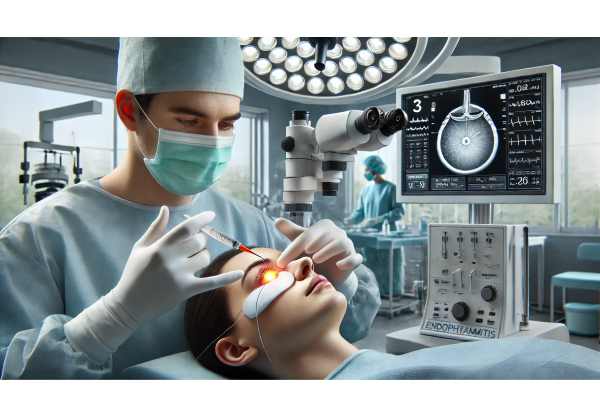
Endophthalmitis is a severe, sight-threatening inflammation of the intraocular cavities, most often triggered by infection. Rapid diagnosis and effective intervention are essential for preserving vision and, in some cases, the eye itself. Patients may face this emergency after eye surgery, trauma, or via bloodstream infections, with symptoms escalating quickly from discomfort to devastating visual loss. In this comprehensive guide, you’ll discover the latest evidence-based approaches to prevention, diagnosis, and management—including conventional treatments, surgical solutions, and cutting-edge advances—so patients, caregivers, and clinicians can make informed, confident decisions at every step.
Table of Contents
- Understanding Endophthalmitis: Nature, Patterns, and Risk Factors
- Pharmacological and Conservative Treatments for Endophthalmitis
- Surgical and Interventional Solutions
- Innovative Research and New Technologies
- Current Clinical Trials and Future Outlook
- Frequently Asked Questions
Understanding Endophthalmitis: Nature, Patterns, and Risk Factors
Definition and Pathophysiology
Endophthalmitis is a critical inflammatory condition affecting the interior of the eye—primarily the vitreous and aqueous humors—most commonly caused by bacteria or fungi. The infectious agents rapidly multiply within the closed eye environment, triggering an intense immune response. Without swift, targeted intervention, this inflammation can lead to irreversible damage to ocular tissues, culminating in severe vision loss or even blindness.
Types of Endophthalmitis
- Exogenous Endophthalmitis: Follows direct entry of organisms into the eye, most often after surgery (notably cataract surgery), intravitreal injections, or ocular trauma.
- Endogenous Endophthalmitis: Results from organisms spreading to the eye via the bloodstream from a distant infection (e.g., endocarditis, urinary tract infections).
Epidemiology and Incidence
- The rate of endophthalmitis after cataract surgery in developed countries ranges from 0.02% to 0.2%.
- Higher risks are observed in settings with increased ocular trauma, poor surgical hygiene, or immunosuppressed patients.
- Endogenous cases account for 2–15% of all endophthalmitis, with risk amplified in those with diabetes, IV drug use, or chronic illnesses.
Common Pathogens
- Bacterial: Staphylococcus epidermidis, Staphylococcus aureus, Streptococcus species, Gram-negative rods.
- Fungal: Candida, Aspergillus, more common in immunocompromised hosts or after penetrating trauma with plant material.
Key Risk Factors
- Recent intraocular surgery (especially cataract or glaucoma procedures)
- Intravitreal injections (anti-VEGF, corticosteroids)
- Ocular trauma, especially with retained foreign bodies
- Systemic infections (endocarditis, bacteremia)
- Immunocompromised states, diabetes, or chronic corticosteroid use
Symptoms and Signs
- Sudden decrease in vision, eye pain, redness, photophobia, hypopyon (pus in the anterior chamber), and sometimes a milky white pupil.
- Endogenous cases may be subtle and are often mistaken for non-infectious uveitis.
Practical Advice:
If you notice sudden visual decline, pain, or significant redness following eye surgery, trauma, or an injection, seek urgent medical attention—early intervention is critical to preserving sight.
Pharmacological and Conservative Treatments for Endophthalmitis
Rapid Assessment and Initial Steps
Timely diagnosis is crucial, often relying on clinical suspicion, slit lamp, and ocular ultrasound, especially when the fundus cannot be visualized due to opacity.
Empiric Antimicrobial Therapy
- Intravitreal Antibiotics: The mainstay of therapy, providing the highest intraocular concentration. Common regimens include vancomycin (Gram-positive coverage) and ceftazidime (Gram-negative coverage).
- Systemic Antibiotics: More critical in endogenous endophthalmitis or when the infectious source is outside the eye. Choices depend on suspected organisms and host factors.
Adjunctive Therapies
- Topical Antibiotics and Steroids: Supportive, but do not replace intravitreal therapy. Topical steroids may help reduce inflammation, but are usually withheld initially in suspected fungal cases.
- Cycloplegic Agents: Reduce pain from ciliary spasm and help stabilize the blood–ocular barrier.
Antifungal Therapy
- For suspected or confirmed fungal infections, intravitreal amphotericin B or voriconazole is used, often with systemic antifungals like fluconazole or voriconazole.
Observation and Monitoring
- Not every case requires surgery immediately—some less severe post-injection cases can be managed with intravitreal antibiotics and close follow-up.
- Visual improvement or stabilization within 24–48 hours is a good prognostic sign.
Antimicrobial Keywords for SEO:
- intravitreal antibiotics for endophthalmitis
- vancomycin ceftazidime injection for eye infection
- antifungal eye treatment for endophthalmitis
- systemic antibiotics for endogenous endophthalmitis
Practical Advice:
Always complete your course of prescribed antibiotics or antifungals and attend all follow-up appointments—even if symptoms improve—to prevent relapse or complications.
Surgical and Interventional Solutions
While many cases can be managed pharmacologically, certain scenarios demand urgent surgical intervention to prevent irreversible vision loss.
Pars Plana Vitrectomy (PPV)
- Indications: Severe vision loss at presentation, presence of significant vitreous opacities, or lack of improvement with intravitreal therapy.
- Procedure: Removal of the infected vitreous reduces microbial load and inflammation, improves drug penetration, and allows microbiologic diagnosis.
Anterior Chamber Washout
- Indicated for significant hypopyon or anterior chamber fibrin, especially when interfering with visual axis or complicating diagnosis.
Removal of Intraocular Foreign Bodies
- Particularly in traumatic cases; foreign bodies can harbor bacteria or fungi and must be removed promptly.
IOL (Intraocular Lens) and Capsular Bag Removal
- In cases of chronic or recurrent post-surgical endophthalmitis, explantation may be required to eradicate the nidus of infection.
Silicone Oil Injection
- In selected severe cases, silicone oil can be used during vitrectomy to help stabilize the eye, particularly when the retina is at risk.
Surgical SEO Keywords:
- vitrectomy for endophthalmitis
- surgical removal of eye infection
- intraocular lens explantation infection
- silicone oil injection for severe endophthalmitis
Practical Advice:
Discuss with your ophthalmic surgeon the potential need for surgery if there’s no rapid response to drug therapy. Early surgery often leads to better outcomes and vision preservation.
Innovative Research and New Technologies
The management of endophthalmitis is rapidly evolving, thanks to new research and high-tech approaches aimed at earlier detection, improved drug delivery, and enhanced patient outcomes.
1. Advanced Diagnostic Platforms
- PCR-Based Pathogen Identification: Real-time polymerase chain reaction (PCR) and next-generation sequencing are speeding up the detection of causative organisms, enabling more precise, tailored therapy.
- Point-of-Care Diagnostic Kits: New kits offer rapid, bedside identification of pathogens from vitreous samples.
2. Targeted Drug Delivery Systems
- Sustained-Release Intravitreal Implants: Allow for continuous delivery of antibiotics or antifungals directly into the eye, improving therapeutic consistency and reducing the need for repeated injections.
3. Antimicrobial Coatings and Devices
- Intraocular lenses and surgical tools now feature anti-biofilm or antimicrobial coatings, reducing the risk of post-surgical infections.
4. AI-Driven Risk Prediction
- Artificial intelligence models can predict which patients are most at risk for post-operative endophthalmitis, allowing for tailored prophylaxis and closer surveillance.
5. Personalized Medicine in Ocular Infections
- Genetic and microbiome profiling may soon allow for highly individualized therapy, ensuring the right drug for the right patient at the right time.
Innovation SEO Keywords:
- rapid PCR test for endophthalmitis
- sustained-release intravitreal antibiotics
- AI infection risk prediction eye surgery
- antimicrobial intraocular lens innovation
Practical Advice:
If you’re facing eye surgery, ask about the infection-prevention measures used at your center—choosing a facility employing the latest technology can further reduce your risk.
Current Clinical Trials and Future Outlook
Continued research is bringing hope for better outcomes and fewer complications from endophthalmitis.
Ongoing Clinical Trials
- Studies evaluating the efficacy and safety of new antimicrobial agents for intraocular use.
- Trials comparing early vitrectomy versus conservative management for different types of endophthalmitis.
- Research on sustained-release drug implants and their real-world impact on vision and quality of life.
Emerging Directions
- Gene-Editing Therapies: Early-stage research is exploring the potential of CRISPR-Cas systems to target and destroy drug-resistant pathogens within the eye.
- Vaccines: Prophylactic vaccines for at-risk patient populations, such as those undergoing repeated intraocular injections, are in early development.
- Microbiome Modulation: Investigating how manipulation of the ocular surface microbiome may prevent infection or speed recovery.
SEO Keywords for Clinical Trials:
- endophthalmitis clinical trials
- new antibiotics for intraocular infection
- sustained-release drug implant research
- gene therapy for drug-resistant eye infection
Practical Advice:
If you’re eligible for a clinical trial, participation can provide access to cutting-edge care and contribute to breakthroughs that benefit the wider eye care community.
Frequently Asked Questions
What is endophthalmitis and how serious is it?
Endophthalmitis is a severe infection or inflammation inside the eye, usually following surgery, injection, or trauma. It is an ophthalmic emergency that can lead to permanent vision loss without rapid treatment.
How is endophthalmitis diagnosed?
Diagnosis relies on a combination of symptoms, eye examination, and tests like ocular ultrasound or sampling intraocular fluids for culture and PCR to identify the infection.
What are the first steps in treating endophthalmitis?
Urgent injection of broad-spectrum antibiotics or antifungals directly into the eye is standard. Surgery may be needed for severe cases, depending on vision and clinical response.
Can endophthalmitis be prevented after eye surgery?
Careful surgical technique, proper sterilization, and prophylactic antibiotics before and after surgery significantly reduce the risk of developing endophthalmitis.
What is the outlook for patients with endophthalmitis?
Outcomes depend on the speed of intervention, the type of organism involved, and patient factors. Early, aggressive treatment offers the best chance for vision preservation.
Are there new treatments for endophthalmitis?
Recent advances include rapid PCR diagnostics, sustained-release antibiotic implants, antimicrobial device coatings, and personalized medicine approaches.
Disclaimer:
This article is for educational purposes only and should not be considered a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider for personalized care regarding endophthalmitis or any other eye condition.
If you found this guide valuable, please share it on Facebook, X (formerly Twitter), or your preferred platform. Follow us for the latest in eye care, and support our efforts by spreading the word—your advocacy helps others find trustworthy vision health information.






