Conjunctival squamous cell carcinoma (SCC) is the most common malignancy of the conjunctiva, presenting unique challenges for both patients and clinicians. This tumor typically arises on the surface of the eye and can invade surrounding tissues if left untreated, potentially threatening vision and, in rare cases, life. Prompt diagnosis, evidence-based treatment, and vigilant follow-up are crucial for optimal outcomes. In this comprehensive guide, we will explore the epidemiology, causes, traditional and modern therapies, surgical options, cutting-edge research, and practical insights to empower you or your loved ones facing this diagnosis.
Table of Contents
- Condition Overview and Epidemiology
- Conventional and Pharmacological Therapies
- Surgical and Interventional Procedures
- Emerging Innovations and Advanced Technologies
- Clinical Trials and Future Directions
- Frequently Asked Questions
- Disclaimer
Condition Overview and Epidemiology
Conjunctival squamous cell carcinoma (SCC) is a malignant tumor originating from the epithelial cells that line the conjunctiva. While the condition is relatively rare in temperate regions, its incidence is increasing globally, particularly in areas with high ultraviolet (UV) exposure.
Definition and Pathophysiology:
- Conjunctival SCC develops from abnormal proliferation of squamous epithelial cells.
- It typically presents as a gelatinous, leukoplakic (white), or nodular lesion, sometimes with feeder blood vessels or surface keratin.
- Tumor cells can invade deeper tissues, including the cornea, sclera, and, in advanced cases, the orbit.
Epidemiology:
- The global incidence varies, with higher rates in equatorial Africa, the Middle East, and regions with intense sunlight.
- Affects adults, particularly males, with the highest prevalence between ages 50 and 70.
- Risk factors include:
- Prolonged UV light exposure
- Immunosuppression (HIV/AIDS, organ transplantation)
- Human papillomavirus (HPV) infection (especially types 16 and 18)
- Chronic inflammation or scarring of the ocular surface
- Exposure to petroleum products or chemicals
Presentation:
- Painless, slowly enlarging conjunctival mass
- Redness, foreign body sensation, irritation, or visual changes (if the tumor invades the cornea)
- Lesions may be non-pigmented or display keratinization
Diagnosis:
- Slit-lamp examination, high-resolution anterior segment imaging, and photographic documentation
- Definitive diagnosis by incisional or excisional biopsy with histopathological analysis
- Staging may involve orbital imaging (ultrasound, CT, MRI) and regional lymph node evaluation for advanced cases
Practical Advice:
If you notice a new or persistent growth, irritation, or unexplained redness on your eye, seek an evaluation by an ophthalmologist. Early detection is the best way to preserve vision and prevent complications.
Conventional and Pharmacological Therapies
While surgery is central to SCC management, non-surgical and pharmacological therapies are crucial for both primary treatment (especially for smaller or in-situ lesions) and for reducing recurrence risk after surgery.
Topical Chemotherapeutic Agents:
- Mitomycin C (MMC):
- The most widely used topical agent, applied as 0.02–0.04% eye drops in cycles (usually 7–14 days per cycle, repeated with drug-free intervals).
- Effective for treating intraepithelial neoplasia (CIN) and residual microscopic disease post-surgery.
- 5-Fluorouracil (5-FU):
- An alternative to MMC, typically used at 1% concentration for 1-week courses with rest periods.
- Well-tolerated and particularly useful in cases with mild to moderate disease.
- Interferon alpha-2b:
- Can be administered as topical drops or local injections.
- Particularly useful in patients with surface disease, intolerance to other agents, or as adjunctive therapy in recurrent cases.
Adjunctive Measures:
- Cryotherapy:
- Application of freezing temperatures to surgical margins after tumor excision to kill any remaining abnormal cells and reduce recurrence risk.
- Lubrication and Supportive Care:
- Artificial tears and lubricating ointments soothe irritation from both the tumor and topical therapies.
- Anti-inflammatory Drops:
- Briefly used to manage inflammation associated with chemotherapeutic agents (always under medical supervision).
Symptom Control and Monitoring:
- Regular follow-up with slit-lamp exams is crucial for early detection of recurrence.
- Use sun protection (UV-blocking sunglasses, hats) and maintain good ocular hygiene.
Practical Advice:
Apply topical medications exactly as prescribed, never skipping or doubling doses. Wash hands before each application and monitor for side effects, such as pain, redness, or vision changes. Report any new or worsening symptoms to your provider.
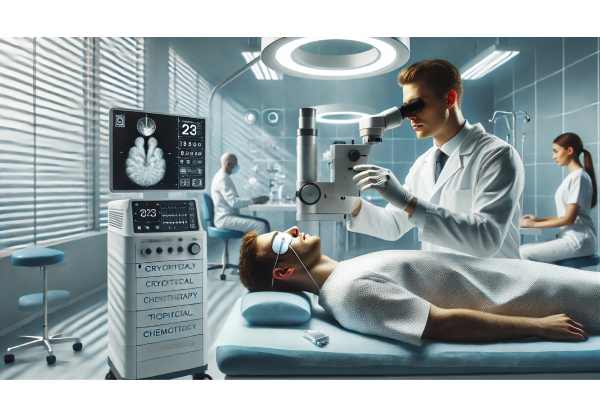
Surgical and Interventional Procedures
Surgical intervention remains the gold standard for conjunctival SCC, especially for invasive or extensive lesions. The goals are complete tumor removal, minimal recurrence, and maximal preservation of ocular structure and function.
Surgical Techniques:
- Excisional Biopsy (“No Touch” Technique):
- Wide local excision with 2–4 mm margins of healthy tissue to ensure complete removal
- Careful handling to avoid tumor seeding
- Alcohol Epitheliectomy:
- Absolute alcohol may be applied to the surface to facilitate removal of abnormal epithelial cells
- Adjuvant Cryotherapy:
- Freezing is applied to the wound edges and bed to destroy residual tumor cells
Reconstructive Procedures:
- Amniotic Membrane Transplantation:
- Used to repair large defects and promote healing with reduced scarring
- Conjunctival Autografting:
- Transplantation of the patient’s own conjunctiva to cover defects and restore a healthy ocular surface
Advanced Surgical Options:
- Sentinel Lymph Node Biopsy:
- Considered for high-risk or invasive cases to assess regional spread
- Orbital Exenteration:
- Reserved for rare, extensive tumors with deep invasion; involves removal of the eye and surrounding tissues to control life-threatening disease
Postoperative Care:
- Topical antibiotics and anti-inflammatories
- Frequent follow-ups for early detection of recurrence
- Patient education on signs of complications
Potential Complications:
- Recurrence (highest within the first two years)
- Scarring, symblepharon (adhesion between the eyelid and eyeball), dry eye, or reduced vision
- Secondary infections or delayed healing
Practical Advice:
Follow your postoperative care plan closely. Attend all scheduled checkups, and immediately report any signs of infection, increased pain, or changes in your eye’s appearance.
Emerging Innovations and Advanced Technologies
In recent years, several innovations have improved the detection, management, and prognosis of conjunctival SCC.
Molecular and Targeted Therapies:
- Genetic and Biomarker Analysis:
- Tumor profiling for markers such as HPV subtype can help guide therapy and risk assessment.
- Immune Modulating Agents:
- Research is ongoing into new topical and systemic immunotherapies for refractory or metastatic disease.
Advances in Surgical Technology:
- Microincision and Sutureless Surgery:
- Smaller, less traumatic procedures for faster recovery and less scarring.
- Laser-Assisted Excision:
- Use of excimer or CO2 lasers to precisely remove tumor tissue with minimal damage to healthy areas.
Artificial Intelligence (AI) and Imaging:
- AI-Assisted Diagnosis:
- Digital image analysis and machine learning tools help distinguish benign from malignant lesions and predict recurrence risk.
- Teleophthalmology:
- Remote monitoring and specialist consultations improve access to care and postoperative surveillance.
Personalized Medicine:
- Liquid Biopsies:
- Experimental blood tests for circulating tumor DNA (ctDNA) are being developed to detect early recurrence or metastasis.
Patient Empowerment:
- Mobile health apps and digital platforms are increasingly used for medication reminders, symptom tracking, and direct communication with care teams.
Practical Advice:
Ask your doctor about the availability of newer diagnostic tools or innovative therapies, especially if your case is complex or if you experience recurrence.
Clinical Trials and Future Directions
Ongoing research and clinical trials are essential to advancing care for conjunctival SCC and improving patient outcomes.
Current Research Areas:
- Novel Topical and Systemic Agents:
- Studies of new drugs with fewer side effects or improved efficacy for resistant cases
- Advanced Imaging and Biomarkers:
- Research on imaging techniques (OCT, confocal microscopy) and molecular markers for earlier detection and precise monitoring
- Combination Therapies:
- Evaluating combinations of chemotherapy, immunotherapy, and surgery to minimize recurrence
- AI and Remote Monitoring:
- Trials of digital and AI-based platforms for remote disease tracking and patient engagement
Patient Participation:
- Clinical trials may offer access to the latest therapies and expert care, especially for those with aggressive or recurrent disease.
- Many academic centers are actively recruiting patients for research studies.
Future Outlook:
- Personalized medicine and AI-driven diagnostics are expected to play increasing roles.
- Improved access to care and awareness may help reduce late diagnoses and enhance survival rates.
Practical Advice:
If you or a loved one is diagnosed with conjunctival SCC, inquire about clinical trial opportunities. Participation can provide access to innovative treatments and contribute to the advancement of care for all patients.
Frequently Asked Questions
What is conjunctival squamous cell carcinoma and how is it diagnosed?
Conjunctival squamous cell carcinoma is a cancer of the eye’s surface cells. Diagnosis involves an eye exam, imaging, and biopsy to confirm malignancy and assess the tumor’s extent.
What are the treatment options for conjunctival SCC?
Treatments include surgical excision, topical chemotherapy, cryotherapy, and, in advanced cases, immunotherapy or radiation. Treatment choice depends on tumor size, location, and depth.
Is conjunctival squamous cell carcinoma life-threatening?
Most cases are treatable and not life-threatening if detected early, but advanced tumors can invade deeper tissues or spread, making early intervention crucial.
Can conjunctival SCC recur after treatment?
Yes, recurrence is possible. Regular follow-up exams and prompt attention to any new symptoms are essential for early detection and management of recurrence.
Are there new therapies for advanced conjunctival SCC?
Recent advances include novel immunotherapies, targeted drugs, and AI-based diagnostics, many available through clinical trials at specialized centers.
Should I consider a clinical trial for conjunctival SCC?
Clinical trials offer access to cutting-edge treatments and intensive care. If you have recurrent or aggressive SCC, discuss available trials with your ophthalmologist or oncologist.
Disclaimer
The information provided in this guide is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a qualified healthcare provider for personalized diagnosis and treatment recommendations.
If you found this article useful, please share it on Facebook, X (formerly Twitter), or your preferred platform. Follow us on social media for more trustworthy, patient-focused insights, and help our team continue producing high-quality content by spreading the word!






