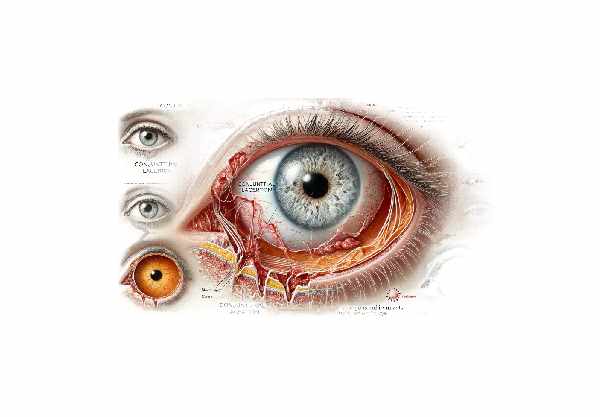
What is Conjunctival Laceration?
A conjunctival laceration is a tear or cut in the conjunctiva, a clear, thin membrane that protects the white part of the eye (sclera) and the inside of the eyelids. This condition can develop as a result of eye trauma, such as being struck by an object, falling, or being poked. Conjunctival lacerations are typically less severe than deeper eye injuries, but they can still cause significant discomfort, redness, and swelling. If not managed properly, they can cause infections and other complications. Understanding the nature of conjunctival lacerations, their causes, and associated risks is critical for effective prevention and treatment.
Conjunctival Laceration Insight
Conjunctival lacerations, while less common than other ocular injuries, require immediate treatment to avoid complications. The conjunctiva protects the eye, and any disruption can expose the underlying tissues to pathogens and irritants. To fully understand the impact of conjunctival lacerations, it is necessary to investigate their causes, symptoms, potential complications, and recovery process.
Causes of conjunctival lacerations
Several types of trauma can cause conjunctival lacerations, such as:
- Blunt Trauma: When an object, such as a ball, fist, or blunt instrument, strikes the eye, the conjunctiva tears. This type of injury frequently occurs in sports or accidents.
- Sharp Trauma: Sharp objects, such as fingernails, paper edges, or tools, can cause conjunctival injuries. These injuries are common in settings where sharp objects are frequently handled.
- Foreign Bodies: Particles like sand, metal shavings, or glass can get lodged in the eye and cause abrasions or lacerations as they move across the conjunctiva.
- Chemical Burns: Exposure to chemicals can cause tissue damage and tears. Acids, alkalis, and other corrosive substances can result in both chemical burns and physical lacerations.
Symptoms of Conjunctival Lacerations
The symptoms of a conjunctival laceration vary according to the severity and cause of the injury. Common symptoms include:
- Redness and Swelling: Inflammation causes the affected area to become red and swollen.
- Pain and Discomfort: Patients frequently report sharp pain or the sensation that something is in their eye.
- Tearing and Discharge: Irritation often causes increased tear production. Discharge may also occur if an infection develops.
- Visual Disturbances: If the laceration is near the cornea or if swelling interferes with vision, you may experience blurred vision or difficulty focusing.
- Bleeding: Small blood vessels in the conjunctiva can bleed, resulting in visible blood in the affected area.
Complications of Conjunctival Lacerations
While most conjunctival lacerations heal without any long-term consequences, complications can occur, especially if the injury is severe or not treated quickly. Possible complications include:
- Infection: Bacteria can enter the eye and infect the open wound, causing conjunctivitis or more serious infections such as keratitis.
- Scarring: Severe lacerations may result in scar formation, which can alter the appearance of the eye and, in some cases, impair vision.
- Deeper Eye Injuries: A conjunctival laceration can result in injuries to the eye’s deeper structures, such as the cornea, sclera, and intraocular tissues. These injuries can have more serious consequences and necessitate specialized care.
- Persistent Discomfort: Even after healing, some patients may experience chronic discomfort or a feeling of dryness if the injury disrupts the normal tear film distribution.
Healing Process for Conjunctival Lacerations
The conjunctiva is a highly vascular tissue with a strong ability to heal. The healing process typically consists of several stages:
- Inflammation: Immediately following an injury, the body launches an inflammatory response to clear debris and prevent infection. This phase is distinguished by redness, swelling, and pain.
- Proliferation: New cells grow to replace damaged tissue. Fibroblasts, which produce collagen and other extracellular matrix components, play an important role in this phase.
- Remodeling: The new tissue matures and strengthens while any excess tissue is removed. This phase can last several weeks, during which the eye gradually regains its normal appearance and function.
Factors that Affect Healing
Several factors can affect the healing of a conjunctival laceration:
- Severity of Injury: Larger and deeper lacerations take longer to heal and are more likely to cause complications.
- Location of the Laceration: Because of differences in tissue structure and blood supply, injuries near the limbus (the border between the cornea and sclera) or involving the fornices (the folds between the eyelid and eyeball) heal differently.
- Patient Health: Diabetes, immune deficiencies, and pre-existing eye diseases can all slow healing. Nutritional status and overall health both play a role.
- Treatment Received: Prompt and appropriate treatment, such as cleaning the wound, removing foreign bodies, and administering medications like antibiotics, can significantly improve healing outcomes.
Psychological Impact
Ocular injuries, such as conjunctival lacerations, can have a psychological impact on patients, especially if the injury is traumatic or causes visible changes to the eye. Patients may feel anxious, fearful of losing their vision, or concerned about their appearance. Providing emotional support and reassurance is an important part of patient care.
Prevention Tips
- Wear Protective Eyewear: Always wear appropriate protective eyewear when participating in activities that could result in eye injury, such as sports, woodworking, or using power tools.
- Handle Sharp Objects Carefully: Exercise caution when using or around sharp objects such as scissors, knives, and tools. Keep these items safely out of reach of children.
- Avoid Rubbing Eyes: Teach children and adults not to rub their eyes, especially if they feel something in them. Rubbing can worsen minor injuries and spread pathogens.
- Keep Hazardous Substances Secure: To avoid accidental exposure, store chemicals, cleaning agents, and other hazardous substances in secure, child-proof containers.
- Supervise Children’s Play: Keep an eye on children during playtime to ensure they do not engage in activities that could cause eye injuries, such as playing with sticks or sharp toys.
- Be Cautious with Contact Lenses: Use proper hygiene and handling procedures for contact lenses to avoid scratches or infections that could result in lacerations.
- First Aid Awareness: Understand basic first aid for eye injuries, such as how to flush foreign bodies and when to seek medical attention.
- Regular Eye Check-Ups: Schedule regular eye exams to detect and address any problems early on, ensuring overall eye health and protection.
Diagnostic methods
An eye care professional performs a thorough ocular examination to diagnose conjunctival lacerations. This assessment ensures that the extent of the injury is accurately determined and that no other ocular structures are affected.
Clinical Examination
The diagnostic process begins with a thorough patient history to determine the cause of injury and any symptoms present. A visual acuity test is typically used to determine whether the injury has affected vision.
Slit Lamp Examination
A slit-lamp examination is a common diagnostic tool used to examine the eye at high magnification. This device offers a detailed view of the conjunctiva and surrounding structures. Fluorescein dye can be applied to the eye to highlight the laceration and detect corneal abrasions or foreign bodies.
Eversion of the eyelids
To ensure that no foreign bodies are concealed beneath the eyelids, the examiner may gently evert them. This method is critical for detecting particles that could cause additional damage or infection if left untreated.
Intraocular Pressure Measurement
Intraocular pressure (IOP) is measured to rule out any possible complications, such as globe rupture, which can significantly raise IOP. Elevated IOP may indicate more severe underlying damage.
Imaging Studies
When the injury is severe or additional intraocular damage is suspected, imaging studies such as ultrasound biomicroscopy (UBM) or optical coherence tomography (OCT) can be used. These modalities produce detailed images of the anterior segment of the eye, allowing for the examination of deeper structures.
Innovative Diagnostic Techniques
Recent advances in ocular diagnostics have introduced techniques like confocal microscopy, which allows for high-resolution imaging of conjunctival tissue. Furthermore, advanced OCT systems can produce cross-sectional images with unprecedented detail, which aids in the assessment of complex injuries.
Microbiological Testing
If an infection is suspected, swabs from the conjunctival surface may be collected for microbiological testing. This aids in the detection of bacteria, fungi, or other pathogens, as well as the selection of appropriate antimicrobial therapy.
These diagnostic methods allow for a thorough evaluation of conjunctival lacerations, resulting in an accurate diagnosis and appropriate treatment planning.
How to Treat Conjunctival Laceration
Treatment for conjunctival lacerations aims to promote healing, prevent infection, and address any complications that may arise. Treatment options vary depending on the severity of the laceration and the presence of any other ocular injuries.
Standard Treatment Options
- Cleaning the Wound: The initial treatment entails thoroughly cleaning the affected eye to remove any debris or foreign bodies. This step is critical for preventing infection and promoting healing.
- Antibiotic Ointments and Drops: Topical antibiotics are frequently used to prevent bacterial infections. Ointments such as erythromycin or bacitracin are commonly used, with several applications per day as directed by the healthcare provider.
- Patching the Eye: In some cases, an eye patch may be used to protect the injured eye, relieve discomfort, and promote healing. The patch is usually worn for one to two days, depending on the severity of the laceration.
- Pain Management: Over-the-counter pain relievers such as acetaminophen or ibuprofen can help alleviate discomfort. Lubricating eye drops can also be used to reduce irritation and dryness.
- Follow-Up Examinations: Regular follow-up visits are required to monitor the healing process and prevent complications, such as infections or scarring.
Surgical Interventions
More severe lacerations that involve deeper layers of the conjunctiva or are associated with other ocular injuries may necessitate surgical intervention.
- Suturing: Suturing may be required for large or gaping lacerations to ensure proper alignment and tissue healing. Absorbable sutures are frequently used because they dissolve over time and do not require removal.
- Foreign Body Removal: If the laceration was caused by a foreign object lodged in the eye, surgical removal may be required to prevent further damage or infection.
- Repair of Associated Injuries: If the laceration is part of a larger ocular injury affecting the sclera or cornea, additional surgical procedures may be required to repair these structures and restore eye integrity.
Innovative and Emerging Therapies
Advances in ocular surgery and wound care have resulted in novel treatments for conjunctival lacerations.
- Amniotic Membrane Transplantation: Amniotic membranes, which have anti-inflammatory and healing properties, can be used to cover the laceration, promoting faster and more complete healing and lowering the risk of scarring.
- Bioengineered Tissues: Research into bioengineered conjunctival tissues shows promise for more effective repair of severe injuries. These tissues have the ability to provide structural support while also enhancing the natural healing process.
- Growth Factor Therapy: Growth factors can be applied topically or injected to promote tissue repair and regeneration, potentially improving the outcome of severe lacerations.
Healthcare providers can effectively manage conjunctival lacerations by using both standard and innovative treatment methods, ensuring optimal healing and reducing the risk of complications.
Trusted Resources
Books
- “Chern’s Handbook of Ophthalmology” by Kelly M. Moffat, Michael P. Kelly, and Andrew P. Schachat
- “Ocular Trauma: Principles and Practice” by Ferenc Kuhn and Dante J. Pieramici










