Introduction to Corneal Laceration
A corneal laceration is a serious ocular injury caused by a cut or tear in the cornea, the clear, dome-shaped surface that protects the front of the eye. This condition can result from trauma caused by sharp objects, accidents, or high-velocity impacts. Corneal lacerations range in severity, from superficial cuts that only affect the cornea’s outer layers to deep lacerations that penetrate the entire thickness of the cornea, potentially resulting in vision loss and other complications. Prompt medical attention is critical for avoiding infection, scarring, and permanent damage. Understanding the causes, symptoms, and risks associated with corneal lacerations is critical for successful prevention and treatment.
Corneal Laceration Insight
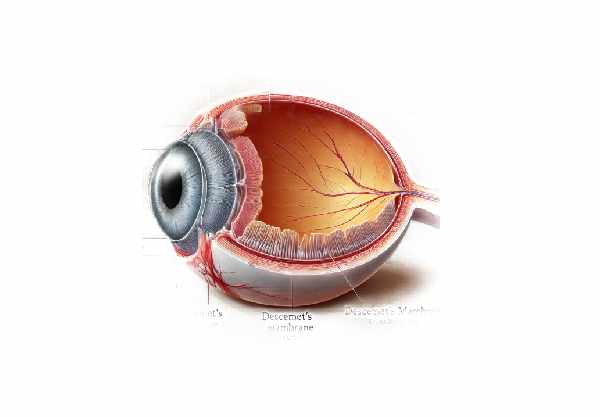
Corneal lacerations are classified according to the depth and extent of the injury. The cornea has five layers: the epithelium, Bowman’s layer, stroma, Descemet’s membrane, and endothelium. A laceration can occur in any or all of these layers, and the severity of the injury determines the urgency and type of treatment needed.
Causes and Risk Factors
- Sharp Object Trauma: Knives, scissors, metal shards, and glass are common sources of injury. These incidents can occur in a variety of settings, including the workplace, the home, or during recreational activities.
- Automobile Accidents: High-impact collisions can cause debris to strike the eye, or the eye may come into contact with shattered glass or other sharp objects.
- Sports Injuries: Contact sports and activities involving fast-moving objects, such as baseball, hockey, or racquetball, increase the risk of corneal lacerations.
- Industrial Accidents: Workers in construction, metalworking, and other industrial settings are more vulnerable due to the nature of their work environment and the tools they use.
- Domestic Incidents: Everyday activities like cooking, cleaning, and gardening can result in accidental eye injuries if proper precautions are not followed.
Symptoms
A corneal laceration typically causes immediate and severe symptoms, necessitating prompt medical evaluation:
- Severe Pain: Because the cornea is densely innervated, a laceration usually results in intense pain.
- Blurred Vision: Damage to the corneal structure can cause significant vision impairment, ranging from mild blurriness to complete vision loss.
- Tearing and Discharge: The eye’s natural response to injury is excessive tearing and, in some cases, discharge, especially if there is an infection.
- Redness and Inflammation: The injured eye is frequently red and inflamed due to the body’s inflammatory response to trauma.
- Photophobia: Increased sensitivity to light is common, making the patient uncomfortable in bright environments.
- Foreign Body Sensation: Patients frequently report that something is stuck in their eye.
Pathophysiology
The pathophysiology of corneal lacerations includes both mechanical damage to the corneal layers and the following biological response aimed at healing the injury:
- Mechanical Disruption: The initial trauma breaks the continuity of the corneal layers. Depending on the depth, this can damage the epithelium, stroma, Descemet’s membrane, and even the endothelium.
- Inflammatory Response: After an injury, the body initiates an inflammatory response to contain and repair the damage. Inflammatory cells migrate to the area of injury, causing redness, swelling, and pain.
- Healing and Repair: The cornea has an incredible ability to heal, but the process is dependent on the severity of the injury. Superficial lacerations primarily involve epithelial cell migration and proliferation, whereas deeper injuries necessitate more complex repair mechanisms involving the stroma and endothelial cells.
- Complications: Without prompt and appropriate treatment, corneal lacerations can result in infections, scarring, corneal perforation, and secondary glaucoma due to increased intraocular pressure.
Impact on Vision
The impact of a corneal laceration on vision is determined by the location and extent of the injury.
- Superficial Lacerations: These injuries affect only the epithelium and Bowman’s layer and may cause temporary vision disturbances, but if treated properly, they usually heal without significant long-term effects.
- Deep Lacerations: These injuries involve the stroma and may reach Descemet’s membrane or the endothelium, increasing the risk of complications such as scarring and permanent vision loss. The cornea’s clarity and refractive properties can be significantly altered, resulting in astigmatism and other vision impairments.
- Central vs. Peripheral Lacerations: Lacerations in the central cornea are more likely to directly affect vision due to their location over the pupil, whereas peripheral lacerations may cause less immediate visual disturbance but can still result in complications such as scarring or peripheral vision loss.
Healing and Recovery
The healing process for corneal lacerations includes several stages, depending on the severity and treatment received:
- Initial Response: The body’s first response to corneal injury is inflammation, pain, and increased tear production to flush out debris.
- Cell Migration and Proliferation: Epithelial cells migrate and multiply to cover the defect. In deeper lacerations, keratocytes in the stroma are activated to aid in healing.
- Collagen Remodeling: To restore the structural integrity of the cornea, stromal lacerations are repaired through the deposition and remodeling of collagen.
- Endothelial Healing: If the endothelium is involved, endothelial cells may spread to cover the defect, but their regenerative capacity is limited, potentially leading to long-term complications.
- Scar Formation: Depending on the depth and treatment of the injury, scar tissue may form, potentially affecting the cornea’s transparency and refractive properties.
Corneal Laceration Prevention Strategies
- Wear Protective Eyewear: Always wear safety glasses or goggles when doing activities that could cause eye injury, such as construction work, metalworking, sports, or using power tools.
- Use Eye Protection in High-Risk Environments: In environments with high exposure to dust, debris, or flying particles, wear appropriate eye protection to prevent foreign objects from causing injury.
- Exercise Caution with Sharp Objects: Use knives, scissors, and other sharp tools with care. When using these tools, keep them pointed away from your face and eyes.
- Follow Safety Protocols at Work: To reduce the risk of ocular injuries, follow workplace safety guidelines, such as using protective equipment and safe handling procedures.
- Educate Children: Teach children the value of eye safety and make sure they wear protective eyewear during sports and recreational activities that could cause eye injuries.
- Proper Storage of Hazardous Materials: To avoid accidental injuries, keep hazardous materials, such as chemicals and sharp objects, securely stored and out of the reach of children.
- Be Cautious During Home Repairs: When performing home repairs or maintenance, wear appropriate eye protection to avoid injuries from tools, chemicals, or flying debris.
- Avoid Rubbing Your Eyes: If you feel anything in your eye, don’t rub it. Instead, gently remove the foreign object from your eye by rinsing it with clean water or saline.
- Use Protective Gear for Sports: To protect your eyes, wear helmets with face shields or sports goggles when participating in sports that involve high-speed objects or physical contact, such as baseball, racquetball, or hockey.
- Regular Eye Check-Ups: Schedule regular eye exams to keep your eyes healthy and detect any potential problems early. Early detection and treatment of eye conditions can help prevent more serious injuries.
Diagnostic Approaches for Corneal Laceration
Diagnosing a corneal laceration entails a thorough clinical examination as well as the application of various diagnostic techniques to determine the scope and severity of the injury. Here are the main methods used:
- Patient History and Symptom Assessment: The diagnostic process begins with a thorough patient history to determine the cause of injury and the symptoms experienced. Important information includes the cause of the injury, the time it occurred, and any immediate actions taken.
- Slit Lamp Examination: A slit lamp is an important tool for examining the cornea in detail. During this examination, the ophthalmologist uses a high-intensity light source and a microscope to magnify the cornea. This allows for the determination of the laceration’s depth and extent, as well as any foreign bodies and associated injuries like corneal edema or hyphema (blood in the anterior chamber).
- Fluorescein Staining: Fluorescein dye is applied to the eye’s surface, and the cornea is illuminated with cobalt blue light. This technique fluoresces defects in the corneal epithelium, making it easier to determine the precise location and size of the laceration.
- Seidel Test: This test is used to detect aqueous humor leakage from the anterior chamber via a corneal laceration. Fluorescein dye is applied to the eye; if there is a leak, the dye dilutes and forms a stream, indicating a full-thickness laceration.
- Anterior Segment Optical Coherence Tomography (AS-OCT): AS-OCT produces high-resolution cross-sections of the cornea. It is useful for determining the depth of a laceration and observing structural changes within the cornea. This non-invasive imaging technique provides detailed information about the extent of the injury, which aids in treatment decisions.
- Ultrasound Biomicroscopy: This advanced imaging technique uses high-frequency ultrasound to produce detailed images of the eye’s anterior segment. It is especially useful when the cornea is too opaque for other imaging methods, allowing for the examination of deeper structures and the detection of additional ocular damage.
- B-Scan Ultrasonography: When a corneal laceration is accompanied by significant anterior segment inflammation or opacification, B-scan ultrasonography can be used to assess the posterior segment of the eye. This technique aids in the identification of any vitreous hemorrhage, retinal detachment, or intraocular foreign bodies that may not be visible on direct examination.
- X-rays or CT Scans: These imaging modalities are used to detect a foreign body, especially if it is metallic or has penetrated deeper into the eye. X-rays and CT scans provide detailed images of the eye’s structure, which aids in the detection and evaluation of the foreign object.
Combining these diagnostic methods allows ophthalmologists to accurately assess the severity of corneal lacerations and devise an appropriate treatment plan to avoid complications and promote healing.
Corneal Laceration: Healing Techniques
The treatment of corneal lacerations is intended to prevent infection, promote healing, and restore vision. Here are some emerging therapies, as well as standard treatment options:
- Topical Antibiotics: To avoid infection, broad-spectrum antibiotic eye drops or ointments are recommended. These medications help to lower the risk of bacterial colonization at the injury site.
- Cycloplegic Agents: Drops containing cyclopentolate or atropine are used to dilate the pupil and relieve pain caused by ciliary muscle spasms. These medications also help to prevent the formation of synechiae.
- Tetanus Prophylaxis: If the injury involves contact with soil or other potential sources of Clostridium tetani, tetanus prophylaxis is given to prevent tetanus infection.
- Surgical Intervention: For full-thickness lacerations or those that cause significant structural damage, surgical repair is frequently required. The procedure entails suturing the corneal wound to preserve its integrity and prevent further damage. Specialized techniques and instruments are used to close the laceration precisely and effectively.
- Bandage Contact Lenses: Soft bandage contact lenses can help to protect the cornea, relieve pain, and promote epithelial healing. These lenses act as a barrier against mechanical irritation from the eyelids, creating a stable environment for healing.
- Patch and Shield: In cases of minor lacerations, patching the eye with a sterile dressing and a protective shield can help immobilize the eyelids and prevent further injury while the cornea heals.
Innovative and Emerging Therapies
- Amniotic Membrane Transplantation: The amniotic membrane, which is derived from the placenta’s innermost layer, has anti-inflammatory and scarring properties. It can be used as a graft or a contact lens to promote healing and reduce inflammation after severe corneal lacerations.
- Fibrin Glue: Fibrin glue, a biological adhesive, is increasingly used to close corneal lacerations. It can be a viable alternative to sutures for minor to moderate lacerations, reducing surgical time and promoting faster healing with less scarring.
- Gene Therapy: Researchers are looking into ways to improve corneal healing and reduce scarring. Gene therapy seeks to improve outcomes for patients suffering from severe corneal injuries by targeting specific genes involved in the wound healing process.
- Stem Cell Therapy: Stem cell-based treatments are being studied for their ability to regenerate damaged corneal tissue. Stem cell therapy, which promotes the growth of healthy corneal cells, could provide a revolutionary approach to treating severe corneal lacerations and preventing long-term complications.
- Corneal Cross-Linking (CXL): Originally used to treat keratoconus, CXL is now being studied as a treatment to strengthen the corneal tissue near the laceration site. CXL can help stabilize and heal the cornea by increasing cross-links between collagen fibers.
- Nanotechnology-Based Drug Delivery: Advances in nanotechnology are enabling the creation of targeted drug delivery systems for the eye. These systems can deliver antibiotics, anti-inflammatory agents, and other medications directly to the site of injury, improving treatment efficacy and minimizing side effects.
Trusted Resources
Books
- “Corneal Disorders: Clinical Diagnosis and Management” by Howard M. Leibowitz
- “Corneal Surgery: Theory, Technique and Tissue” by Frederick S. Brightbill
Online Resources
- American Academy of Ophthalmology
- National Eye Institute
- [MedlinePlus:






