthalmology Illustrated” by Valerie Biousse and Nancy J. Newman
- “Clinical Neuro-Ophthalmology” by Andrew G. Lee and Paul W. Brazis
- “Optic Nerve Disorders: Diagnosis and Management” by Jane W. Chan






