What is Cortical Cataract?
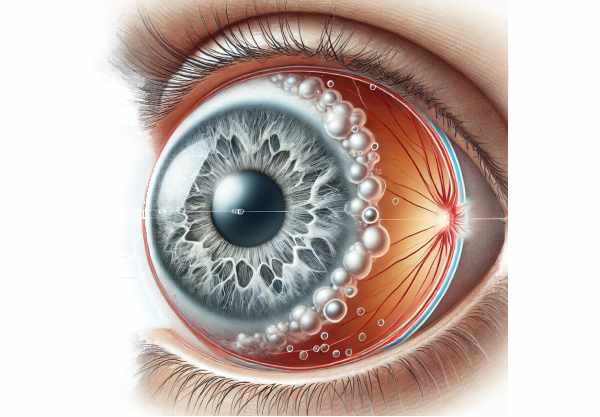
A cortical cataract is a type of cataract that affects the lens of the eye, causing vision impairment. This condition is distinguished by the appearance of opaque, white opacities or cloudy areas in the lens cortex, the outermost part of the lens. These opacities are often shaped like spokes on a wheel and extend from the lens’s periphery to its center. Cortical cataracts can cause serious visual problems, such as blurred vision, glare, and difficulty seeing at night. Understanding the underlying causes, risk factors, and potential preventive measures is critical for maintaining ocular health and slowing the progression of cortical cataracts.
Cortical Cataract Insights
Cortical cataracts are one of the most common types of cataracts, distinguished by a distinctive pattern of opacities in the lens cortex. They have a significant impact on vision and quality of life, particularly in older adults.
Etiology
Cortical cataracts are most commonly caused by aging. As people age, the proteins in their lenses change, resulting in the formation of opacities. However, age is not the only factor to consider. Several other factors may contribute to the development of cortical cataracts, including:
- Genetic Predisposition: A family history of cataracts raises the risk of developing the condition.
- Environmental Factors: Prolonged exposure to ultraviolet (UV) radiation poses a significant risk. UV light can cause oxidative stress, which can damage the lens fibers and proteins.
- Medical Conditions: Diabetes has been linked to accelerated cataract formation. High blood sugar levels can cause changes in lens metabolism, which promotes cataract development.
- Lifestyle Factors: Smoking and excessive alcohol consumption have been associated with an increased risk of cortical cataracts. These habits promote oxidative stress and lens damage.
Pathophysiology
The eye’s lens is made of water and proteins that are precisely arranged to maintain transparency and function. In cortical cataracts, the orderly arrangement of these proteins is disrupted, resulting in opaque areas. The lens cortex, which surrounds the lens’s central nucleus, becomes cloudy as these opacities accumulate. The exact mechanism includes:
- Oxidative Stress: Free radicals from UV exposure, smoking, and metabolic disorders cause oxidative damage to lens proteins and fibers.
- Protein Aggregation: Oxidative stress causes the aggregation and denaturation of lens proteins, resulting in opacities.
- Electrolyte Imbalance: Changes in electrolyte balance within lens fibers can cause fluid accumulation and swelling, which contributes to cataract formation.
Clinical Manifestations
Cortical cataracts cause a variety of symptoms that differ depending on the size and location of the opacities. Common symptoms include:
- Blurred Vision: As the cataract progresses, vision becomes more blurred and hazy.
- Glare and Halos: People frequently experience glare and halos around lights, especially at night, which makes driving difficult.
- Double Vision: When opacities scatter light, it can cause monocular diplopia (double vision in one eye).
- Reduced Contrast Sensitivity: There is a noticeable decrease in the ability to distinguish between different shades and contrasts, which affects daily activities.
Risk Factors
Several risk factors are linked to the development of cortical cataracts, including:
- Age: Aging is the most significant risk factor, with cataracts becoming more common as people get older.
- Genetics: A family history of cataracts may indicate a genetic predisposition to the condition.
- Sun Exposure: Prolonged exposure to ultraviolet radiation raises the risk of developing cortical cataracts.
- Diabetes: Diabetic patients are at a higher risk because of changes in lens metabolism and increased oxidative stress.
- Smoking and Alcohol: Both smoking and excessive alcohol consumption are associated with an increased risk of cataracts.
- Nutritional Deficiencies: Low-antioxidant diets, such as those lacking vitamins C and E, can contribute to cataract development.
Complications
Left untreated, cortical cataracts can cause significant visual impairment and complications, such as:
- Severe Vision Loss: Progressive opacification can cause severe vision loss, limiting an individual’s ability to perform daily tasks.
- Increased Risk of Falls: Impaired vision raises the risk of falls and associated injuries, especially in older adults.
- Secondary Glaucoma: Advanced cortical cataracts can cause elevated intraocular pressure and secondary glaucoma.
- Lens Dislocation: In rare cases, the supporting structures may weaken, causing the lens to become dislocated.
Psychological and Social Impact
Cortical cataracts have far-reaching consequences beyond their physical symptoms. The condition can significantly impact the individual’s quality of life, resulting in:
- Reduced Independence: Impaired vision can make it difficult to complete daily tasks, resulting in decreased independence.
- Emotional Distress: Loss of vision and the fear of blindness can result in anxiety and depression.
- Social Isolation: Difficulty participating in social activities can result in social isolation and a drop in overall well-being.
Tips for Cortical Cataracts Prevention
- Protect your eyes from UV rays. When outdoors, wear sunglasses that block 100% of UV rays to reduce the risk of lens damage caused by UV exposure.
- Manage Chronic Conditions: Keep medical conditions like diabetes under control to avoid metabolic changes that can cause cataracts.
- Maintain a Healthy Diet: To protect the lens from oxidative damage, consume a well-balanced diet rich in antioxidants, such as vitamins C and E.
- Avoid Smoking: Smoking causes an increase in the production of free radicals, which can damage the lens.
- Reduce Alcohol Consumption: Drink less alcohol to reduce the risk of oxidative stress and its effects on the lens.
- Regular Eye Check-ups: Schedule regular eye exams to detect early signs of cataracts and other ocular problems.
- Stay Hydrated: Stay hydrated to keep your eyes healthy and prevent lens dehydration.
- Wear Protective Eyewear: Wear protective eyewear when participating in activities that increase the risk of eye injury, such as sports or certain occupations.
Diagnostic Methods:
Cortical cataracts are diagnosed using a combination of clinical evaluation and specialized diagnostic techniques to accurately assess their presence and severity. Early and accurate diagnosis is critical for successful management and treatment planning.
Comprehensive Eye Examination
The diagnostic process begins with a thorough eye examination by an ophthalmologist or optometrist. This exam includes:
- Visual Acuity Test: An eye chart is used to assess the patient’s visual acuity at various distances. Reduced visual acuity may indicate the presence of a cataract.
- Slit Lamp Examination: An ophthalmologist uses a slit lamp, a microscope with a bright light, to examine the front structures of the eye, such as the cornea, iris, and lens. The slit lamp provides a detailed view of the lens, making it easier to identify the distinctive opacities of cortical cataract.
- Retinal Examination: Using an ophthalmoscope, the doctor examines the retina to rule out other potential causes of vision loss and assess the overall health of the eyes.
Dilated Eye Examination
To obtain a better view of the lens and the extent of the cataract, the ophthalmologist may dilate (widen) the pupil using eye drops. This allows for a more thorough examination of the lens, which aids in determining the specific type and location of the cataract.
Imaging Techniques
Advanced imaging techniques are increasingly being used to help diagnose cortical cataracts.
- Optical Coherence Tomography (OCT): OCT is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the eye’s structures. It is especially useful for determining the size and density of the cataract, as well as tracking changes over time.
- Scheimpflug Imaging: This technique uses a specialized camera to take detailed images of the lens. Scheimpflug imaging aids in the quantitative assessment of lens opacities and is useful for planning cataract surgery.
Specialized Tests
In some cases, additional tests may be required to diagnose cortical cataracts and assess their impact on vision:
- Glare Test: This test assesses how glare affects the patient’s vision, which is a common sign of cortical cataracts. The test is useful in determining the functional impact of cataracts on daily activities, particularly driving at night.
- Contrast Sensitivity Test: This test determines the patient’s ability to distinguish between various shades of gray. Cortical cataracts frequently reduce contrast sensitivity, making it difficult to see in low light conditions.
Emerging Diagnostic Technologies
Innovative diagnostic technologies are being developed to improve the accuracy and efficiency of cataract detection:
- Wavefront Aberrometry: This cutting-edge technology determines how light waves travel through the eye, revealing distortions caused by lens opacities. Wavefront aberrometry provides detailed information about the eye’s optical quality, allowing cataract surgery to be tailored to the patient.
- Artificial Intelligence (AI) in Ophthalmology: AI algorithms are being developed to analyze imaging data and detect cataract patterns with high precision. These technologies have the potential to transform cataract diagnosis by providing quick, objective evaluations.
Cortical Cataracts: Treatment Methods
Cortical cataract treatment aims to restore clear vision while also improving the patient’s quality of life. Treatment options differ according to the severity of the cataract and the patient’s overall health and preferences.
Non-surgical Management
In the early stages of cortical cataracts, when symptoms are mild, non-surgical treatment may be sufficient. This includes:
- Prescription Glasses: Changing the patient’s prescription for glasses or contact lenses can improve vision and relieve symptoms.
- Anti-Glare Coatings: Anti-glare coatings on glasses can help reduce glare and halos, which is especially useful when driving at night.
- Enhanced Lighting: Using brighter lights for reading and other activities can help compensate for poor vision.
Surgical Treatment
When cortical cataracts cause significant vision impairment and interfere with daily activities, surgery is the most effective treatment. The typical surgical procedure for cataracts is:
- Phacoemulsification: This is the most common cataract surgery procedure. The procedure entails making a small incision in the cornea and inserting an ultrasonic probe to break up (emulsify) the cloudy lens. The fragmented pieces are then suctioned out, and an artificial intraocular lens (IOL) replaces the natural lens. Phacoemulsification is a minimally invasive procedure with a high success rate and a short recovery period.
- Extracapsular Cataract Extraction (ECCE): In cases where phacoemulsification is not appropriate, ECCE may be used. This requires making a larger incision to remove the entire cloudy lens in one piece before inserting the IOL. This method is less common because it takes longer to recover and has a higher risk of complications than phacoemulsification.
Innovative and Emerging Therapies
Research and technological advancements are resulting in innovative treatments for cortical cataracts:
- Femtosecond Laser-Assisted Cataract Surgery: This technique employs a femtosecond laser to perform critical steps in cataract surgery, such as making incisions and fragmenting the lens. It provides greater precision and potentially better results than traditional methods.
- Extended Depth of Focus (EDOF) Lenses: EDOF lenses are a type of IOL that provides a continuous range of vision, reducing the need for glasses after cataract surgery. These lenses can improve both near and distance vision, resulting in better overall visual performance.
- Multifocal and Accommodative IOLs: These advanced IOLs are designed to restore a wider range of vision by mimicking the eye’s natural focus ability. Multifocal IOLs have multiple focal points, whereas accommodative IOLs change position within the eye to focus at various distances.
- Nanotechnology-Based Treatments: Researchers are investigating the use of nanoparticles to deliver drugs directly to the lens, which could prevent or reverse cataract formation. These treatments are still in the experimental stages, but they show promise for non-surgical cataract management.
Trusted Resources
Books
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski and Brad Bowling
- “Lens and Cataract” by David F. Chang
- “Cataract Surgery: Expert Consult” by Roger F. Steinert and David F. Chang










