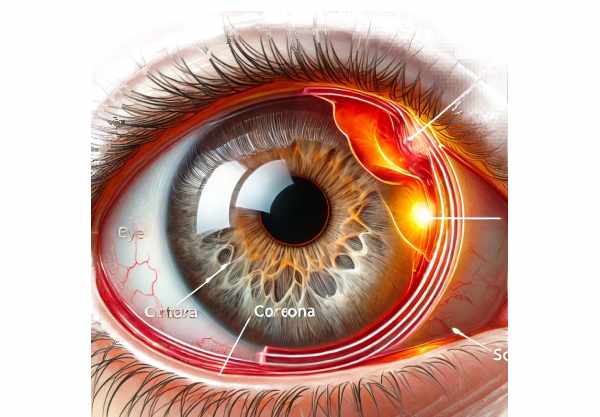
Overview of Corneal Ulcers
A corneal ulcer is a painful, open sore on the cornea, the transparent, dome-shaped surface that covers the front of the eye. This is a serious ocular emergency that, if not treated promptly, can cause significant vision impairment. Corneal ulcers can develop from a variety of causes, including infections, physical trauma, and certain underlying diseases. They are frequently associated with intense pain, redness, discharge, and blurred vision. Early diagnosis and treatment are critical in avoiding complications like scarring or even vision loss. Understanding the nature, causes, and preventive measures of corneal ulcers is critical for maintaining ocular health and receiving timely medical attention when necessary.
Corneal Ulcers: Key Information
Corneal ulcers are a serious condition that affects the clear, outermost layer of the eye. This layer, known as the cornea, is essential for focusing vision. When this layer is damaged or infected, it can lead to an ulcer, which impairs visual acuity and eye health.
Etiology
Corneal ulcers can be caused by a variety of conditions, the most common of which are infections. These infections may be bacterial, viral, fungal, or parasitic in nature. Bacterial corneal ulcers are common in contact lens wearers, especially when the lenses are not properly cleaned or are worn for an extended period. Pseudomonas aeruginosa and Staphylococcus aureus are common bacteria that cause this. Viral infections, particularly those caused by the herpes simplex virus, can result in recurring corneal ulcers. Fungal infections, while less common, can occur, particularly in people who have suffered an eye injury involving organic material such as plant matter. Parasitic infections, such as those caused by Acanthamoeba, are uncommon but severe, and are frequently linked to poor contact lens hygiene or exposure to contaminated water.
Non-infectious Causes
Aside from infections, corneal ulcers can develop from non-infectious causes. These include physical trauma, such as scratches from foreign objects, chemical burns, and prolonged use of contact lenses. Autoimmune conditions, such as rheumatoid arthritis and Sjögren’s syndrome, can also cause corneal ulceration due to decreased tear production and subsequent dryness. Other factors include severe dry eye syndrome and ultraviolet light exposure.
Pathophysiology
The pathophysiology of corneal ulcers involves the disruption of the corneal epithelium, which allows pathogens or irritants to enter the underlying stroma. This causes an inflammatory response, which is characterized by immune cell infiltration, inflammatory mediator release, and tissue damage. The ulcerative process can cause stromal thinning, scarring, and, in severe cases, corneal perforation, which can result in intraocular infection and vision loss.
Symptoms and Signs
Corneal ulcers present clinically with severe eye pain, redness, tearing, and the sensation of a foreign body in the eye. Patients frequently report photophobia (sensitivity to light) and blurred vision. Purulent discharge may be present, particularly in bacterial infections. On examination, an ulcer appears as a white or greyish spot on the cornea, which may be accompanied by corneal edema and hypopyon (pus accumulation in the eye’s anterior chamber).
Risk Factors
Several risk factors predispose people to corneal ulcers. Improper contact lens use, including overnight wear and inadequate disinfection, greatly increases the risk. Eye trauma and previous ocular surgeries can also increase the cornea’s susceptibility to ulcers. Individuals with weakened immune systems, whether due to systemic diseases such as diabetes or the use of immunosuppressive medications, are at a greater risk. Chronic ocular surface diseases, such as blepharitis (eyelid inflammation) and lagophthalmos (incomplete eyelid closure), also play a role in the development of corneal ulcers.
Complications
If not treated promptly, corneal ulcers can cause a variety of complications. Scarring of the cornea is a common complication that can impair vision depending on the size and location of the scar. In severe cases, the cornea can perforate, resulting in endophthalmitis, an infection of the eye’s interior that can cause vision loss. Chronic or recurrent ulcers can also cause persistent epithelial defects and neovascularization (the formation of new blood vessels in the cornea), which impairs corneal transparency and vision.
Psychological and Social Impact
The consequences of corneal ulcers go beyond physical symptoms. The associated pain and vision loss can have a significant impact on a person’s quality of life, causing emotional distress and difficulties with daily activities. This condition can also have societal implications, such as decreased productivity and higher healthcare costs. Awareness and education about preventive measures are critical in mitigating these consequences.
Advanced Understanding
Understanding corneal ulcers in depth entails recognizing the complex interplay between the corneal epithelium, immune response, and microbial or non-microbial insults. The molecular mechanisms underlying corneal healing, as well as the role of different cytokines and growth factors in the repair process, are still being investigated. Diagnostic technique advancements, such as in vivo confocal microscopy and molecular assays, improve the ability to detect and characterize corneal ulcers more accurately. Furthermore, advances in therapeutic approaches, such as novel antimicrobial agents, immunomodulatory therapies, and regenerative medicine, show promise for improving outcomes in patients with corneal ulcers.
Corneal Ulcers Prevention Tips
- Maintain proper contact lens hygiene. Always wash your hands before handling contact lenses. Clean and disinfect your lenses as recommended, and avoid wearing them overnight or for long periods of time.
- Protect Your Eyes from Injury: Wear protective eyewear when participating in activities that could result in eye injury, such as sports, construction work, or chemical handling.
- Avoid Contaminated Water: Do not expose contact lenses to water, such as swimming pools, hot tubs, or tap water, as these can contain harmful microorganisms.
- Manage Underlying Health Conditions: Properly manage chronic conditions such as diabetes and autoimmune diseases to reduce your risk of developing corneal ulcers.
- Treat Eye Infections Promptly: Seek medical attention if you notice any symptoms of an eye infection, such as redness, discharge, or pain, to avoid complications.
- Use Preservative-Free Artificial Tears: For people who have dry eyes, using preservative-free artificial tears can help keep the cornea hydrated and lower the risk of ulceration.
- Avoid Eye Rubbing: Avoid rubbing your eyes, as this can cause microtrauma and increase the risk of infection, particularly if your hands are dirty.
- Regular Eye Examinations: Schedule regular eye exams with an ophthalmologist or optometrist to detect and treat potential problems early.
Corneal Ulcers Diagnostic Techniques
Diagnosing corneal ulcers requires a combination of clinical evaluation and specialized diagnostic techniques. The process usually starts with a thorough patient history and physical examination. The ophthalmologist will ask about your symptoms, contact lens use, trauma history, and any underlying medical conditions.
Slit Lamp Examination
Slit lamp biomicroscopy is an important diagnostic tool for corneal ulcers. This instrument enables a thorough examination of the eye’s anterior segment, including the cornea. Using high-intensity light and magnification, the ophthalmologist can see the ulcer’s size, depth, and location, as well as any associated corneal edema, infiltrates, or hypopyon.
Fluorescein Staining
Fluorescein staining is an important diagnostic tool for detecting corneal ulcers. Fluorescein dye is applied to the ocular surface to highlight epithelial damage. Areas of corneal ulceration appear bright green under cobalt blue light, making it possible to precisely assess the extent of the ulcer.
Microbial Culture and Sensitivity Testing
Corneal scrapings are taken and sent for microbial cultures and sensitivity testing to determine the causative pathogen, especially in cases where infection is suspected. During this procedure, samples are collected from the ulcerated area using a sterile instrument. The samples are then cultured to identify bacterial, fungal, or parasitic organisms, and sensitivity testing is used to determine the most effective antimicrobial treatment option.
Polymerase Chain Reaction(PCR)
PCR is a sophisticated molecular diagnostic technique that detects viral pathogens such as herpes simplex virus. This method amplifies the virus’s DNA, allowing for rapid and accurate identification. PCR is especially useful when conventional culture methods are inconclusive or slow.
Confocal Microscopy
In vivo confocal microscopy is a novel diagnostic technique that produces high-resolution images of the cornea at the cellular level. This technique is particularly useful for detecting fungal and Acanthamoeba infections, which can be difficult to diagnose using conventional methods. Confocal microscopy enables the visualization of fungal filaments and amoebic cysts within the corneal tissue.
Anterior Segment Optical Coherence Tomography (AS-OCT)
AS-OCT is a non-invasive imaging technique for obtaining cross-sectional images of the cornea. This technology can help determine the depth and extent of the ulcer, as well as monitor treatment response. It is especially useful when the ulcer is deep and affects the central visual axis.
Corneal Ulcers: Treatment Methods
Treating corneal ulcers entails identifying the underlying cause, alleviating symptoms, and avoiding complications. The type of treatment is determined by the cause of the ulcer, the severity of the condition, and the presence of any underlying diseases.
Standard Treatment Options
For bacterial corneal ulcers, broad-spectrum antibiotic eye drops are usually prescribed first, followed by targeted therapy based on culture and sensitivity findings. Fluoroquinolones, aminoglycosides, and cephalosporins are among the most commonly used antibiotics. In severe cases, fortified antibiotics, which are specially compounded at higher concentrations, may be used.
Antiviral medications such as acyclovir, ganciclovir, or valacyclovir are used to treat viral corneal ulcers, specifically those caused by the herpes simplex virus. These can be administered topically as eye drops or ointments, or orally in more severe cases.
Antifungal eye drops, such as natamycin or voriconazole, are required to treat fungal corneal ulcers. Fungal infections can be particularly difficult to treat and frequently necessitate prolonged treatment.
Acanthamoeba keratitis, a severe parasitic infection, is treated with a combination of anti-amoebic agents such as polyhexamethylene biguanide (PHMB) and chlorhexidine. Given Acanthamoeba cysts’ resistance, treatment is usually prolonged.
Adjunctive Treatment
Adjunctive treatments are intended to promote healing and alleviate symptoms. Cycloplegic agents, such as atropine or cyclopentolate, can be used to treat ciliary spasm pain. Lubricating eye drops or ointments can help keep the cornea hydrated and comfortable.
Surgical Interventions
When medical treatment fails or complications arise, surgical interventions may be required. Debridement, or the mechanical removal of infected and necrotic tissue, can reduce microbial load and improve the efficacy of topical treatments. In severe cases, especially those involving corneal perforation, a corneal transplant (keratoplasty) may be necessary to restore ocular integrity and vision.
Emerging Therapies
To improve outcomes, researchers are looking into innovative and emerging therapies for corneal ulcers. Amniotic membrane transplantation, for example, has demonstrated promise in promoting corneal healing and decreasing inflammation. The amniotic membrane, which is anti-inflammatory and anti-scarring, can be used as a biological bandage on the cornea’s surface.
Stem cell therapy is another emerging field, with research focusing on the regeneration of damaged cornea tissue. The use of cultured limbal stem cells to replace damaged corneal epithelial cells is currently under investigation.
Trusted Resources
Books
- “Keratitis and Corneal Ulcers” by Thomas Reinhard and Frank Larkin
- “Corneal Disorders: Clinical Diagnosis and Management” by Gilbert Smolin, Charles Stephen Foster, and Dimitri T. Azar






