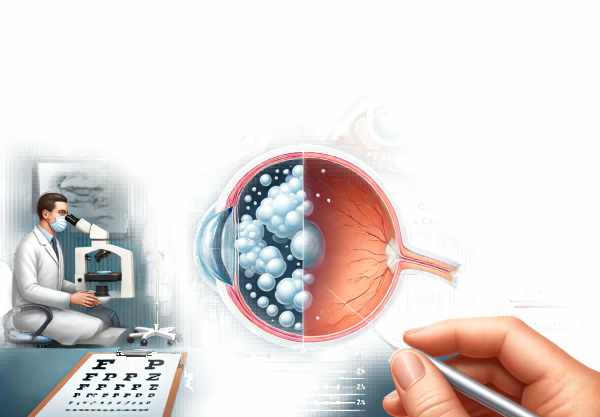
What is Congenital Cataract?
Congenital cataracts are cloudings of the eye’s lens that occur at birth or develop during infancy. This condition can range in severity, potentially resulting in significant vision impairment or blindness if not treated. Congenital cataracts can affect one or both eyes and are caused by genetics, intrauterine infections, metabolic disorders, or other developmental abnormalities. Early detection and intervention are critical for preventing long-term visual deficits and promoting proper visual development in affected infants. Understanding the causes, manifestations, and implications of congenital cataracts is critical for effective management and better results.
Congenital Cataract Insights
Congenital cataract is defined as an opacity of the eye’s lens that occurs at birth or develops shortly thereafter. The lens, which is normally clear and responsible for focusing light on the retina, becomes clouded, resulting in blurred vision or vision loss. This condition is a leading cause of childhood blindness and visual impairment globally, necessitating prompt diagnosis and treatment.
Etiology and Pathophysiology
Congenital cataracts can be caused by a variety of factors.
- Genetic Factors:
- Hereditary Cataracts: Congenital cataracts are most commonly inherited in an autosomal dominant pattern. Mutations in genes like CRYAA, CRYBB2, and CRYGC, which encode crystallin proteins required for lens transparency, are frequently implicated.
- Chromosomal Abnormalities: Down syndrome (trisomy 21) and other chromosomal abnormalities can increase the risk of developing congenital cataracts.
- Intrauterine Infection:
- TORCH Infections: Toxoplasmosis, rubella, cytomegalovirus (CMV), and herpes simplex virus (HSV) are major intrauterine infections linked to congenital cataracts. Rubella, in particular, has a strong association with cataract formation during the first trimester of pregnancy.
- Metabolic Disorder:
- Galactosemia: A metabolic disorder characterized by an inability to metabolize galactose, which can result in cataract formation due to galactitol accumulation in the lens.
- Hypoglycemia: Severe and prolonged hypoglycemia in newborns can also cause cataracts.
- Environmental factors:
- Radiation Exposure: Ionizing radiation during pregnancy can disrupt normal lens development and lead to cataracts.
- Maternal Malnutrition: Lack of essential nutrients during pregnancy can impair fetal eye development.
Clinical Presentation
The clinical presentation of congenital cataracts varies depending on the location, size, and density of the lens opacity. Key clinical characteristics include:
- Leukocoria:
- A white or grayish reflection from the pupil, known as the “cat’s eye reflex,” is a defining feature of congenital cataract. This abnormal reflex can be detected during routine neonatal examinations or by parents.
- Nystagmus:
- Infants with significant visual impairment from congenital cataracts may develop involuntary, rhythmic eye movements.
- Strabismus:
- Misalignment of the eyes, also known as “crossed eyes,” can occur when visual input is unequal due to cataract-induced vision loss.
- Poor visual tracking:
- Infants born with congenital cataracts may have difficulty following objects with their eyes, indicating poor visual development.
- Delayed Visual Development:
- Infants with untreated congenital cataracts frequently fail to meet visual milestones such as recognizing faces and objects.
Impact on Visual Development
Early visual experiences are critical to the development of visual pathways in the brain. If left untreated, congenital cataracts can cause amblyopia, also known as “lazy eye.” This condition occurs when the brain favors input from the unaffected eye, resulting in underdevelopment of the visual cortex associated with the cataract-affected eye. The critical period for visual development lasts from birth to around seven years of age, with the first few months being especially important. To avoid permanent visual impairment, congenital cataracts must be detected and treated early.
Epidemiology
Congenital cataracts are the most common cause of treatable childhood blindness. The prevalence varies across the globe, with higher rates in low- and middle-income countries due to limited access to healthcare and prenatal services. In developed countries, the incidence is estimated to be 1–6 cases per 10,000 live births. The condition can occur alone or as part of a syndrome that includes other systemic abnormalities.
Genetic Counseling and Testing
Given the significant genetic component in congenital cataracts, affected families should seek genetic counseling. Identifying the specific genetic mutation can shed light on the mode of inheritance and recurrence risk in future pregnancies. Genetic testing, such as next-generation sequencing (NGS) panels that target cataract-related genes, can help identify the underlying genetic cause.
Risk Factors
Several risk factors increase the likelihood of developing a congenital cataract.
- Family history:
- Offspring are more likely to develop congenital cataracts or other hereditary eye conditions if their parents have a history of them.
- Maternal Infection:
- Pregnancy infections, especially in the first trimester, are a significant risk factor for congenital cataracts.
- Metabolic Conditions*:
- Infants born to mothers with uncontrolled metabolic disorders, such as diabetes, have a higher risk of congenital cataracts.
- Chromosomal abnormalities:
Congenital cataracts are frequently associated with genetic syndromes characterized by chromosomal abnormalities.
Complications
Untreated congenital cataracts can cause a variety of complications:
- Amblyopia:
- As previously stated, amblyopia can result from the brain’s preference for the unaffected eye, leading to permanent vision impairment if not treated promptly.
- Glaucoma:
- Secondary glaucoma can develop as a result of increased intraocular pressure caused by lens anomalies or surgical procedures.
- ** Retinal Detachment**:
- Eyes with structural abnormalities caused by congenital cataracts or after cataract surgery are more likely to develop retinal detachment.
- Visual impairment:
- Persistent visual impairment can have an impact on the child’s overall development, such as motor skills, social interactions, and academic performance.
Prognosis
The prognosis for infants with congenital cataracts is determined by several factors, including the time of diagnosis, the severity of the cataract, and the promptness of treatment. Early surgical intervention, preferably within the first few months of life, can greatly improve visual outcomes. Regular follow-up and visual rehabilitation are critical components of post-treatment care to ensure optimal visual development and avoid complications.
Congenital Cataract Prevention Tips
Congenital cataracts can be prevented by addressing modifiable risk factors and ensuring adequate prenatal care. Here are some important preventive measures and risk reduction tips:
- Prenatal Care*:
- Regular prenatal check-ups are essential for monitoring the health of both the mother and the developing fetus. Early detection of maternal infections or other risk factors allows for timely intervention.
- Vaccination:
- Make sure women of childbearing age are immunized against rubella and other infections that can cause congenital cataracts. Rubella vaccination before pregnancy is especially important.
- Genetic counseling:
- Couples with a family history of congenital cataracts or genetic syndromes should seek genetic counseling before beginning a pregnancy to better understand the risks and options.
- Good Nutrition:
- Eating a balanced diet rich in essential nutrients during pregnancy promotes overall fetal development and lowers the risk of congenital anomalies, such as cataracts.
- Avoiding Teratogens:
- Pregnant women should avoid known teratogens, such as alcohol, tobacco, and certain medications, which can harm fetal development.
- Manage Chronic Conditions:
- Women with chronic conditions, such as diabetes, should work with their healthcare providers to effectively manage their condition before and during pregnancy in order to reduce the risk of complications.
- Preventing Infection:
- Practicing good hygiene and avoiding contact with people who have infectious diseases can help prevent maternal infections that may harm the fetus.
- Regular screenings:
- Infants born to mothers with risk factors should have early and regular eye screenings to detect and treat congenital cataracts.
- Educating Parents:
- Educating parents on the symptoms of congenital cataracts and the importance of early intervention can result in timely medical consultation and treatment.
- Newborn Screening Programs:
- Encourage and participate in newborn screening programs that include eye exams to detect and treat congenital cataracts and other eye conditions early.
Diagnostic methods
Congenital cataracts are diagnosed through a combination of clinical examination and advanced diagnostic techniques to determine the extent and severity of the lens opacity. Early detection is critical for timely intervention and best visual results.
Clinical Examination
- Visual Inspection: During the initial assessment, look for visible signs like leukocoria, which causes the pupil to appear white or gray. This can be accomplished during routine neonatal examinations or through parental observation.
- Pupillary Reflex Test: The red reflex test is a simple but effective screening tool for routine pediatric check-ups. Absence or abnormality of the red reflex may indicate the presence of a cataract.
- Slit-Lamp Examination: A thorough slit-lamp examination allows ophthalmologists to examine the anterior segment of the eye, providing a magnified view of the lens and determining the type, size, and location of the cataract.
Imaging Techniques
- Ocular Ultrasound: When a fundus examination is not possible due to dense cataracts, ocular ultrasound can help visualize the internal structures of the eye, including the retina and optic nerve, to rule out other abnormalities.
- Optical Coherence Tomography (OCT): OCT can produce high-resolution cross-sectional images of the retina and optic nerve. This is especially useful for determining the structural integrity of the retina and detecting associated conditions.
Genetic Testing
- Molecular Genetic Testing: Because many congenital cataracts are hereditary, genetic testing can pinpoint the exact mutations that cause the condition. Next-generation sequencing (NGS) is a technique that can analyze multiple genes at the same time, providing a complete genetic profile.
- Chromosomal Analysis: In cases with syndromic presentations or chromosomal abnormalities, karyotyping or chromosomal microarray analysis may be used to detect large genetic changes.
Electrophysiological tests
- Electroretinography (ERG): ERG detects the electrical responses of different cell types in the retina. It aids in determining the functional state of the retina and distinguishing between retinal and optic nerve dysfunctions.
- Visual Evoked Potentials (VEP): VEP measures the electrical activity of the visual cortex in response to visual stimuli, revealing information about the entire visual pathway from the retina to the brain.
Comprehensive Eye Exam
- Fundus Examination: Following cataract removal, a thorough fundus examination is performed to ensure the retina and optic nerve are normal.
- Refraction Test: Assessing refractive errors following surgery is critical to determining the need for corrective lenses to aid in visual rehabilitation.
Congenital Cataract Management
The goal of treating congenital cataracts is to restore visual function while preventing amblyopia. Early intervention is critical for optimal visual development in infants and young children.
Surgical Intervention
- Cataract Extraction: The primary treatment for severe congenital cataracts is surgical removal. The timing of surgery is critical; ideally, it should be done within the first few months of life to avoid visual loss and amblyopia. There are two primary types of cataract extraction:
- Lens Aspiration: This procedure removes the cataractous lens material while preserving the lens capsule and is appropriate for softer cataracts.
- Lensectomy: Complete removal of the lens and capsule, commonly used for denser cataracts or significant posterior capsule opacification.
- Intraocular Lens (IOL) Implantation: After cataract surgery, an artificial intraocular lens (IOL) can be implanted to restore focusing ability. Primary IOL implantation in infants is being debated due to ongoing eye growth and development. Secondary IOL implantation may be considered as the child ages.
Post-surgical Management
- Aphakic Correction: In cases where IOL implantation is not performed, aphakic correction with contact lenses or glasses is required. Contact lenses are frequently preferred in infants due to their superior visual outcomes and ease of use.
- Patching Therapy: To avoid amblyopia, occlusion therapy (patching the stronger eye) is used to stimulate visual development in the affected eye.
- Refractive Correction: Frequent follow-ups and refractive assessments are essential. Providing appropriate corrective lenses ensures optimal visual development and prevents amblyopia.
Innovative and Emerging Therapies
- Gene Therapy: Research into gene therapy for genetic forms of congenital cataracts is currently underway. This approach seeks to correct the underlying cause at the molecular level by focusing on specific genetic mutations.
- Stem Cell Therapy: Stem cell therapy has the potential to regenerate the lens and restore its transparency. Early studies show promise, but more research is needed to determine its efficacy and safety in clinical practice.
- Pharmacological Interventions: Another research area is developing drugs to prevent or slow the progression of lens opacification. These therapies aim to keep the lens transparent and postpone the need for surgical intervention.
Visual Rehabilitation
- Early Intervention Programs: Enrolling children in visual rehabilitation programs after surgery can improve visual outcomes. These programs include activities that promote visual-motor coordination and cognitive development.
- Supportive Services: Giving families access to low vision aids, educational support, and counseling services helps them manage the long-term effects of congenital cataracts on their child’s development and quality of life.
Trusted Resources
Books
- “Pediatric Ophthalmology and Strabismus” by Kenneth W. Wright and Peter H. Spiegel
- “Congenital Cataract: A Concise Guide to Diagnosis and Management” by Roberto Pineda II and Susan Vitale
- “Principles and Practice of Pediatric Ophthalmology” by Daniel M. Albert and Edward M. Jakobiec






