Introduction to Corneal Graft Rejection
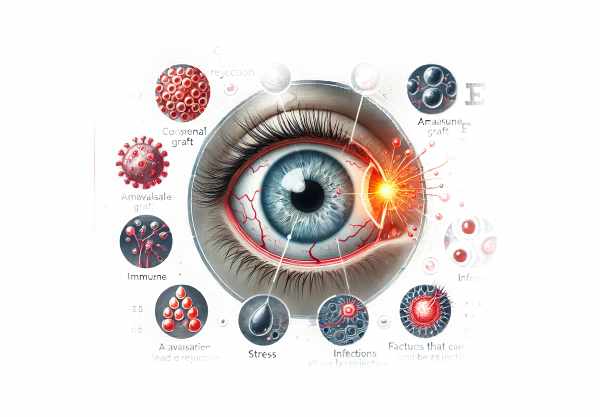
Corneal graft rejection is a serious complication that can develop following a corneal transplant, also known as keratoplasty. This condition occurs when the recipient’s immune system recognizes the transplanted corneal tissue as foreign and launches an immune response against it. Although corneal transplants have a high success rate, graft rejection is still a significant risk that can lead to graft failure if not addressed promptly and effectively. Understanding the mechanisms, risk factors, and symptoms of corneal graft rejection is critical for patients and healthcare providers seeking early detection and intervention.
Comprehensive Information on Corneal Graft Rejection
Corneal graft rejection is a complex process in which the recipient’s immune system attacks the donor cornea. The cornea is an avascular tissue, which means it lacks blood vessels, lowering the risk of an immune response. However, several factors can undermine this immune privilege, resulting in rejection.
Mechanisms for Rejection
T cells are the primary mediators of the immune response in corneal graft rejection, which involves both direct and indirect pathways.
- Direct Pathway: Donor-derived antigen-presenting cells (APCs) deliver donor antigens to the recipient’s T cells. This can occur when donor APCs migrate to the recipient’s lymph nodes and activate T cells directly.
- Indirect Pathway: Recipient APCs process donor antigens before presenting them to the recipient’s T cells. This pathway is more common in corneal graft rejection, which occurs when the recipient’s immune system recognizes the transplanted tissue as foreign.
Types of Rejection
Corneal graft rejection is divided into three types based on the layers of the cornea involved:
- Epithelial Rejection is the least severe form, affecting only the cornea’s outermost layer. It frequently presents with superficial punctate keratitis, which causes small, dot-like opacities on the corneal surface.
- Stromal Rejection: This condition affects the middle layer of the cornea and is distinguished by stromal haze, which can result in significant visual impairment. Inflammatory cells infiltrate the stroma, causing cloudiness and edema.
- Endothelial Rejection: Endothelial rejection is the most severe form, affecting the cornea’s innermost layer. It is characterized by the presence of keratic precipitates (KP) on the endothelium, endothelial cell loss, and corneal edema. This type can quickly lead to graft failure if not treated promptly.
Risk Factors
Several factors contribute to the risk of corneal graft rejection:
- Previous Rejections: A history of graft rejection raises the possibility of further rejections in the same eye.
- Vascularization: Increased blood vessel growth into the cornea (neovascularization) can improve immune cell access to the graft, raising the risk of rejection.
- Infections: Pre-existing or post-operative infections can activate an immune response, resulting in graft rejection.
- Glaucoma: Patients with glaucoma, especially those who have had glaucoma surgery, are at a higher risk due to changes in intraocular pressure and immune responses.
- Suture-related Issues: Problems with the sutures used to secure the graft can cause inflammation and immune activation.
- Donor and Recipient Age: Higher rejection rates have been observed for younger recipients and older donor tissues.
Symptoms:
The symptoms of corneal graft rejection can vary depending on the type and severity, but they typically include:
- Redness: Increased redness in the eye is a common early sign of rejection, resulting from inflammation and increased blood flow.
- Pain: Patients may feel discomfort or pain in their affected eye, which can range from mild to severe.
- Photophobia: Sensitivity to light is a common symptom, making patients uncomfortable in bright environments.
- Decreased Vision: Progressive vision loss or blurring is a strong indicator of graft rejection, particularly in cases involving the stromal or endothelial layers.
- Tearing: Excessive tearing can result from irritation and inflammation.
- Swelling: Corneal edema, or swelling, is a sign of endothelial rejection and can cause a significant increase in corneal thickness.
Pathophysiology
The underlying pathophysiology of corneal graft rejection is a complex interaction between the immune system and transplanted tissue. The immune response begins when the recipient’s immune system recognizes the donor antigens as foreign, activating T cells and producing inflammatory cytokines.
- Immune Activation: Antigen-presenting cells (APCs), such as dendritic cells, are critical for presenting donor antigens to the recipient’s T cells. This can happen through both direct and indirect pathways.
- Cytokine Release: Activated T cells produce cytokines, which are signaling molecules that increase inflammation and attract other immune cells to the graft site.
- Inflammatory Cell Infiltration: T cells, macrophages, and neutrophils infiltrate the corneal graft, resulting in tissue damage and edema.
- Endothelial Cell Damage: In endothelial rejection, the immune response specifically targets endothelial cells, resulting in cell death and loss of endothelial barrier function. This causes corneal edema and decreases transparency.
Clinical Course and Prognosis.
Corneal graft rejection can have either an acute or chronic clinical course.
- Acute Rejection: This form occurs quickly, usually within weeks to months of the transplant. It is distinguished by a sudden onset of symptoms and necessitates prompt treatment to avoid graft failure.
- Chronic Rejection: This type progresses slowly over months to years and is frequently accompanied by low-grade inflammation and gradual endothelial cell loss. Chronic rejection is more difficult to treat and can lead to progressive graft failure.
The prognosis for corneal graft rejection varies according to the timing of diagnosis and the efficacy of treatment. Early detection and intervention can improve outcomes and increase the chances of graft survival.
Prevention Tips
- Follow Post-Operative Care Instructions: Follow all post-operative care instructions given by your ophthalmologist, including taking prescribed medications and attending follow-up appointments.
- Use Immunosuppressive Medications: Take immunosuppressive medications as directed to reduce the risk of rejection. These medications help to regulate the immune response and keep the body from attacking the graft.
- Check for Symptoms: Look for any signs of graft rejection, such as redness, pain, photophobia, decreased vision, tearing, or swelling. Any changes should be reported to your healthcare provider immediately.
- Avoid Eye Rubbing: Avoid rubbing your eyes, which can cause irritation and increase your chances of rejection.
- Protect Your Eyes: Wear protective eyewear to keep your eyes safe from trauma, dust, and other environmental factors that can cause an immune response.
- Managing Underlying Conditions: Keep any underlying conditions, such as glaucoma or infections, under control. Proper management of these conditions can reduce the likelihood of complications leading to rejection.
- Regular Check-Ups: Keep all scheduled follow-up appointments with your ophthalmologist to monitor the graft’s health and identify any early signs of rejection.
- Avoid Contact with Infections: Stay away from people who have contagious infections, as systemic infections can raise the risk of graft rejection.
- Healthy Lifestyle: Maintain a healthy lifestyle, which includes a well-balanced diet and regular exercise, to help with immune health and recovery.
- Avoid Irritants: Limit your exposure to environmental irritants like smoke, pollutants, and chemicals, which can worsen inflammation and increase the risk of rejection.
Diagnostic methods
Diagnosing corneal graft rejection requires a patient history, clinical examination, and advanced diagnostic techniques to accurately assess the graft’s status and identify rejection signs. Here are the main diagnostic methods used:
- Slit Lamp Examination: The slit lamp is a valuable tool in ophthalmology because it provides a detailed view of the cornea. During a slit lamp examination, an ophthalmologist looks for inflammation, keratic precipitates (KP), stromal edema, and other signs of graft rejection. This examination provides a thorough assessment of the corneal layers and aids in the differentiation of types of rejection.
- Anterior Segment Optical Coherence Tomography (AS-OCT): AS-OCT is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the cornea. It aids in determining corneal thickness, detecting fluid accumulation, and assessing the structural integrity of the graft. AS-OCT is especially useful for tracking changes over time and identifying early signs of rejection.
- Specular Microscopy: This technique evaluates the cornea’s endothelial cell layer. Specular microscopy produces images of endothelial cells that can be used to assess cell density, size, and morphology. A decrease in endothelial cell density or abnormal cell morphology may indicate endothelial rejection.
- Fluorescein Angiography: In this imaging technique, a fluorescent dye is injected into the bloodstream and photographs are taken of the cornea as it passes through the blood vessels. Fluorescein angiography identifies areas of neovascularization and leakage, which are indicators of inflammation and possible rejection.
- Confocal Microscopy: Confocal microscopy produces in-vivo, high-resolution images of the cornea at the cellular level. This technique is useful for detecting inflammatory cells, keratic precipitates, and other microscopic changes linked to graft rejection. It provides a comprehensive evaluation of the corneal layers and aids in the diagnosis of early rejection.
- Corneal Topography: Corneal topography maps the cornea’s surface curvature, revealing its shape and any irregularities. This technique can detect changes in corneal curvature and thickness, which may indicate graft rejection. Topographic changes like increased astigmatism or irregularity can be early indicators of stromal or endothelial rejection.
- Tear Cytokine Analysis: New research suggests that analyzing cytokine levels in tear fluid can provide useful information about the inflammatory status of the eye. Certain cytokine levels may be elevated, indicating an ongoing immune response and potential graft rejection. This non-invasive technique is still being investigated, but it shows promise for early rejection detection.
- Ultrasound Biomicroscopy: This imaging technique employs high-frequency ultrasound to produce detailed images of the eye’s anterior segment, including the cornea. Ultrasound biomicroscopy is especially useful in determining the depth and extent of corneal edema and other structural changes caused by graft rejection.
Ophthalmologists can use these diagnostic methods to accurately diagnose corneal graft rejection, determine its severity, and devise an appropriate treatment plan to avoid graft failure.
Corneal Graft Rejection Treatment Options
The goal of treating corneal graft rejection is to stop the immune response, preserve graft function, and prevent graft failure. Here are the standard and innovative therapies:
Standard Treatments
- Topical corticosteroids are the primary treatment for corneal graft rejection. These medications reduce inflammation and suppress the immune response, thereby preventing further damage to the graft. High-potency steroids, such as prednisolone acetate, are frequently used first, with the dosage gradually tapered as the condition improves.
- Systemic Immunosuppressants: In severe or resistant rejection, systemic immunosuppressive agents such as oral corticosteroids (e.g., prednisone) or cyclosporine may be used. These medications help regulate the immune response throughout the body and are usually used in conjunction with topical treatments.
- Antibiotic and Antiviral Therapy: If an infection is suspected or confirmed as a cause of rejection, appropriate antibiotic or antiviral medications are given. These treatments help to clear the infection and reduce inflammation, preventing further immune activation.
- Cycloplegics: Atropine or cyclopentolate can be used to dilate the pupil and alleviate pain caused by ciliary spasm. These medications also help to reduce the risk of synechiae, which occur when the iris adheres to the cornea or lens.
Innovative and Emerging Therapies
- Anti-VEGF Therapy: VEGF inhibitors, such as bevacizumab, are being studied as treatments for corneal neovascularization. By inhibiting the formation of new blood vessels, these agents help to maintain the cornea’s immune-privileged status and reduce the likelihood of rejection.
- Biologic Agents: Monoclonal antibodies and other biologic agents that target specific components of the immune response are being studied for their ability to treat corneal graft rejection. Agents such as rituximab, which targets B cells, and infliximab, which targets tumor necrosis factor (TNF), have demonstrated promise in lowering rejection rates.
- Gene Therapy: Research into gene therapy seeks to modify the immune response at the genetic level, potentially providing long-term protection against graft rejection. This novel approach is still in the experimental stage, but it provides hope for more effective and targeted treatments in the future.
- Stem Cell Therapy: Stem cell-based therapies are under investigation for their ability to regenerate damaged corneal tissue and improve graft survival. These treatments use stem cells to repair or replace damaged cells in the graft, promoting healing while lowering the risk of rejection.
- Amniotic Membrane Transplantation: When graft rejection occurs, amniotic membrane transplantation can be used as an adjunctive treatment to reduce inflammation and promote healing. The amniotic membrane supports the cornea and contains anti-inflammatory and scarring properties.
By combining these traditional and novel treatment approaches, ophthalmologists can effectively manage corneal graft rejection, increase graft survival rates, and improve patients’ vision.
Trusted Resources
Books
- “Corneal Transplantation: A History in Profiles” by M. Soledad Cortina
- “Keratoplasty: Techniques and Complications” by Christopher J. Rapuano






